Urinary Tract Infection
Teresa Chapman, MD
LEARNING OBJECTIVES
1. Define atypical urinary tract infection.
2. List appropriate indications for a fluoroscopic voiding cystourethrogram (VCUG) in an infant or child presenting with urinary tract infection.
3. Describe limitations and advantages of radionuclide cystography compared with fluoroscopic VCUG.
4. Identify pediatric patients who require daily antibiotics for prevention of urinary tract infection.
5. Describe rationale behind a “top-down” approach in imaging kidneys with dimercaptosuccinic acid (DMSA) renal scintigraphy following presentation with a urinary tract infection.
INTRODUCTION
A thorough description of urinary tract anomalies is presented in Chapter 19. Any anomaly that allows for urinary stasis may predispose an individual to urinary tract infection (UTI). UTI also occurs with normal anatomy, and diagnostic imaging plays an important role in the assessment of these children. In this chapter, genitourinary system infections and the application of diagnostic imaging to patients with suspected or diagnosed infections of the genitourinary system are discussed. Our fundamental role in imaging is to identify pediatric patients who require continued further imaging, antibiotic prophylactic therapy, and/or referral to nephrology or urologic surgery subspecialists.
HISTORICAL PERSPECTIVE: INFANTS AND SMALL CHILDREN
With introduction of routine vaccinations for Haemophilus influenzae Type b and Streptococcus pneumoniae, the incidence of bacteremia and meningitis as diagnoses explaining the presentation of fever in infants and small children has dropped substantially. Since the 1970s, there has been an increasing recognition of UTIs as a cause of fever in infants and toddlers without a clinically evident source of infection.1 In children between 2 and 24 months of age presenting with fever above 38.0°C, the prevalence of UTI is approximately 5%.2,3 If urinalysis suggests a UTI (based on positive leukocyte esterase, positive nitrite test, or microscopic analysis showing leukocytes or bacteria), then culture of urine acquired by either sterile urinary bladder catheterization or suprapubic aspiration is required. The presence of at least 10,000 colony-forming units per mL of a uropathogen confirms the diagnosis of UTI.3 Standard treatment of a UTI is 10 to 14 days of antibiotic therapy.
The primary concern in children presenting with febrile UTI is that any renal parenchymal injury could potentially lead to future complications such as hypertension or renal insufficiency.4, 5 and 6 Clinical management of febrile UTI has historically varied considerably between different outpatient centers, as well as for inpatient cases.7,8 In the late 1900s and early 2000s, standard management of infants and small children with febrile UTI would typically include initial antibiotic therapy, establishment of a daily prophylactic antibiotic, and multimodality imaging with ultrasound, voiding cystourethrogram (VCUG), and scintigraphic renal cortical imaging with 99mTc dimercaptosuccinic acid (DMSA).9 These practices have more recently been scrutinized in an effort to reduce the burden on impacted families, the financial cost to society, and the radiation exposure to patients required for VCUG and scintigraphy.
Multicenter investigations and extensive expert committee work, both in the United States and in the United Kingdom, have focused on unifying standards for management of UTI, including application of imaging and use of medical therapy.2,10 Two main observations in the literature have challenged the routine use of antibiotic prophylactic therapy in infants and small children with a history of febrile UTI: pyelonephritis occurs even without a diagnosis of VUR, and several studies have shown that prophylaxis with a daily antibiotic dose does not necessarily offer the desired protection against a subsequent UTI.11, 12, 13, 14 and 15 The American Academy of Pediatrics (AAP) guidelines published in 2011 estimate that only 1 infant or small child in a cohort of 100 individuals presenting with a first-time febrile UTI will have high-grade VUR, which is not high enough to merit performing 100 VCUG procedures on the full cohort.2 Large practices have successfully applied these new guidelines, with close to 100% compliance in the inpatient and outpatient settings, drastically lowering the number of VCUG studies performed following a patient’s first UTI.7
ULTRASOUND ASSESSMENT FOLLOWING UTI
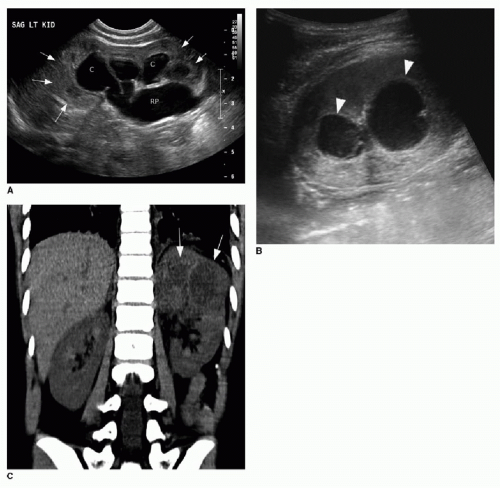
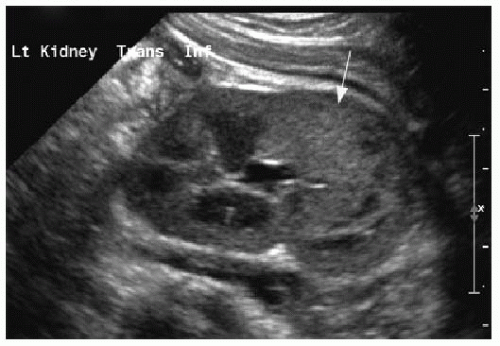
The diagnosis of pyelonephritis is made based on clinical presentation and laboratory evaluation of the urine. All cases of febrile UTI merit diagnostic imaging to assess for (1) underlying risk factors, as discussed in Chapter 19, and (2) complications of infection. The 2011 AAP guidelines report the rationale for obtaining renal and urinary bladder ultrasound on all infants and young patients (age 2 to 24 months) presenting with a febrile UTI.2 In this patient population, approximately 15% of ultrasound examinations will be abnormal, and no more than 2% of ultrasound studies will lead to further clinical action.16,17 Nevertheless, given the safety and noninvasive nature of ultrasound, the use of renal and bladder ultrasound in this clinical context is recommended by the AAP. Renal ultrasound is usually performed after complete treatment of the UTI, but early sonographic imaging after only 2 days of antibiotic therapy would be appropriate if the illness is severe and if the child is not responding to therapy as expected. Early imaging is appropriate to evaluate for serious complications such as renal or perinephric abscesses or pyonephrosis associated with unanticipated collecting system obstruction (Fig. 20.1). Imaging too early in straightforward cases is unlikely to offer additional information and may not provide useful baseline information to assess renal growth in the future, as acute pyelonephritis can cause transient renal enlargement and focal areas of abnormal
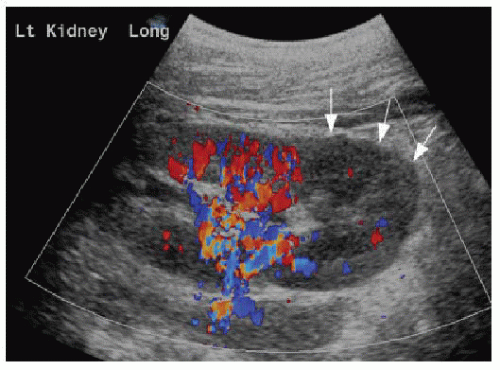
renal echogenicity (Fig. 20.2). Furthermore, the endotoxin produced by Escherichia coli may cause transient distention of the collecting system, which could be confused with obstruction.17 Although renal cortical scintigraphy is a much more sensitive study to detect acute inflammation in pyelonephritis (discussed later in this chapter), color and power Doppler applied to renal ultrasound may be helpful to identify areas of renal parenchymal infiltration by infection, manifested by areas of hypovascularity (Fig. 20.3).18 This technique can be very difficult in the infant and young child, however, due to patient movement.
renal echogenicity (Fig. 20.2). Furthermore, the endotoxin produced by Escherichia coli may cause transient distention of the collecting system, which could be confused with obstruction.17 Although renal cortical scintigraphy is a much more sensitive study to detect acute inflammation in pyelonephritis (discussed later in this chapter), color and power Doppler applied to renal ultrasound may be helpful to identify areas of renal parenchymal infiltration by infection, manifested by areas of hypovascularity (Fig. 20.3).18 This technique can be very difficult in the infant and young child, however, due to patient movement.
Reemphasizing the discussion earlier in this chapter, following the AAP guidelines, infants and toddlers with a single UTI and a normal renal ultrasound require no further imaging.2,7 However, since publication of those guidelines, subsequent studies evaluating the efficacy of renal ultrasound as a screening tool to successfully identify at-risk patients have already challenged this approach.8,19,20 In the next decade, we are likely to see alterations in how this challenging problem is approached.
VOIDING CYSTOURETHROGRAM FOLLOWING UTI
VCUG, a procedure described in Chapter 19




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree