CHAPTER 9 Upper extremity arteries
Arteriography (video 9-1)
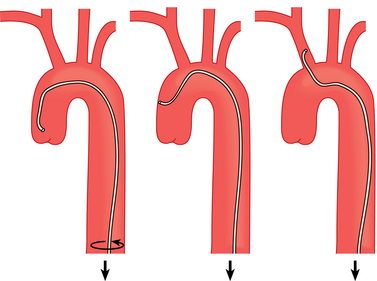
The brachiocephalic, left carotid, and left subclavian arteries are catheterized from a common femoral artery approach with a 4- or 5-French (Fr) vertebral or headhunter catheter. The catheter is advanced over a guidewire into the ascending thoracic aorta and then simultaneously torqued and withdrawn at the groin until the tip engages the artery of interest (Fig. 9-1). In older patients with ectasia of the aorta and arch vessels, a reverse-curve catheter may be useful (Fig. 9-2). When atherosclerotic disease is present, gentle catheter manipulations are essential to avoid dislodging aortic plaque fragments into the brain or periphery. Even minute air bubbles or clots released during catheterization of arch vessels and their branches may cause a stroke (through the carotid or vertebral arteries) or paraplegia (e.g., through spinal branches of the costocervical artery.) Therefore meticulous double flushing with uncontaminated saline is done every 60 to 90 seconds if blood can be aspirated from the catheter.
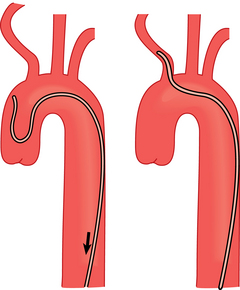
Figure 9-2 Steps in catheterization of a tortuous brachiocephalic artery with a Simmons catheter.
(Adapted from Kadir S. Diagnostic angiography. Philadelphia: WB Saunders; 1986: p.178.)
In some instances, arteriography of the forearm and hand is accomplished by direct antegrade brachial artery puncture (see Chapter 3). For example, this approach is useful to evaluate the anastomosis of a dialysis fistula that is not easily accessible directly from the access itself.
Anatomy (online cases 3 and 17)
Development
In early gestation, the upper limbs are nourished by the axial artery. This vessel evolves into the axillary, brachial, interosseous, and median arteries that feed the hand in the fetus.1 The ulnar artery is an outgrowth of the brachial artery at the elbow. The radial artery arises from a superficial branch of the proximal brachial artery, but its origin migrates toward the elbow as the fetus grows. In most cases, the distal interosseous and median arteries regress before birth.
Normal anatomy
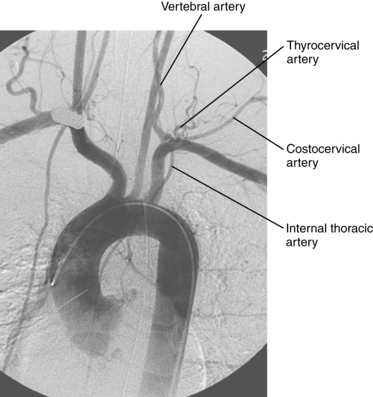
The subclavian arteries originate from the brachiocephalic (innominate) artery on the right and directly from the aortic arch on the left2 (Fig. 9-3). The artery runs posterior to the subclavian vein and the anterior scalene muscle. It arches over the pulmonary apex within the costoclavicular space surrounded by nerves of the brachial plexus. The subclavian artery has several major branches (Fig. 9-4):
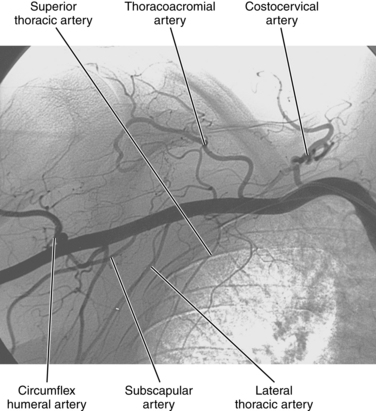
At the outer edge of the first rib, the subclavian artery becomes the axillary artery (see Fig. 9-4). The vessel runs deep to the pectoralis major and minor muscles and lateral to the axillary vein. Its major branches include the superior thoracic, thoracoacromial, lateral thoracic, subscapular, and anterior and posterior humeral circumflex arteries. These branches supply muscles of the shoulder girdle, humerus, scapula, and chest wall.
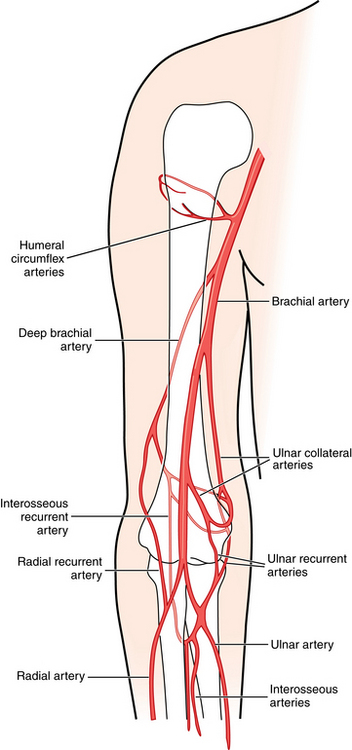
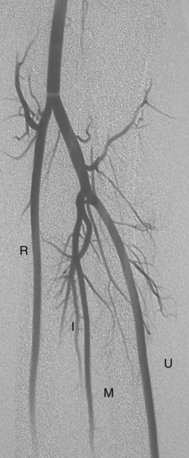
At the lateral edge of the teres major muscle (approximately the lateral scapular border), the axillary artery becomes the brachial artery. In the mid-upper arm, the artery lies in a fascial sheath along with the basilic vein, paired brachial veins, and the median and ulnar nerves. Its major branches include the deep brachial and the superior and inferior ulnar collateral arteries (Fig. 9-6). At about the level of the radial head, the brachial artery divides into the radial and ulnar arteries (Fig. 9-7). The radial artery obviously descends on the radial side of the forearm. The ulnar artery, which is usually the larger of the two, gives off the common interosseous artery and then descends on the ulnar side of the forearm. The interosseous artery divides into anterior and posterior branches separated by the interosseous membrane. In less than 10% of individuals, the anterior interosseous or median artery persists and contributes to the palmar arch.3
The arterial anatomy of the hand is extremely variable, and deviations from the classic pattern described here are common.3,4 The ulnar artery supplies the superficial palmar arch, and the radial artery supplies the deep palmar arch (Figs. 9-8 and 9-9). The arches often are in continuity with the opposing forearm artery through small branches at the wrist. The superficial arch is dominant and typically forms distal to the deep arch. The princeps pollicis and radialis indicis arteries arise from the radial artery and supply the thumb and index finger, respectively. The superficial palmar arch gives off three or four common palmar digital arteries, and the deep arch gives off the palmar metacarpal arteries. At the bases of the proximal phalanges, adjacent metacarpal vessels from each arch merge and then immediately divide into proper digital arteries, which supply apposing surfaces of the fingers. A so-called incomplete superficial arch, defined by lack of continuity of the radial artery with the superficial arch and lack of supply of the thumb and medial index finger by the ulnar artery, is found in about 14% to 20% of the population in autopsy studies.3,4
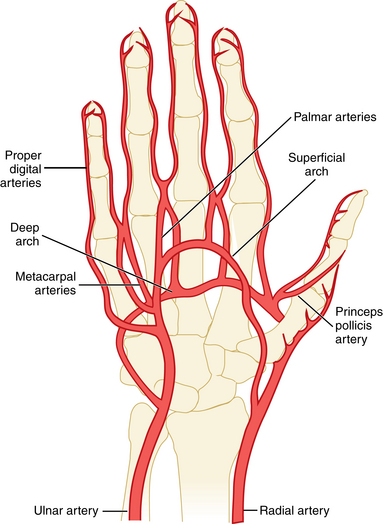
Figure 9-8 Arterial anatomy of the hand.
(Adapted from Loring LA, Hallisey MJ. Arteriography and interventional therapy for diseases of the hand. Radiographics 1995;15:1299.)
Variant anatomy
Anomalies of the subclavian artery origin are discussed in Chapter 6. In about one third of the population, the superficial cervical and dorsal scapular arteries have a common origin from the thyrocervical artery (i.e., transverse cervical artery). Variations in muscular branches of the axillary or brachial artery are common but do not have much clinical relevance.5,6
“High” origin of the radial artery from the axillary or upper brachial artery is an important variant (Fig. 9-10). This anomaly results when the radial artery origin fails to migrate distally toward the elbow during gestation. It was found in 14% of cases in one autopsy series.6 A high origin of the ulnar artery is far less common. Duplications of the brachial artery and hypoplasia or aplasia of the radial and ulnar arteries are rare variants.
The persistent median artery reflects lack of regression of the embryonic median branch of the common interosseous artery (Fig. 9-11). It was identified in 3.4% of cases in one large operative series.7 This vessel may supply a palmar arch.
Collateral circulation
In proximal brachial artery obstruction, the subscapular and posterior humeral circumflex arteries provide flow through muscular branches into the distal brachial or forearm arteries2 (see Fig. 9-6). In cases of midbrachial artery occlusion, the deep brachial artery and superior ulnar collateral arteries supply the radial recurrent and ulnar recurrent arteries, respectively, above the elbow. The radial and ulnar recurrent arteries are the chief pathways across the elbow in patients with distal brachial artery occlusions.
Major disorders
Acute upper extremity ischemia (online case 64)
Etiology
Acute ischemia is far less common in the arm than in the leg. This disparity is partially explained by the extensive collateral network around the scapula and shoulder and by the smaller muscle mass and metabolic needs of the arm. Emboli account for about 50% of cases of acute arterial occlusion, and most come from the heart8–10 (Box 9-1). About one fourth of cases result from iatrogenic or accidental trauma leading to arterial thrombosis. In the remainder, acute thrombosis is caused by superimposed atherosclerotic plaque, local extrinsic disease (e.g., thoracic outlet syndrome), aneurysm, or arteritis.
Clinical features
Most embolic occlusions occur in older patients with a history of cardiac dysrhythmias, myocardial infarction, or valvular heart disease. Sudden and complete upper extremity arterial obstruction causes abrupt onset of arm pain, coolness, cyanosis, pallor, diminished or absent pulses, and, occasionally, sensorimotor deficits. However, some patients are only mildly symptomatic if the underlying disease is chronic (as with thrombosis at a site of preexisting atherosclerotic stenosis) and collateral circulation is robust. The presence of arm swelling should raise the suspicion of severe venous thrombosis (see Chapter 17).
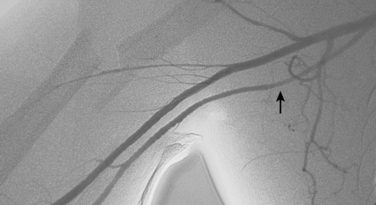
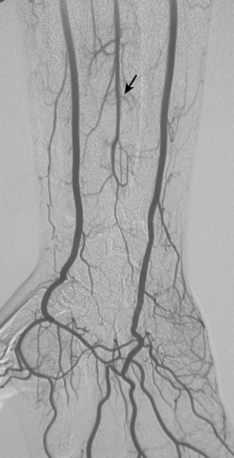
Imaging
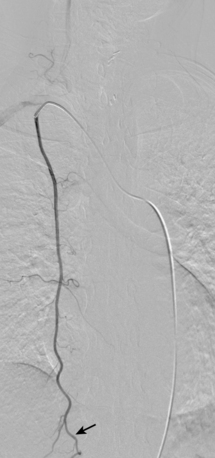
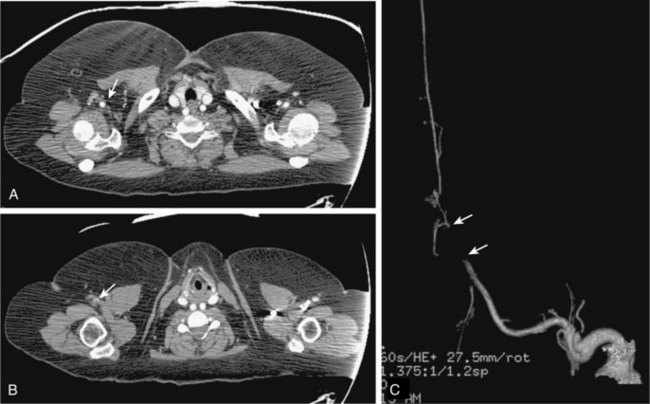
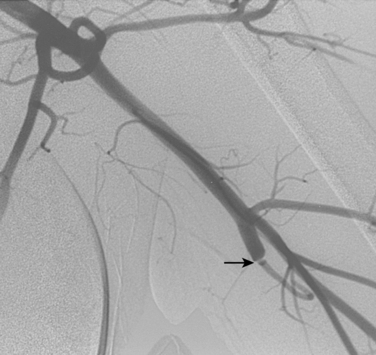
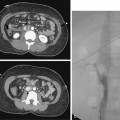
Duplex sonography, computed tomography (CT) angiography, and magnetic resonance (MR) angiography are sometimes used in the initial evaluation of patients who do not go directly for operation11–13 (Fig. 9-12). Catheter angiography is usually reserved for cases in which endovascular treatment is planned. It is customary to investigate the entire circulation from the aortic arch to the digital arteries of the hand to identify potential sources of emboli and to search for occult distal disease. An acute embolus produces a discrete filling defect with reconstitution of the distal vessels. However, it also may appear as a sharp cutoff that mimics a thrombotic occlusion (Fig. 9-13). After the embolic event occurs, clot propagates proximally and distally to the next large collateral branches. Post-traumatic thrombosis results in an abrupt occlusion at or near the site of injury (Fig. 9-14).
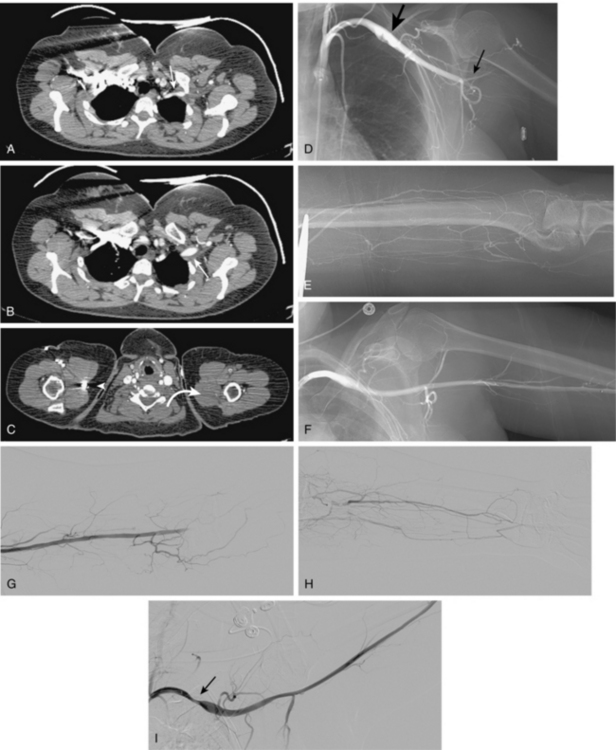
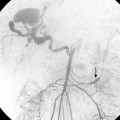
Figure 9-13 Embolus to the left brachial artery in a patient with thoracic outlet syndrome. A through C, Contrast-enhanced computed tomography images show left subclavian artery (arrow) abutting callus from an old clavicular fracture with post-stenotic dilation of the artery (arrow). Unlike the right brachial artery (arrowhead), the mid left brachial artery is thrombosed (curved arrow). D, Left subclavian arteriogram shows mural thrombus within the dilated segment of the left subclavian artery (large arrow) and complete occlusion of the proximal left brachial artery (small arrow).E, Weak collateral flow is found in the upper arm. F, Following overnight thrombolysis with t-PA at 1 mg/hr, the proximal occlusion is completely gone. Flow is noted to the distal left brachial artery (G), with collateral filling of forearm arteries (H). I, With the left arm in extreme abduction, narrowing of the subclavian artery is noted (arrow).
Treatment
Blood flow to the arm must be restored promptly (within about 4 to 6 hours after acute occlusion in the absence of preexisting collateral circulation) to avoid ischemic peripheral neuropathy, irreversible muscle necrosis, and (ultimately) amputation.14
Surgical therapy
Anticoagulation and embolectomy with a Fogarty catheter are standard treatment for embolic occlusions.8–10,15 If the symptoms are mild and the clot burden is small, the patient can sometimes be managed with anticoagulation alone. Thrombotic occlusions are repaired by direct thrombectomy, patch revision, or bypass grafting.
Endovascular therapy
Thrombolysis is an attractive alternative to surgery for some acute upper extremity arterial occlusions.16,17 Acute embolic occlusions are very responsive to enzymatic thrombolysis, which achieves complete or near-complete clot lysis and limb salvage in many cases18,19 (see Fig. 9-13). Techniques for extremity arterial thrombolysis are considered in Chapter 3. Liberal use of intraarterial vasodilators is recommended to combat vasospasm, which occurs frequently with upper extremity artery manipulations. Because the collateral circulation in the arm and hand is so extensive, even partial lysis of an occlusion may avoid amputation or at least limit its extent. Occlusions less than 48 hours old respond better to thrombolysis than do older ones. An important advantage of lytic infusion over surgery is the ability to lyse clots in small vessels of the forearm and hand. Stroke from embolization of pericatheter clot has been reported with prolonged infusions, but it is a rare complication.
Chronic upper extremity ischemia (online case 29)
Etiology
A variety of diseases may cause subacute or chronic upper extremity ischemia20,21 (Box 9-2). Atherosclerosis usually affects the proximal segments of the subclavian artery and less often the brachiocephalic artery. Oddly, symptomatic disease is far more common in the left than the right subclavian artery. The various sources of thromboemboli were considered in the previous section.
Imaging
Duplex sonography, CT angiography, and MR imaging (MRI) play a role in evaluation of patients with suspected proximal arterial obstruction, particularly when they have symptoms of subclavian steal.11–13,28 Doppler ultrasound signs of obstructive disease include a “parvus et tardus” waveform (downstream lesion) and loss of normal diastolic flow reversal (upstream lesion).11
Catheter angiography is performed when noninvasive imaging studies are equivocal (a rare situation) or endovascular therapy is contemplated. Atherosclerotic stenoses are typically found at the origins of the subclavian or brachiocephalic arteries (see Fig. 9-15). With proximal subclavian artery obstruction, flow in the ipsilateral vertebral artery may be reversed. Thrombotic occlusions produce an abrupt vessel cutoff. Arteriographic findings in thoracic outlet syndrome and more unusual causes of chronic obstruction are considered in later sections.
Treatment
Endovascular therapy
When feasible, catheter-based interventions (usually primary stent placement) are preferred for subclavian and brachiocephalic artery obstructions.24,29–32 In a minority of cases, direct brachial artery puncture is necessary instead of (or combined with) femoral artery access:
Surgical therapy
The preferred operative method for treating total subclavian artery occlusion is an extrathoracic bypass procedure, such as carotid-subclavian bypass, carotid-subclavian transposition, axilloaxillary bypass, or subclavian-subclavian bypass.29,38 Brachial artery revascularization is done with autologous vein or synthetic graft material.39
Thoracic outlet syndrome
Etiology
The various forms of thoracic outlet syndrome are a distinct set of clinical disorders of the upper extremity caused by extrinsic compression of the major nerves and blood vessels exiting or entering the thorax. In more than 90% of affected persons, symptoms are caused by compression of the brachial plexus and related nerves; arterial compression is responsible for less than 5% of cases.40–42 However, these frequently reported figures are strongly influenced by the composition of referral patterns.
The subclavian and axillary arteries are subject to compression primarily within three well-defined anatomic regions: the interscalene triangle, costoclavicular space, and retropectal (subcoracoid) space (Fig. 9-17). Imaging studies in normal volunteers show that a significant minority of healthy individuals exhibit arterial constriction within the costoclavicular and retropectal spaces with arm elevation.43,44 In a small number of patients, however, this physiologic narrowing is exaggerated by one of several musculoskeletal abnormalities. These include cervical ribs, elongated C7 transverse processes, and congenital or acquired pathology of the first rib or clavicle.45
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree