This article summarizes the updates and revisions to the second edition of the BI-RADS MRI lexicon. A new feature in the lexicon is background parenchymal enhancement and its descriptors. Another major focus is on revised terminology for masses and non-mass enhancement. A section on breast implants and associated lexicon terms has also been added. Because diagnostic breast imaging increasingly includes multimodality evaluation, the new edition of the lexicon also contains revised recommendations for combined reporting with mammography and ultrasound if these modalities are included as comparison, and clarification on the use of final assessment categories in MR imaging.
Key points
- •
The BI-RADS lexicon has improved the consistency of breast MR imaging interpretation and reporting.
- •
New revisions of the MRI Lexicon serve to further clarify breast MR imaging reporting, improve lesion diagnosis and management, and facilitate patient care.
- •
As diagnostic breast imaging increasingly includes multimodality evaluation, the new edition of the lexicon also contains revised recommendations for combined reporting with mammography and ultrasound if these modalities are included as comparison, and clarification on the use of final assessment categories in MR imaging.
Introduction
The American College of Radiology (ACR) developed the Breast Imaging Reporting and Data System (BI-RADS) mammography lexicon in 1993 to standardize and improve mammography interpretation and reporting. Subsequently, a lexicon for breast magnetic resonance (MR) imaging was developed to enable comparison of findings from study to study in the literature and to provide a more consistent approach for communicating findings to referring physicians, patients, and scientists alike.
Investigations of the normal breast and breast pathologic abnormality on MR imaging have advanced the understanding of the appearance of the breast in physiologic and diseased states. Advances and improvements in breast MR imaging hardware and software development have allowed higher spatial resolution and faster temporal scanning, with improved visualization of MR imaging findings. The MRI BI-RADS lexicon has been revised accordingly, with new terminology added to improve the description of lesions seen on current pulse sequences, and removal of terms that were infrequently used. In addition, the MRI BI-RADS lexicon underwent concurrent revision with the Mammography and Ultrasound Lexicons, with the aim of providing more consistency of terms across each modality-specific lexicon. The new ACR BI-RADS Atlas contains all 3 newly revised lexicons.
This article summarizes the updates and revisions to the second edition of the BI-RADS MRI lexicon ( Box 1 ). A new feature in the lexicon is background parenchymal enhancement and its descriptors. Another major focus is on revised terminology for masses and non-mass enhancement. A section on breast implants and associated lexicon terms has also been added. As diagnostic breast imaging increasingly includes multimodality evaluation, the new edition of the lexicon also contains revised recommendations for combined reporting with mammography and ultrasound, and clarification on the use of final assessment categories in MR imaging. Note the lexicon is still undergoing revision and the final version of the lexicon should be reviewed for a complete compilation of the revisions in their entirety.
| Imaging Findings | Update |
|---|---|
| Background parenchymal enhancement | New imaging finding |
| Lesion types | |
| Masses | New and omitted terms |
| Non-mass-like enhancement | New and omitted terms |
| Associated findings | |
| Implants | New section and terms |
| Assessment and categories | |
| BI-RADS 0 | Usage clarified |
| BI-RADS 4 | Usage clarified |
Introduction
The American College of Radiology (ACR) developed the Breast Imaging Reporting and Data System (BI-RADS) mammography lexicon in 1993 to standardize and improve mammography interpretation and reporting. Subsequently, a lexicon for breast magnetic resonance (MR) imaging was developed to enable comparison of findings from study to study in the literature and to provide a more consistent approach for communicating findings to referring physicians, patients, and scientists alike.
Investigations of the normal breast and breast pathologic abnormality on MR imaging have advanced the understanding of the appearance of the breast in physiologic and diseased states. Advances and improvements in breast MR imaging hardware and software development have allowed higher spatial resolution and faster temporal scanning, with improved visualization of MR imaging findings. The MRI BI-RADS lexicon has been revised accordingly, with new terminology added to improve the description of lesions seen on current pulse sequences, and removal of terms that were infrequently used. In addition, the MRI BI-RADS lexicon underwent concurrent revision with the Mammography and Ultrasound Lexicons, with the aim of providing more consistency of terms across each modality-specific lexicon. The new ACR BI-RADS Atlas contains all 3 newly revised lexicons.
This article summarizes the updates and revisions to the second edition of the BI-RADS MRI lexicon ( Box 1 ). A new feature in the lexicon is background parenchymal enhancement and its descriptors. Another major focus is on revised terminology for masses and non-mass enhancement. A section on breast implants and associated lexicon terms has also been added. As diagnostic breast imaging increasingly includes multimodality evaluation, the new edition of the lexicon also contains revised recommendations for combined reporting with mammography and ultrasound, and clarification on the use of final assessment categories in MR imaging. Note the lexicon is still undergoing revision and the final version of the lexicon should be reviewed for a complete compilation of the revisions in their entirety.
| Imaging Findings | Update |
|---|---|
| Background parenchymal enhancement | New imaging finding |
| Lesion types | |
| Masses | New and omitted terms |
| Non-mass-like enhancement | New and omitted terms |
| Associated findings | |
| Implants | New section and terms |
| Assessment and categories | |
| BI-RADS 0 | Usage clarified |
| BI-RADS 4 | Usage clarified |
Technique
There is a new section on technical parameters, which are important for obtaining high-quality breast MR images and for examination interpretation. A brief discussion related to reporting technique is included here.
Revised acquisition reporting recommendations include description of key elements of image acquisition, contrast administration, and postprocessing. Recommendations include comments on whether a dedicated breast coil was used, pulse sequence techniques obtained, such as T1-weighting or T2-weighting, and whether fat suppression was applied. It is recommended that a T2-weighted or fluid-specific sequence be obtained before the administration of intravenous contrast, as this has been shown to help identify lymph nodes, fluid, and other findings.
The new lexicon mentions both diffusion-weighted imaging and magnetic resonance spectroscopy, which are still considered investigational. Reporting recommendations to include clinical history and comparison examinations are unchanged.
Background parenchymal enhancement
Although previously introduced as a concept and sporadically used in breast MR imaging reporting, background parenchymal enhancement (BPE) is a newly formalized BI-RADS feature to be recognized and described in the breast MR imaging report.
Categories of BPE are based on both the amount and the degree of normal parenchymal tissue enhancement on the first contrast-enhanced MR imaging sequence. BPE is described as none, minimal, mild, moderate, and marked ( Fig. 1 ). It is important to note that the amount of background parenchymal enhancement on MR imaging is not correlated with the amount of mammographically visible fibroglandular tissue. For example, mammographically dense breasts may have no or minimal BPE, whereas breasts with scattered fibroglandular parenchymal tissue may have marked BPE. Although mammographic glandular tissue patterns do not have a direct association with BPE, women with heterogeneously dense or dense glandular tissue have been found to have significantly more BPE than women with fatty or scattered fibroglandular tissue.
The detection of malignancy by MR imaging is based on the angiogenic properties of tumors, including increased blood flow, neovascularity, and capillary leakiness. Although it is hypothesized that greater BPE may negatively influence breast MR imaging performance, either by decreasing the MR imaging sensitivity, similar to the way in which increased mammographic density decreases mammographic sensitivity, or by decreasing specificity caused by potential overlap in appearance with benign findings on MR imaging, current evidence from the literature to date demonstrates no adverse impact from BPE on the diagnostic accuracy of breast MR imaging. Two retrospective studies of BPE found no significant difference in cancer detection between women with minimal/mild versus moderate/marked BPE. Furthermore, DeMartini and colleagues showed no significant difference in positive rate of biopsy, cancer yield, or specificity between women with minimal/mild BPE compared with moderate/marked BPE. However, both studies also reported that greater BPE was associated with a higher rate of abnormal interpretation and probably benign findings (BI-RADS 3 final assessment), with Hambly and colleagues noting that the most common finding (78%) to be given a BI-RADS 3 assessment was diffuse background parenchymal enhancement.
BPE has a spectrum of patterns, ranging from focal and nodular to diffuse, which is predominantly mediated by hormonal fluctuation and can vary depending on menstrual cycle phase, hormone replacement therapy, and lactation. Premenopausal women tend to have more background parenchymal enhancement than postmenopausal women, with the degree of enhancement related to estrogen-induced vascular permeability. Progesterone is thought to balance and counteract estrogen-induced microvessel permeability, decreasing background parenchymal enhancement. Similarly, anti-estrogen tamoxifen therapy is also associated with decreased BPE. For these reasons, optimal timing of a breast MR imaging examination is at the nadir of estrogen effects, during days 7 to 10 of the menstrual cycle.
Lesion analysis—morphology
A “lesion” on contrast-enhanced breast MR imaging is a unique enhancing entity seen on the first postcontrast sequence that is clearly different from the BPE. The lexicon identifies 3 lesion types: foci, masses, and non-mass enhancement. Lesion characteristics to be described and considered when making a final assessment include both morphology and enhancement kinetics. Because of underlying breast cancer neoangiogenesis, breast cancer tends to demonstrate earlier enhancement relative to background enhancement. Thus, lesion morphology characteristics are generally best evaluated on postcontrast images obtained within the first 3 minutes following intravenous contrast administration. In the revised lexicon, the recommendations that both morphology and enhancement kinetics are important for lesion analysis are unchanged.
Foci
A focus of enhancement is less than 5 mm in size and in general is so small that it cannot be otherwise characterized. Usually, the shape and margins cannot be visualized clearly enough to be described. The definition of an enhancing focus is unchanged in the revised lexicon. If there are multiple bilateral enhancing foci such as those commonly seen as part of background parenchymal enhancement, those foci could be included in the reporting of the BPE and need not be described further.
Masses
Breast masses are space-occupying three-dimensional lesions that are greater than 5 mm in size and have distinct shapes, margins, and internal enhancement characteristics. Masses should be evaluated on both precontrast and postcontrast scans, T1-weighted and T2-weighted pulse sequences and viewed in both axial and sagittal planes to evaluate both shapes and margins. Mass descriptions may be affected by scan parameters such as slice thickness or other technical factors related to in-plane spatial resolution.
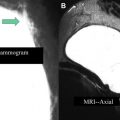
Mass shape descriptors are round, oval, or irregular. Round lesions are spherical in shape. In the revised lexicon, “oval” replaces “lobulated” as a shape descriptor and now includes masses with up to 3 gentle lobulations ( Box 2 , Fig. 2 A). “Irregular” shapes are uneven and not round nor oval. Previously used to describe either shape or margin, the term “irregular” in the revised lexicon will be a combined descriptor used for both mass shape and margin (see Fig. 2 B).
| BI-RADS Lexicon Term | Update |
|---|---|
| Irregular | Now a combined shape/margin descriptor |
| Oval | Replaces Lobulated as a shape descriptor |
| Circumscribed | Replaces Smooth as a margin descriptor |
| Enhancing internal septations | Removed due to underutilization |
| Central enhancement | Removed due to underutilization |
| Signal intensity on noncontrast T2-weighted images | New feature |
Mass margin descriptors are described as circumscribed, irregular, or spiculated. In the revised lexicon, “circumscribed” replaces “smooth” as a margin descriptor (see Fig. 2 A). As noted above, the term “irregular” in the revised lexicon will be a combined descriptor of both shape and margin. Spiculated margins, as with mammography, are characterized by radiating lines.
Mass internal enhancement patterns include homogeneous, heterogeneous, rim enhancement, or dark internal septations. Homogeneous enhancement is uniform and consistent throughout the mass, while heterogeneous enhancement is nonuniform and variable within the mass. Rim enhancement can be identified at the periphery of a mass, and dark internal septations are nonenhancing linear areas on postcontrast images. Because of underutilization, the terms “enhancing internal septation” and “central enhancement” have been removed from the lexicon.
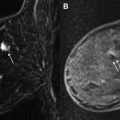
A new mass feature in the revised lexicon is the T2-weighted signal intensity on noncontrast images. It has been reported that increased T2 signal intensity is associated with benign findings such as intramammary lymph nodes and fibroadenomas ( Fig. 3 ). However, although associated with some benign lesions, increased T2 signal intensity has also been identified with some breast cancers, particularly the mucinous subtype. Thus, it is important to evaluate all lesion characteristics before making a final assessment.