Fig. 29.1
Normal aortic arch
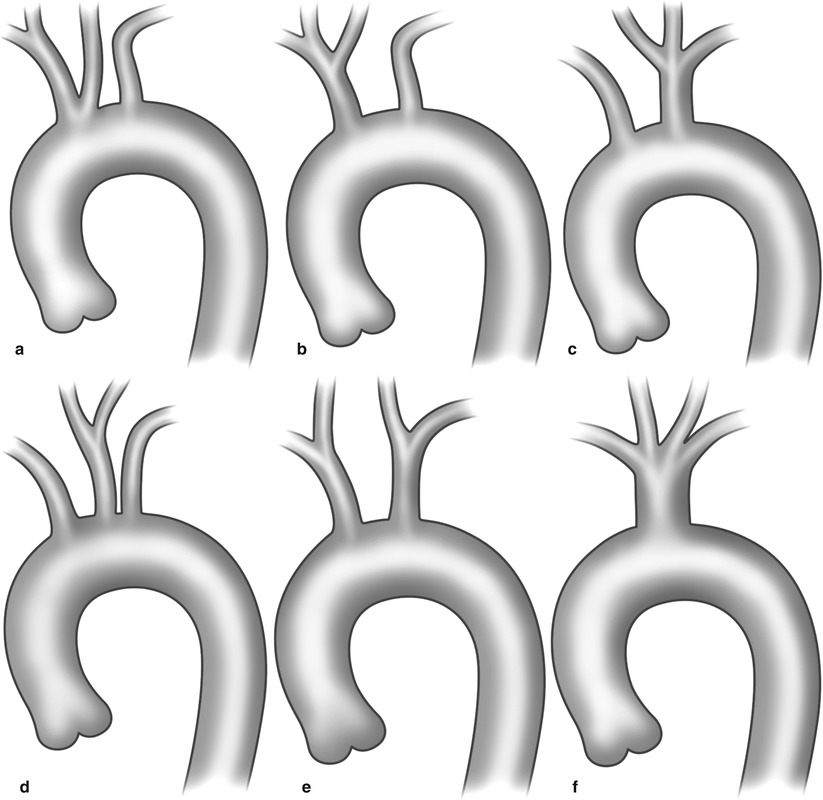
Fig. 29.2
Aortic arch variants – (a) common trunk of brachiocephalic trunk and right common carotid artery (bovine arch), (b) left common carotid artery arising from brachiocephalic trunk, (c) right and left common carotid arising from left subclavian artery, (d) right and left carotid arteries arising from common aortic trunk, (e) left common carotid artery arising from left subclavian artery, and (f) common trunk for subclavian and carotid arteries
The most important branches of the subclavian artery arise from the proximal segment of the artery (the vertebral and the internal mammary branches of the subclavian artery). These branches supply the posterior cerebral circulation (vertebral) and anterior chest wall (internal mammary artery). In 5 % of patients, the left vertebral artery arises directly from the aortic arch between the left subclavian artery and left common carotid artery. The subclavian artery is divided into three parts: proximal (ostium to origin of vertebral artery), middle (segment including vertebral and IMA), and distal (segment beyond IA to lateral border of pectoralis minor).
At the lateral margin of the first rib, the subclavian artery becomes the axillary artery. The axillary artery gives off the anterior and posterior circumflex humeral branches before continuing on as the brachial artery at the distal aspect of the humerus. In the forearm, the brachial artery supplies the deep brachial branch that runs posteriorly and the superior and inferior ulnar collateral arteries. At the elbow, the brachial artery gives rise to the radial and the ulnar arteries.
The ulnar artery is usually the larger of the two branches in the forearm, and it gives rise to the anterior and posterior ulnar recurrent arteries supplying collateral flow to the elbow before giving rise to the common interosseous artery in the antecubital fossa. The ulnar artery then descends along the medial aspect of the forearm. The radial artery gives off a recurrent radial branch before traversing the lateral aspect of the forearm. In some cases, the radial artery may originate high from the axillary (1–3 % cases) or upper brachial artery (15–20 % cases) [4].
In the hand, the ulnar artery supplies the superficial palmar arch, while the radial artery supplies the deep palmar arch (Fig. 29.3). In 10 % of cases, the anterior interosseous or median artery supplies the deep palmar arch. The princeps pollicis and radialis indicis arteries arise from the radial artery and supply the thumb and index finger. The superficial palmar arch gives off three or four common palmar digital arteries, and the deep palmar arch gives off the palmar metacarpal arteries. At the bases of the proximal phalanges, adjacent metacarpal vessels from each arch join and divide into the proper digital arteries to supply the fingers.
Fig. 29.3
(a and b) Brachial and hand circulation
Patient Selection
As with all endovascular procedures, careful patient selection is crucial to maximizing patient safety and procedural success rates while minimizing the risk of complications. This requires careful planning and a fundamental knowledge of normal and abnormal vascular anatomy in addition to details of each patient’s history, physical examination, and noninvasive test results. An understanding of the technical nuances, safety, indications, and potential complications is essential before undertaking a peripheral intervention.
In general, endovascular revascularization is reserved for patients with symptomatic subclavian or brachiocephalic disease. However, most patients with subclavian or brachiocephalic artery disease are asymptomatic due to the slow development of atherosclerosis over time and the rich network of collateral flow that develops. These lesions are usually detected incidentally by the finding of asymmetric arm blood pressures difference of >15 mmHg or on noninvasive imaging performed for another indication. Arm pain, fatigue, ache, heaviness, or numbness with exertion may be misdiagnosed as arthritis, a pinched nerve, or other neuromusculoskeletal disorders. Evidence of distal thromboembolism, acute upper extremity limb ischemia, or chronic ischemic symptom (ischemic rest pain or digital ulceration) is a sign of upper extremity stenosis or occlusion. Symptoms such as dizziness, diplopia, nystagmus, ataxia, vertigo, drop attacks, or syncope may be due to compromise of the posterior cerebral circulation as a result of significant subclavian steal syndrome (SSS) with retrograde vertebral flow in the setting of significant subclavian stenosis (Table 29.1). In patients with prior bypass surgery, angina or ischemia due to compromised flow through the IMA bypass graft may occur due to subclavian stenosis or brachiocephalic stenosis on the right.
Table 29.1
Indications for upper extremity intervention
Indication |
|---|
Upper extremity claudication |
Vertebrobasilar insufficiency |
Ischemia or ulceration due to distal embolization |
Subclavian steal syndrome (SSS): |
Coronary-subclavian steal symptoms |
Vertebral-subclavian steal symptoms |
Preemptive protection of coronary artery bypass graft (IMA) |
Protection of axillofemoral bypass or lower extremity claudication with axillofemoral graft |
Protection of axillo-axillo bypass graft |
Protection of arterio-venous fistula |
Preemptive left subclavian stenting prior to thoracic endovascular aortic repair (TEVAR) [9] |
The major contraindication to subclavian/brachiocephalic intervention is the presence of an acute thrombus. Embolization to the vertebral artery or right internal carotid artery during subclavian or brachiocephalic artery intervention is an important complication. With thrombotic lesions, we recommend treatment with either thrombolytics or anticoagulation for 4 weeks prior to intervention. The use of embolic protection devices should also be considered. Patients with long occlusions (>5 cm) combined with severe calcification and occlusions in proximity of the vertebral artery ostium and patients with arteritis should be considered for surgical revascularization.
The major risk of upper extremity interventions is the risk of distal embolization; however, this risk is low and generally less than 1 % in most series. [4] Access site complications are another common complication with a rate of up to 5 % in some series. The major risk for access site complication is brachial access due to difficulty to control hemostasis, hematoma, thrombosis, fistula formation, and pseudoaneurysm. Stent migration has also been reported, possibly due to stent malapposition. The rate of stent restenosis is less than 10–15 % and comparable to surgical failure rates [2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree