Case presentation
A 13-year-old female presents with acute onset of right lower quadrant pain for the past 4 hours. She states that she has been in her usual, normal state of health and was “just walking down the street” when she experienced the pain, which was accompanied by nausea and she has had three episodes of nonbilious/nonbloody emesis. She states that after the emesis, she feels “a little better” but the pain has persisted. She denies fever, diarrhea, or trauma. She denies being sexually active and there is no history of vaginal bleeding or discharge. She began her menses 2 years ago and has had occasional cramping with her menstrual cycle; her last menstrual period was 2 weeks ago.
Physical examination reveals a slightly uncomfortable-appearing patient, complaining of abdominal pain, mostly in the right lower quadrant. She is afebrile, and aside from mild tachycardia (a heart rate of 120 beats per minute), the vital signs are unremarkable. She has mild tenderness to palpation of the right lower quadrant and suprapubic areas; there is no rebound or guarding. She has no palpable abdominal masses and there is no abdominal distention; a urine pregnancy test is negative.
Imaging considerations
Prior to imaging, a pregnancy test must be obtained, since this can assist the clinician in considering an appropriate imaging modality selection to evaluate nongynecologic and gynecologic causes of abdominal pain and to avoid fetal exposure to ionizing radiation. The American College of Radiology (ACR) has Appropriateness Criteria® (AC) useful for selecting among various imaging modalities for the evaluation of female acute pelvic pain in the reproductive age group, based on gynecologic and nongynecologic suspected etiologies and whether the patient is pregnant or not. As the patient had a negative serum pregnancy test, Variant 2 of the AC for “gynecological etiology suspected, serum β-hCG negative” applies ( Table 23.1 ). The ACR Appropriateness Criteria® content is updated regularly and users should go to the website ( https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria® ) to access the most current and complete version of the AC.
Plain radiography
While plain radiography of the abdomen may be utilized in cases of abdominal pain, it is not indicated as a first-line imaging study in patients who have suspected ovarian pathology as a source of their pain.
Ultrasound (US)
Readily available and without ionizing radiation exposure, US is an excellent means by which to visualize the ovary and surrounding structures. This is the first-line imaging modality for cases of suspected ovarian torsion or other gynecologic pathology where imaging is indicated.
A mid- to high-frequency curvilinear transducer is used and the bladder is used as a sonographic window and therefore must be full to obtain meaningful results. In pediatric patients, a transabdominal approach is usually employed, although in select patients such as sexually active adolescents, a transvaginal technique may be utilized. The clinician should be aware of local statutes regarding informed consent for performing a transvaginal US, which vary among jurisdictions. The decision to perform transvaginal US should be based on sexual and clinical history, and age of the patient. The preference of the patient, parent/guardian, and physician are factors in the decision to utilize a transvaginal approach and informed consent for the procedure should be obtained. The patient should also be made aware that the study can be stopped at any time, if the patient wishes. Clinicians may utilize institutional protocols if they are available.
Suggested transabdominal technique includes the following :
- ■
A scout scan of the entire pelvis in two planes, making sure the bladder is full.
- ■
Low-frequency color Doppler use to ensure proper penetration.
- ■
Imaging the uterus in two planes, with uterine volume.
- ■
Measuring the anteroposterior thickness of the endometrium in the midsagittal plane and color Doppler assessment of the endometrium, looking for endometrial lesions.
- ■
Measurement of the ovaries in three orthogonal planes with calculation of the ovarian volume.
- ■
Other organ assessment (appendix, kidneys, bowel wall) as clinically indicated.
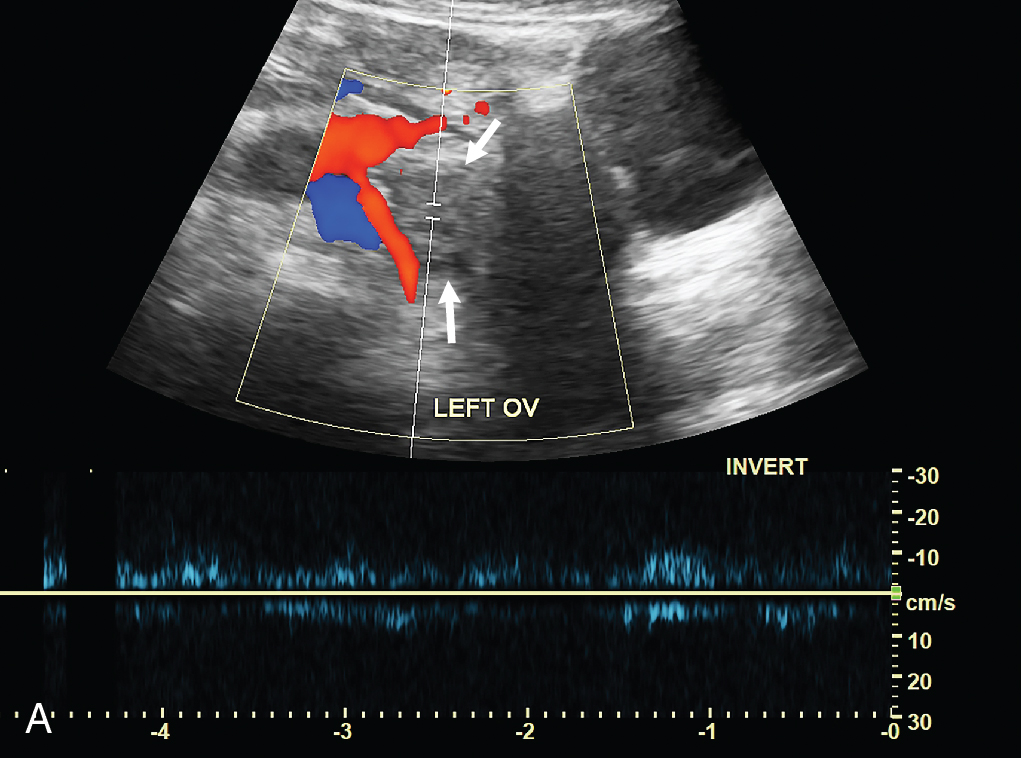
Doppler sonography has been the traditional imaging method to evaluate for the presence of ovarian torsion, since both venous and arterial flow can be compromised during this process. A lack of normal blood flow is suspicious for ovarian torsion. Abnormal blood flow has modest accuracy for identifying ovarian torsion and while abnormal arterial blood flow is often a concern, abnormal venous blood flow is seen earlier in ovarian torsion. , The presence of arterial blood flow to the ovary does not exclude ovarian torsion, due to secondary ovarian vascular supply, and does not rule out intermittent, or even partial torsion. Other findings should be considered, such as the size and morphology of the affected ovary (compared to the unaffected ovary), venous blood flow, the presence of free fluid, or ovarian masses. Ovarian enlargement is particularly concerning for torsion, and lack of venous blood flow is a frequent finding with ovarian torsion. , A number of studies confirm cases of proven ovarian torsion where patients have either an enlarged ovary or lack of venous blood flow despite having arterial blood flow by Doppler sonography. , , , , , Combining abnormal findings, particularly ovarian enlargement and the presence of free fluid, increases the sensitivity of sonography to detect ovarian torsion. , , , , Detection of the twisting of the vascular pedicle—the “Whirlpool Sign”—demonstrated as a round hyperechoic structure with concentric hypoechoic stripes or as a tubular structure with internal heterogeneous echoes, suggests ovarian torsion. Sensitivities and specificities for various US findings for ovarian torsion have been reported , :
| ULTRASOUND FINDING | SENSITIVITY a | SPECIFICITY a |
| Tissue edema | 21% | 100% |
| Absence of intraovarian vascularity | 52% | 91% |
| Absence of arterial flow | 76% | 99% |
| Absence or abnormal venous flow | 100% | 97% |
a These values represent upper estimates and may be lower based on the skill of the providers performing and interpreting the test.
US can also detect other gynecologic entities that may mimic symptoms of ovarian torsion, including ovarian (simple, complex, and hemorrhagic) cysts, tubo-ovarian abscesses, and ovarian masses, as well as nongynecologic etiologies, such as appendicitis. ,
US is the diagnostic imaging modality of choice for all patients when ovarian torsion is suspected, but the presence of arterial flow by Doppler alone cannot be solely and exclusively relied upon to exclude this condition in patients whose symptoms and exam are consistent with ovarian torsion. The clinician should also consider the history, clinical exam, and other ovarian US findings when interpreting sonography results.
Computed tomography (CT)
Computed tomography is utilized frequently during the evaluation of abdominal pain. With pediatric patients, ALARA (as low as reasonably achievable) principles should be practiced.
There are no well-defined CT criteria for ovarian torsion, but there are findings that suggest this process. Ovarian enlargement, pelvic free fluid, a twisted vascular pedicle, inflammatory fat stranding, and deviation of the uterus to the side of the torsion have been reported CT findings in patients with proven ovarian torsion. , , , Some studies have proposed that a well-visualized, normal-appearing ovary on CT can exclude torsion; in these studies, patients with proven ovarian torsion had abnormalities on imaging, including an enlarged ovary, free pelvic fluid, abnormal ovarian enhancement, uterine deviation, and a twisted pedicle. , Notably, there are findings on CT that can mimic ovarian torsion, including ectopic pregnancy, endometriosis, hemorrhagic functional cyst, or tumors.
While CT is not a first-line imaging modality to investigate ovarian torsion and should not be solely relied upon to exclude this diagnosis, a normal CT scan appears to make torsion less likely. This modality may be useful if US findings are equivocal or indeterminant, but suspicious, for torsion or if nongynecologic pathology such as appendicitis is suspected. , , , , However, if available, magnetic resonance imaging (MRI) with intravenous (IV) contrast is preferred over CT as the second-line imaging modality for gynecologic pathology including ovarian torsion, if sonography is nondiagnostic. This is promulgated by the ACR Appropriateness Criteria®—Variant 2.
Magnetic resonance imaging
While also not a first-line imaging modality for ovarian torsion, MRI is excellent at visualizing Mullerian structures and the ovaries. , Findings on MRI suggestive of torsion are similar to those seen with CT: ovarian enlargement, masses (well visualized on T2 weighted images), twisted pedicles, and free fluid (to which MRI is very sensitive). , , Although used infrequently for ovarian torsion, MRI is the study of choice for gynecologic pathology, including ovarian torsion, after an inconclusive pelvic sonogram. MRI is especially useful if the diagnosis of ovarian torsion is suspected in a pediatric patient, a pregnant patient, patients with renal failure, or patients with severe IV contrast allergies when a secondary imaging test is needed to clarify US results.
Imaging findings
While IV access was established, pediatric surgical consultation was obtained. The patient appeared improved on examination, although still with pain. A request was made for a transabdominal pelvic US. The need for a full urinary bladder was discussed at length with the patient and her parents; they did not consent to the placement of a urinary catheter. Rather, several normal saline boluses were given, and the patient, after the second bolus, stated she felt a strong urge to urinate, at which time the US was obtained. Selected images from that study are presented here. The right ovary is enlarged, and ovarian parenchyma is diffusely heterogeneous with a prominent cyst or follicle and a few peripherally arranged small follicles. The right ovary appears to be shifted toward the midline of the pelvis and Doppler evaluation showed no convincing arterial or venous flow in the right ovary; comparison is made to the left ovary ( Figs. 23.1–23.4 ).