Fig. 4.1
Schematic drawing of relevant cervical vessels with respective flow patterns on Doppler US, (a) arterial and (b) venous
Rarely target more peripheral vessels (e.g. query vascular malformation, temporal arteritis).
NOTE: For detailed spectral analysis with velocity measurements proper angle correction mandatory, with angle <60°!
4.1.3.4 Cervical Veins
Assessed primarily in axial section, imaging upwards and downwards as far as possible, completed by longitudinal documentation:
Compression manoeuvres (gentle) allow assessing for stiffness and thrombosis.
CDS and spectral analysis for confirmation of initial findings (Fig. 4.1).
NOTE: For any vascular investigation transducer, pressure may cause artefacts that mimic pathology; same applies for wrong patient positioning with bending or kinking of vessels.
4.1.3.5 Intervention
4.2 Normal Findings
4.2.1 Lymph Nodes
Lymph nodes look similar throughout the body – will not be discussed in other chapters.
Typical lymph node locations in neck shown in Fig. 4.2a.
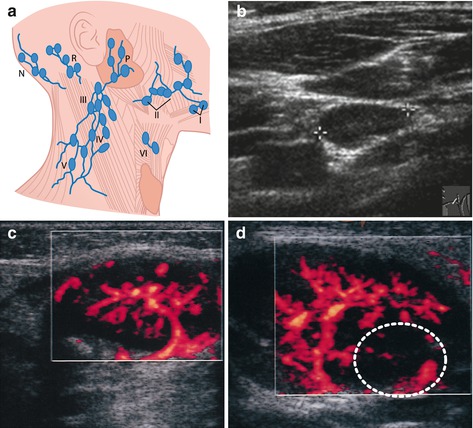
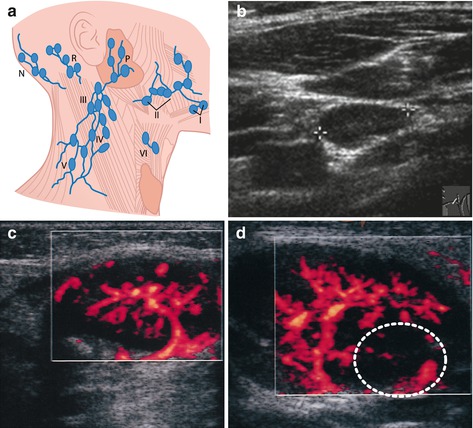
Fig. 4.2
Cervical lymph nodes. (a) Scheme (choose one): typical cervical lymph node regions and distribution. Abbreviations: Level I submandibular space, Level II jugulodigastric space, Level III venous group, Level IV jugular vein nodes, Level V lateral cervical triangle, Level VI prelaryngeal, P parotid, N nuchal group and A extra-/para-auricular group. (b) Gray scale US (+ +), ovaloid, >1 cm, hilar structures. (c) Normal vascular architecture on aCDS (Power Doppler). (d) Spherically enlarged lymph node with focal infiltration (….) depicted by reduced vascularity on aCDS
US Findings
More or less homogeneous structure of low echogenicity with sharp margins and ovoid configuration. Central echogenic hilar structure (Fig. 4.2b):
Usually measure <1 cm diameter, length-to-diameter ratio <0.7.
CDS
Exhibit central/hilar vascular supply with regularly brunching vessels (Fig. 4.2c).
aCDS more sensitive for low flow velocities at high insonation angles – better demonstrates peripheral vasculature (Fig. 4.2d). Helps to depict small peripheral infiltrations even in normal-sized lymph nodes – alternatively ce-US improves detection of focal infiltration/disrupted vascular architecture in future B-flow might further improve potential.
NOTE: These criteria apply to all lymph nodes everywhere throughout the body; normal lymph nodes often seen physiologically.
4.2.2 Cervical Glands
4.2.2.1 Thyroid Gland
Composed of two lobes with central isthmus (Fig. 4.3).
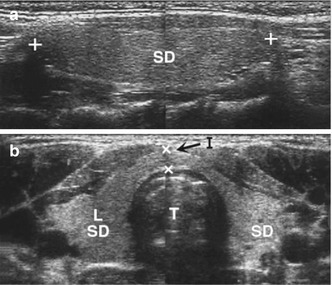
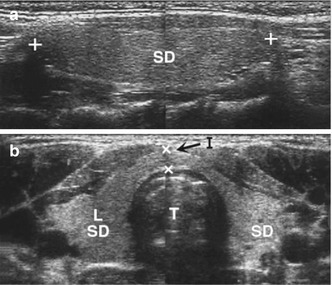
Fig. 4.3
Normal thyroid gland. (a) Longitudinal (length, + +) and (b) axial section, both images using dual image technique. SD = thyroid gland, L = lobe, I = isthmus (→, × ×) and T = trachea
US Findings
Parenchyma of slightly high, but homogenous echogenicity, potentially with tubular anechoic structures representing vessels (particularly in slightly older age).
Echogenicity increases slightly with age.
Anterolateral border convex shaped (concave shape indicates increase in size and may only occur regionally in local infiltration):
Some mild cystic changes and nodular-patchy parenchymal irregularities may normally be present in older children.
Size calculated using ellipsoid equation (L × W × T × 0.48) for each lobe: entire volume = sum of left + right lobe, volume of isthmus negligible in normal thyroid.
NOTE: Thyroid volume changes with age (see respective growth charts) and shows geographic regional variation (depending on iodine supply in water and food, endemic goitre, etc.) (Table4.1). 3DUS more accurate, but new 3DUS-based normal value charts necessary.
Table 4.1
Thyroid US
(a) Normal thyroid size/volume (in Austria): | |
Till 6 years > 4 ml | |
6–10 years 7.1 ± 3.5 ml | |
10–13 years 9.7 + ± 6.6 ml | |
13–15 years 13.0 ± 8.9 ml | |
15–17 years 14.1 ± 10.2 ml | |
Grown-up male < 18 ml | |
Grown-up female < 25 ml | |
(b) Volume calculation of thyroid: | |
 | |
Schematic drawing: how and where to take measurements for volume assessment, with respective age-related graph of normal thyroid volume | |
Note: thyroid size is age, gender and region as well as nutrition dependent | |
Abbreviations: w width, d depth and l length | |
(c) DDx of thyroid lesions | |
Diagnosis | US findings |
Simple cyst | Anechoic, sharp margin, thin wall, no central echoes |
Complicated cyst (regressive, abscess, haemorrhage, etc.) | Cyst with often prominent, irregular or thickened wall, central echoes, potentially septet and levelling |
Adenomatous nodule | Echoic nodule, echo-poor rim-like border |
Adenoma | Focal nodule with sharp margins, usually of higher (seldom less) echogenicity than thyroid parenchyma |
Regressive nodule | Often irregular shape and border and content |
Fibrous nodule | Very low level echostructure, may be part of adenoma, often with calcification |
Tumour (carcinoma, metastasis, lymphoma, etc.) | Nonspecific echostructure, may grow rapidly, often low echogenicity, micro-calcification and some inhomogenicity, unclear and irregular border, may exhibit penetrating-infiltrating behaviour, irregular vascular architecture |
Parathyroid gland and respective adenoma | Usually hypoechoic nodules close to dorsal capsule, or positioned cranially/caudally to thyroid gland |
Sometimes nodular areas up to 1 cm size of low echogenicity depicted – particularly close to outer borders in posterior part of gland – represent parathyroid glands (alternatively positioned next to thyroid gland, then difficult to depict particularly in infants).
aCDS
For demonstration of vascular architecture, vessel identification (DDx cysts) or displacement (as seen in tumours).
Necessary for judging (hyper)vascularisation (e.g. in hyperthyroidism or thyroiditis) and focal vessel disruption/aneurysm (trauma).
4.2.2.2 Parotid, Submandibular and Sublingual Glands
US Findings
Parotid gland: slightly patchy, somewhat inhomogenous, echogenic parenchyma with lobules and hilar vascular supply (Fig. 4.4). Parotid duct only visible if enlarged, particularly in children:
Fig. 4.4
Glands and tonsils. Normal parotid gland, note the normal slightly prominent hypoechoic, nodular-shaped tonsil below the echogenic triangular gland as often observed in infants and children, adjacent normal homogenously echogenic tongue
Assessment of duct continuity is difficult/impossible.
Submandibular/sublingual gland: echogenicity similar to parotid, but without lobules, potentially less patchy. Hilar structures less prominent than in parotid. Ducts usually not identified. Vessels depictable by aCDS.
4.2.3 Other Cervical Soft Tissues
4.2.3.2 Tonsils
Usually seen as hypoechoic lobulated nodular structures in respective location and may show echogenic bands representing air-filled crypts or vessels (see Fig. 4.4).
Physiologically often prominent in childhood.
Tree-shaped or stripe-like vascular architecture on CDS.
4.2.3.3 Tongue
Nicely seen from submental access and best in axial section.
Has homogeneous structure of muscle-like appearance, potentially with some slightly higher echogenicity than muscles elsewhere.
4.2.3.4 Para- and Retropharyngeal Spaces
Only meaningfully assessable in case of pathology, such as parapharyngeal abscess or paravertebral tumour. Otherwise not a routine target of US investigation, retropharyngeal space is difficult to visualise.
4.2.3.5 Larynx
Especially in infant/younger children, laryngeal US often difficult due to limited patient cooperation.
Cartilaginous structures nicely assessable – helpful for assessing congenital malformations (e.g. cysts, haemangioma), posttraumatic changes (e.g. haematoma of vocal cord) and similar queries (Fig. 4.5).
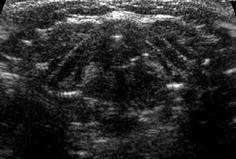
Fig. 4.5
Larynx US. Normal US appearance of yet non-ossified larynx
NOTE: It is important to know age-dependent anatomic appearance (varies with progressive calcification).
4.2.4 Cervical Vessels
Normal anatomy with respective US and Doppler findings of major vessels shown in Fig. 4.1.
US Findings:
Vessel – anechoic tubular structure
Artery – multilayered thick wall.
Vein – usually thin wall, valves may be visible and more easily compressible:
Veins show significant variation in diameter depending on respiratory cycle and intrathoracic/transducer pressure – used for assessing patency.
NOTE: Physiologic venous ectasia may be present, particularly during valsalva manoeuvre.
CDS (Fig. 4.6)
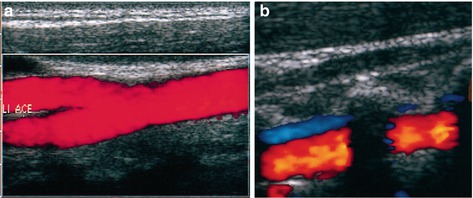
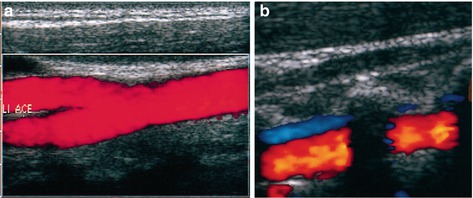
Fig. 4.6
Cervical vessels. Anatomy + typical US appearance of carotid artery (a) using aCDS and the vertebral artery with accompanying vein (b) on CDS (note shadowing from transverse process of cervical vertebra)
In arteries – biphasic unidirectional flow towards head.
In (jugular) veins – usually three-phase modulated flow, inspiratory and expiratory velocity variations can be bidirectional.
Spectral Analysis
Essential – typical flow patterns can be demonstrated in individual arteries (see Fig. 4.1):
CCA – intermediate resistive flow pattern, relatively low antegrade diastolic velocity and RI = 0.7–0.9.
ICA – low-resistant flow pattern, higher diastolic velocity and RI = 0.6–0.7.
ECA – flow profile resembles any peripheral high-resistance vessel with low, potentially missing or inverted end-diastolic flow, RI = 0.9–1.1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree