(1)
Department of Medical Imaging, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
(2)
Department of Medical Imaging and Radiological Sciences, Institute of Radiological Research Chang Gung University, Taoyuan, Taiwan
2.1 Acute Pyelonephritis
Case 1
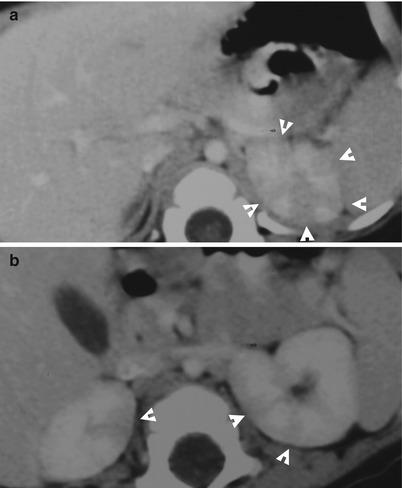
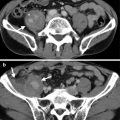
Fig. 2.1
Enhanced computed tomography (CT) shows acute pyelonephritis of both kidneys. Figure 2.1a, enhanced axial renal CT image shows stripes of hypodense areas (arrowheads) relative to normal renal parenchyma of the left renal upper pole. Figure 2.1b, enhanced axial renal CT image shows low-density areas (arrowheads) of both kidneys. Note that the hypodense areas involve the whole thickness of the renal parenchyma.
Case 2
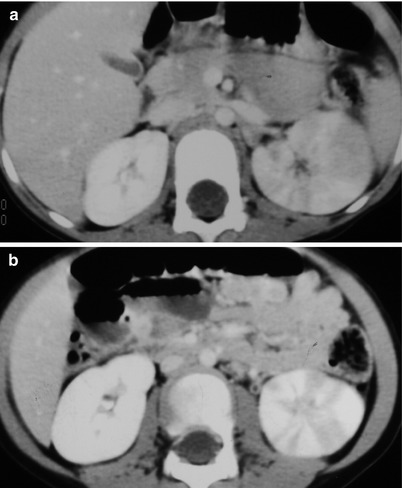
Fig. 2.2
Computed tomography (CT) images illustrate imaging characteristics of a left acute pyelonephritis. Enhanced axial CT images (Fig. 2.2a, b) show variable sizes of hypodense areas of the left renal parenchyma. Note globular appearance of the left kidney as an imaging sign of renal swelling.
Case 3
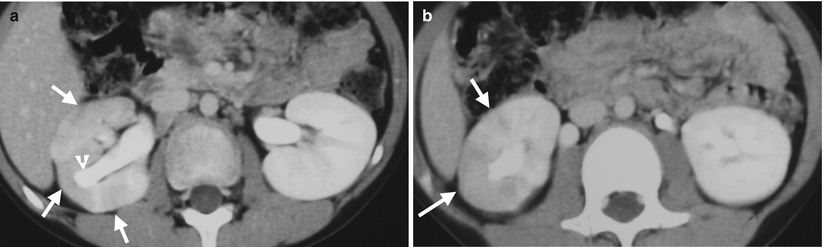
Fig. 2.3
Computed tomography (CT) images illustrate imaging characteristics of right acute pyelonephritis in a 3-year-old child. Enhanced axial CT images (Fig. 2.3a, b) show hypodense areas of the right renal parenchyma, appearing as wedge shapes or stripes (arrows). Note focal hydrocalicosis (arrowhead, 2.3a) of the right kidney.
Key Diagnostic Features
Acute renal pyelonephritis is better diagnosed by enhanced computed tomography (CT) or magnetic resonance imaging (MRI) than by renal ultrasound (US). Acute pyelonephritis usually has no abnormal density area on unenhanced CT or MRI except for severe cases. In severe forms of acute pyelonephritis, a liquefied region in acute pyelonephritis foci could occur, which may appear as lower density than normal parenchyma. Therefore, enhanced CT or MRI is usually necessary for evaluating the extent of infection in acute pyelonephritis patients. On enhanced CT or MRI, acute pyelonephritis typically shows striated nephrogram [1]. Striated nephrogram consists of one or more stripes or wedge shapes of hypodense areas on the renal parenchyma, which involves the whole renal parenchymal thickness [1]. In radiological literature, the term “multifocal bacterial nephritis” has been used to describe multiple low-density area involvements by acute pyelonephritis on enhanced CT or MRI. Acute pyelonephritis may involve one or both kidneys. Other common associated findings of acute pyelonephritis include renal swelling and dirty ipsilateral perinephric fat or fluid. In severe infection of acute pyelonephritis, the involved kidney could have a delayed hemodynamics and nephrogram. At follow-up images, the infected site of renal parenchyma shows renal scarring appearance.
Main Differential Diagnoses
1.
Focal renal infarct
Focal renal infarct appears as a wedge-shaped area of low density at the renal parenchyma after contrast medium enhancement, which is similar to that seen in acute pyelonephritis [2]. However, several imaging findings may be used for differentiation between focal renal infarct and acute pyelonephritis. The presence of cortical rim sign in the periphery of hypodense regions suggests a diagnosis of focal renal infarct. Nonetheless, the absence of cortical rim sign could not exclude the diagnosis of focal renal infarct. On the other hand, the presence of renal swelling, globular renal shape, and dirty perinephric space in addition to wedge-shaped low-density area on enhanced CT or magnetic resonance imaging favors acute pyelonephritis.
2.2 Nephronia
Case 4
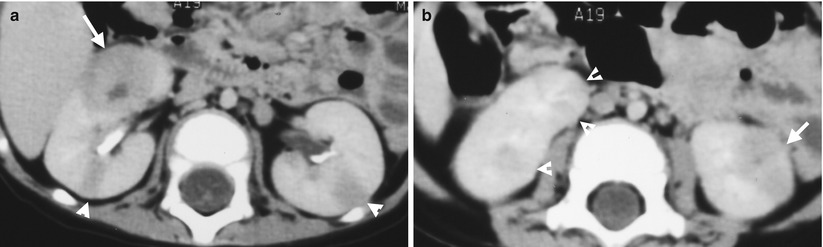
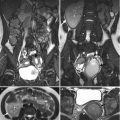
Fig. 2.4
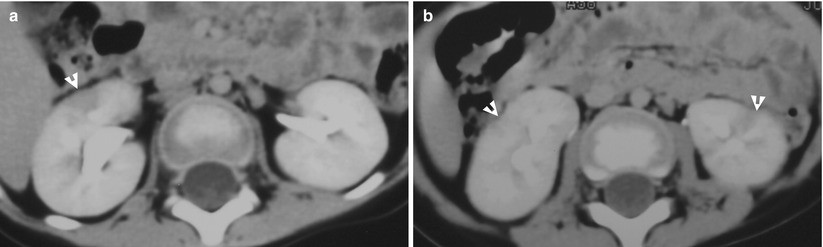
Fig. 2.5
Renal nephronia and acute pyelonephritis of both kidneys are depicted of a patient in first and follow-up images of computed tomography (CT). Figure 2.4a, enhanced axial renal CT image at midportion level shows hypodense areas in stripes (arrowheads) of both kidneys as acute pyelonephritis. There is a round nodule (arrow) at the right kidney as an imaging finding of renal nephronia. Figure 2.4b, enhanced renal CT image at lower pole level shows acute pyelonephritis appearance (arrowheads) of the right kidney. Note an oval hypodense nodule (arrow) with a tiny cystic area in the center. Figure 2.5a, enhanced axial renal CT image at midportion level, 3 weeks later after Fig. 2.4a, shows that the prior nodule in Fig. 2.4a becomes a wedge-shaped low-density area without obvious swelling. Figure 2.5b, enhanced axial renal CT image at the lower pole shows focal renal parenchymal scarring (arrowheads) of both kidneys. There are still visible hypodense areas of both kidneys, but less obvious than before.
Key Diagnostic Features
Renal nephronia is one special form of bacterial infection of the kidney. Unlike striated nephrogram typical for acute pyelonephritis, renal nephronia appears as a round or oval hypodense nodule of the kidney on enhanced computed tomography (CT) or magnetic resonance imaging (MRI). There could be some cystic area of variable sizes in a renal nephronia. Therefore, renal nephronia has been reported for mimicking renal cell carcinomas (RCCs) in the literature. However, renal nephronia has some associated findings which may aid in its diagnosis. The presence of striated nephrogram as acute pyelonephritis in ipsilateral kidney implies that the nodule is very likely to be renal nephronia. The presence of ipsilateral perinephric dirty fat and fluid also supports a diagnosis of renal nephronia. Clinical symptoms and signs such as fever, flank pain, knocking pain, pyuria, and high WBC counts also favor the presence of urinary tract infection. In addition, follow-up enhanced CT or MRI studies may show renal scarring or less obvious findings of renal infection if appropriate antibiotics have been prescribed.
Main Differential Diagnoses
1.
Renal cell carcinoma
Renal cell carcinomas confined in the kidney could have similar pictures as those of renal nephronia [3]. The absence of associated findings related to infection on images as well as clinical symptoms and signs of infection favors RCC diagnosis. In encountering a rare instance of infected RCC, follow-up images by CT or MRI after antibiotics treatment are usually necessary to distinguish an RCC from a renal nephronia.
2.3 Renal Abscess
Case 5
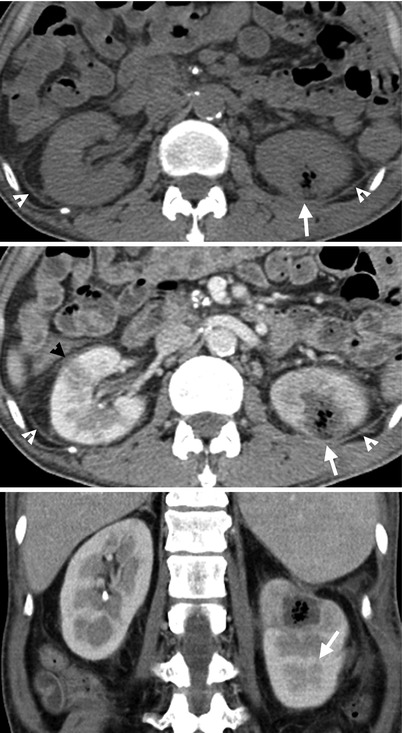
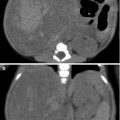
Fig. 2.6
Renal enhanced computed tomography (CT) shows imaging features of renal abscess. Figure 2.6a, unenhanced axial renal CT image shows a mixed cystic and air density nodule (arrow) at the left kidney. Figure 2.6b, enhanced renal CT image shows a renal abscess appearing as a cystic mass with central air density (arrow). Striated nephrogram (black arrowhead) is noted at the right kidney as an imaging presentation of acute pyelonephritis. Note thickening of bilateral perinephric fascia and perinephric fat (white arrowheads). Figure 2.6c, enhanced coronal renal CT image shows a renal abscess (arrow) at the left upper pole.
Case 6
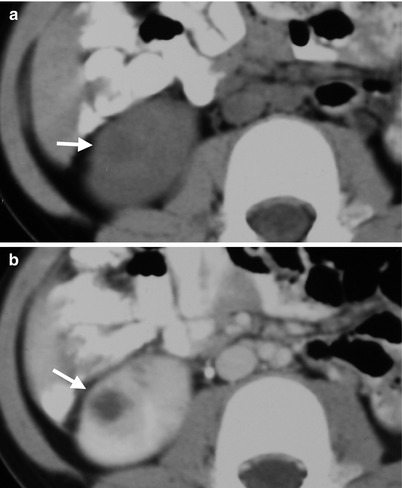
Fig. 2.7
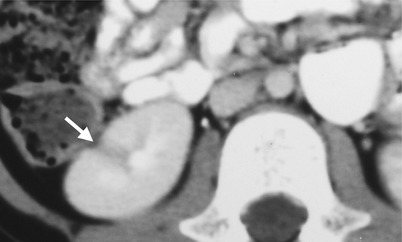
Fig. 2.8
Renal computed tomography (CT) shows imaging characteristics of renal abscess and its follow-up appearance. Figure 2.7a, unenhanced axial renal CT image shows a cystic mass (arrow) at the right kidney. Figure 2.7b, enhanced axial renal CT image shows a cystic mass with thick wall (arrow) at the right kidney. Figure 2.8, enhanced axial renal CT image at 3 months later shows renal scarring (arrow) at the right upper pole.
Key Diagnostic Features
Renal abscess is diagnosed on computed tomography (CT) or magnetic resonance imaging (MRI) by the presence of a cystic mass with internal air density. Renal abscess could also appear as a cystic mass with rim wall enhancement on CT and MRI. Similar to acute pyelonephritis and renal nephronia, there are usually associated imaging findings, such as thickened perinephric fascia, dirty perinephric fat, perinephric fluid collection, and renal swelling, to support imaging diagnosis of renal abscess. Furthermore, renal bacterial infection could present as a disease spectrum varied from acute pyelonephritis to renal abscess. Therefore, it is common for patients to have concurrent imaging findings of renal abscess, renal nephronia, and acute pyelonephritis on one imaging study. Furthermore, as the infection could also spread to anatomical regions other than the kidney, it is important to identify the involved extent of urinary tract infection on images. In summary, a renal cystic mass with internal air density or rim enhancement on images in the presence of other supportive imaging signs of renal infection suggests a diagnosis of renal abscess.
Main Differential Diagnoses
1.
A renal neoplasm with necrosis
The necrotic part in a renal neoplasm appears as an internal cystic area on images, which simulate the cystic content of a renal abscess. However, being a renal neoplasm, the soft tissue non-necrotic part in a renal neoplasm usually has a more irregular profile and thickness than that of the wall of a renal abscess. There are also no associated infection findings on images in a necrotic renal neoplasm, unless it has superimposed infection.
2.
Infected renal cyst
A renal simple cyst is a cyst with thin or unrecognizable wall. When a cyst is infected, the wall could be thickened and enhanced and there could be coexisting infection findings on images. Nonetheless, a renal cyst existed before infection and a renal abscess occur without prior cyst. Therefore, the key to differentiate an infected renal cyst from a renal abscess is based on whether there is a preexisting renal cyst or not. If there are available prior images, a comparison between the anatomical location on a prior imaging study and this imaging examination could clarify this question. If there is evidence of renal cystic diseases on images, an infected renal cyst is also favored as well.
2.4 Renal Subcapsular Abscess
Case 7
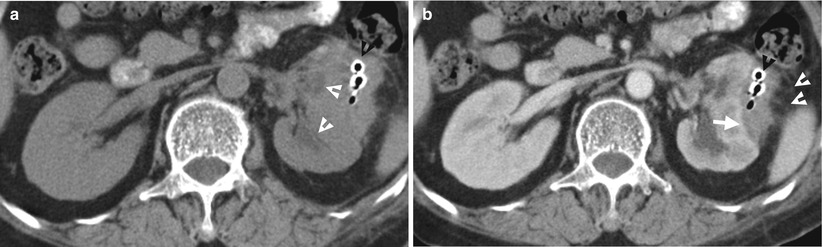
Fig. 2.9
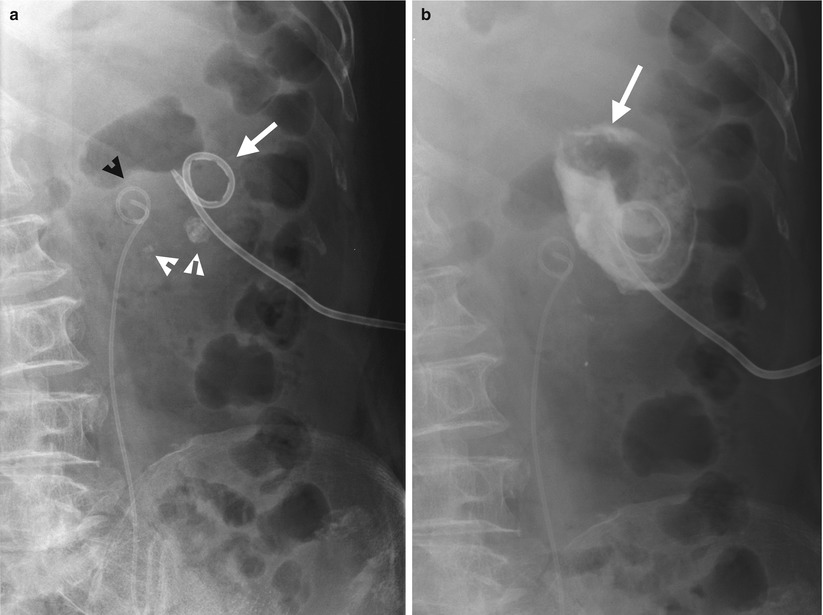
Fig. 2.10
Renal enhanced computed tomography (CT) shows imaging features of renal subcapsular abscess. Figure 2.9a, unenhanced axial renal CT image shows mass effect on left renal collecting system (white arrowheads). The left renal subcapsular abscess is isodense to the left renal parenchyma on unenhanced CT. Thus, the extent and margin of the left renal subcapsular abscess could not be clearly delineated on this unenhanced CT image. Figure 2.9b, enhanced renal CT image shows the left renal subcapsular abscess (white arrow) being hypodense to the adjacent renal parenchyma. The left subcapsular abscess has an irregular lateral profile with dirty fat in ipsilateral perinephric space (white arrowheads) and thickening of the left perinephric fascia. This subcapsular abscess has a lenticular shape. The left renal parenchyma is compressed to a concave appearance by this subcapsular abscess. Pus is drained out via the radiopaque drainage tube (black arrowhead) inserted in the left renal subcapsular abscess. Figure 2.10a, baseline plain radiography after drainage tube inserted in the left subcapsular abscess shows several radiopaque left renal stones (white arrowheads). The tip of an abscess drainage catheter (white arrow) is separated from the cranial loop of a double J catheter (black arrowhead). Figure 2.10b, plain radiography of the abscess after contrast medium injection via the abscess drainage catheter shows opacification of the abscess space (white arrow), which has no communication with the left kidney.
Key Diagnostic Features
Renal subcapsular abscess is diagnosed on images by recognition of an abscess which is located in the renal subcapsular space. Abscesses are typically of cystic density on unenhanced CT; however, with a thick pus in an abscess, its density could become isodense to the renal parenchyma. On the other hand, any space-occupying lesion located in the renal subcapsular space would exert mass effect on the adjacent renal parenchyma as well as the ipsilateral renal collecting system. Similar to renal abscess, renal subcapsular abscess is usually associated with perinephric stranding, perinephric fluid collection, perinephric dirty fat, and thickened perinephric fascia. Because the shape of a renal subcapsular hematoma is restricted laterally by the renal capsule and medially by the adjacent renal parenchyma, it usually has a lenticular shape on images.
Main Differential Diagnoses
1.
Perinephric abscess
Perinephric abscess has less mass effect on the adjacent renal parenchyma and ipsilateral renal collecting system. Perinephric space usually does not form a lenticular shape as that seen in the renal subcapsular abscess. The large space of the perinephric area also allows a much larger abscess than the size of a renal subcapsular abscess.
2.
Renal subcapsular hematoma
Hematoma is usually not enhanced after contrast medium administration on computed tomography (CT) and magnetic resonance imaging (MRI). Acute hematoma is recognized by its high density of 60–90 Hounsfield units on unenhanced CT images, without enhancement after contrast medium administration. For a renal subcapsular hematoma, there is usually the lack of associated infection signs on images unless there is superimposed infection of a preexisting hematoma.
2.5 Perinephric Abscess
Case 8

Fig. 2.11
Renal computed tomography (CT) shows imaging features of perinephric abscess. Unenhanced axial renal CT images (Fig. 2.11a, b) show a large cystic mass (arrows) displacing the right kidney anterolaterally. Thickening of the right perinephric fascia is depicted (arrowheads). Enhanced axial renal CT images (Fig. 2.11c, d) show an abscess with thick wall (arrow) with thickened fascia (arrowhead). Another abscess (black arrow) involving the right psoas muscle is noted.
Case 9
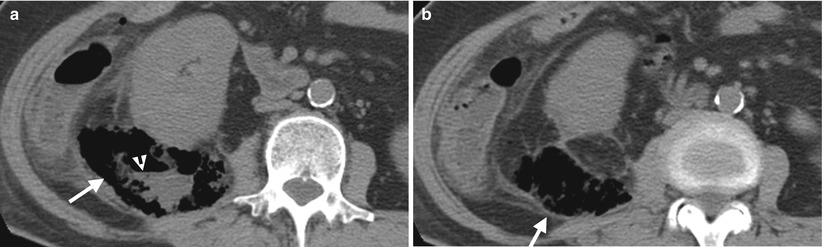
Fig. 2.12
Renal computed tomography (CT) shows a patient with perinephric abscess. Figure 2.12a, unenhanced axial CT images at midportion of the right kidney shows a mixed air and cystic area (arrow) with air-fluid layering (arrowhead). Figure 2.12b, unenhanced axial CT image at the lower pole of the right kidney shows abnormal air collection area (arrow) in the right perinephric space. The right kidney is anteriorly displaced and there is dirty fat in the adjacent pericolic fat of the ascending colon.
Key Diagnostic Features
Perinephric abscess is diagnosed on CT by identifying an abscess located in the perinephric space. A perinephric abscess could present on CT as a cystic mass with thickened and enhancing wall, a mass with air-fluid layering, a lesion full of air collection, or any combination of the above three pictures. As the perinephric space is contiguous to the kidney and confined in a potentially large perinephric space, a perinephric abscess usually has obvious displacement of the ipsilateral kidney, especially if it is large sized. The compression effect of the adjacent renal parenchyma by a perinephric abscess is usually less evident than the displacement effect.
Main Differential Diagnoses
1.
Subcapsular abscess
Subcapsular abscess usually has a lenticular shape with obvious mass effect on the adjacent renal parenchyma. Subcapsular abscess usually has a smaller size than a perinephric abscess due to the confined effect of the renal capsule.
2.6 Pyonephrosis
Case 10
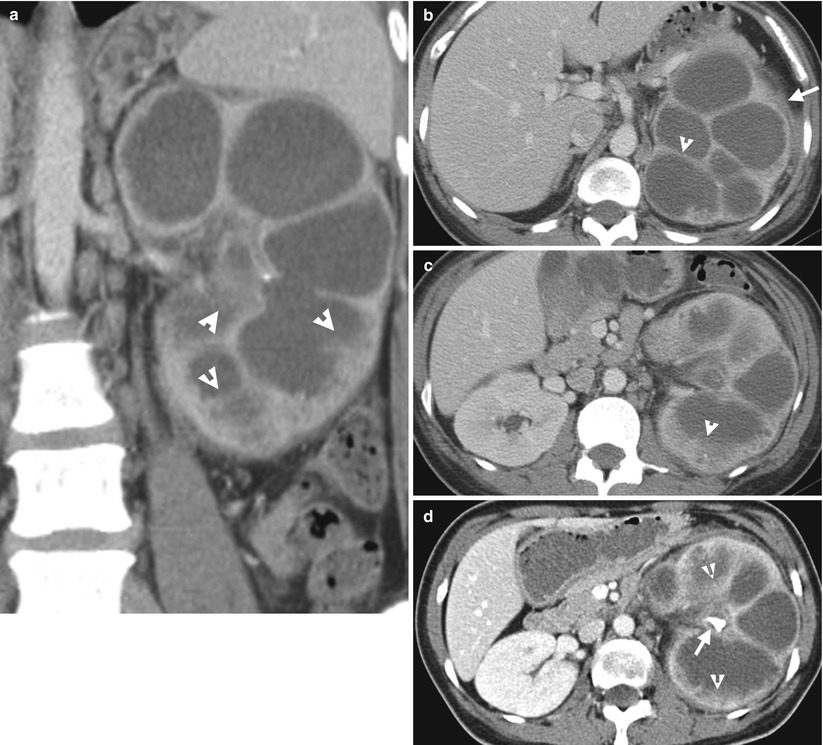
Fig. 2.13
Enhanced computed tomography (CT) shows imaging findings of pyonephrosis. Figure 2.13a, coronal enhanced CT image shows dilatation of left pelvicalyceal system with enhancing wall and debris (arrowheads). Figure 2.13b, axial enhanced CT image shows abnormally thickened wall (arrowhead) in left hydronephrosis with left perinephric fascia thickening (arrow) and dirty left perinephric fat. Figure 2.13c, axial enhanced CT image shows layering appearance (arrowhead) of debris in dependent portion of a left renal middle calyx. The left renal pelvis is small in size with thickened wall as well. Figure 2.13d, axial enhanced CT image shows a right renal pelvis calculus (arrow) with resultant left pyonephrosis, as evidenced by urine-debris layering (arrowheads) in calyces. Gross and microscopic examinations of the left nephrectomy specimen reveals marked pyonephrosis with pus in the left renal collecting system as well as severe acute and chronic inflammation.
Key Diagnostic Features
Pyonephrosis means infection of an obstructed and dilated renal collecting system. Therefore, pyonephrosis is diagnosed on images not only by presence of hydronephrosis or hydrocalicosis but also by imaging signs suggestive of infection. On CT, the presence of urine-debris layering, air-fluid layering, or debris in a dilated pelvicalyceal system with adjacent perinephric stranding or fascia thickening suggests pyonephrosis. On MRI, similar signs could be sued for diagnosis of pyonephrosis. On ultrasound, pyonephrosis could be diagnosed by identifying debris as low echoic materials in a dilated renal collecting system with or without layering appearance. The most common cause of obstruction for pyonephrosis is urolithiasis. However, any causes resulting in urinary tract obstruction may suffer from further infection and result in pyonephrosis.
Main Differential Diagnoses
1.
Xanthogranulomatous pyelonephritis
Xanthogranulomatous pyelonephritis (XGN) is an uncommon renal infection, diagnosed by the presence of so-called xanthoma cells. Xanthoma cells are characterized by histiocytes having foamy fat-containing cytoplasm on histological examinations. The classical XGN involves the whole kidney. The typical findings of classical XGN on CT are a staghorn stone, multiple hypodense areas surrounding the stone, and poor or absence of function of the involved kidney. Thus, the presence of normal renal excretory function in a dilated and infected renal collecting system by calculus obstruction favors the diagnosis of pyonephrosis. Nonetheless, severe pyonephrosis may result in poor or no renal excretory function as well, which may be indistinguishable from XGN on images. On the other hand, the presence of perinephric inflammatory mass or fistula between the kidney and adjacent anatomical structures is much more common in XGN than in pyonephrosis.
2.7 Emphysematous Pyelitis
Case 11
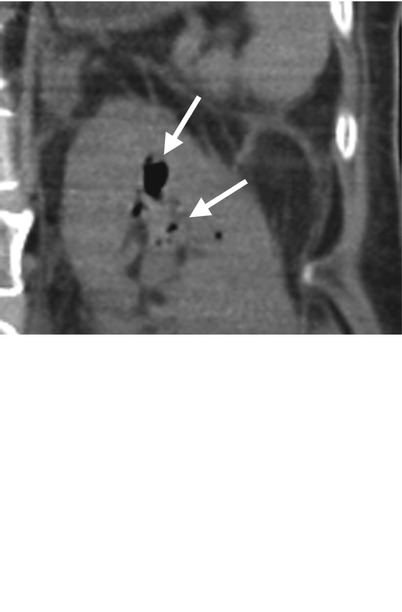

Fig. 2.14
Unenhanced computed tomography (CT) images illustrate typical imaging findings of emphysematous pyelitis. Figure 2.14a, unenhanced coronal CT image shows abnormal air collections of variable sizes (arrows) in the left renal upper calyx. Figure 2.14b, unenhanced sagittal CT image shows air bubbles (arrows) in the left renal and middle calyces. Figure 2.14c, unenhanced axial renal CT image shows abnormal air (arrow) in the left renal upper calyx. Figure 2.14d, unenhanced axial CT image at the left proximal ureter level shows an air bubble (arrow) inside the left proximal ureteral lumen. Note that there is a nonspecific increased stranding of the left perinephric space and thickened left perinephric fascia on all four images.
Key Diagnostic Features
Emphysematous pyelitis is described as an abnormal air collection inside the renal collecting system. Therefore, computed tomography is a much sensitive imaging tool for detecting the presence of air collections inside the lumen of the renal collecting system than plain radiographs of the kidney, ureter, and bladder (KUB), especially in small amounts of abnormal air. The presence of air in the renal collecting system could be due to prior instrumentation or interventions, such as retrograde pyelography (RP), antegrade pyelography (AP), percutaneous nephrostomy, ureteroscopy, ureteral stenting, or biopsy. Gas-producing bacterial infection (e.g., E. coli infection) could also present with emphysematous pyelitis on CT. Since the ureteral lumen is communicated with the renal collecting system, concurrent air collection in the ureter may be seen as well.
Main Differential Diagnoses
1.
Emphysematous pyelonephritis
Classical emphysematous pyelonephritis is defined as the abnormal air collection in the renal parenchyma rather than in the renal collecting system. Emphysematous pyelonephritis implies a much more severe renal infection than emphysematous pyelitis does.
2.8 Emphysematous Pyelonephritis
Case 12

Fig. 2.15
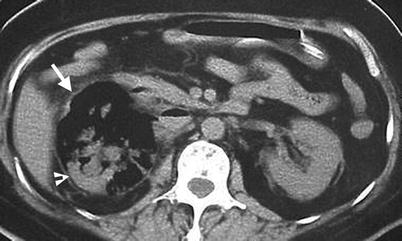
Fig. 2.16
Plain radiograph of the kidney, ureter, and bladder (KUB) and unenhanced computed tomography (CT) show typical imaging sign of emphysematous pyelonephritis. Figure 2.15, KUB shows mottled air density collection in a reniform shape (arrow) of the right abdomen. The left psoas line (arrowheads) is clearly visible. The right psoas line could not be visualized. Figure 2.16, unenhanced axial renal CT image shows the right renal parenchyma being replaced by air density collection (arrow) except a small posterior part (arrowhead). The pictures on KUB and CT are pathognomonic of emphysematous pyelonephritis.
Case 13

Fig. 2.17
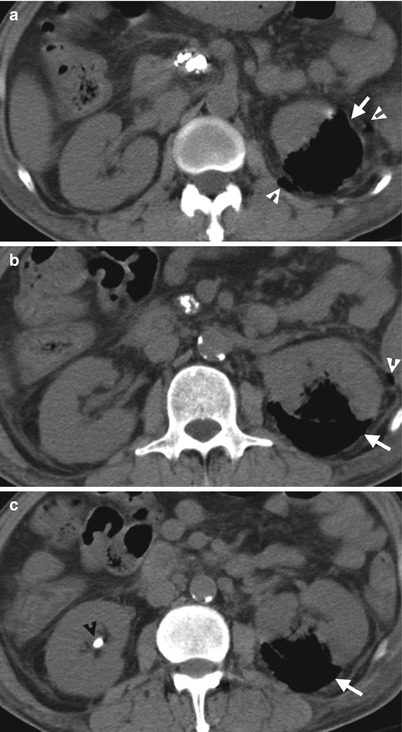
Fig. 2.18
Renal ultrasound (US) and unenhanced computed tomography (CT) show imaging findings in a patient with left emphysematous pyelonephritis. Figure 2.17, left renal US shows a highly echogenic part (arrow) with posterior dirty shadowing, consistent with intrarenal air collection. Serial unenhanced axial renal CT images (Fig. 2.18a–c) show air density collection (arrows) instead of normal renal parenchymal density in the posterior part of the left kidney, suggestive of emphysematous pyelonephritis. The infection extends to the left perinephric space as evidenced by small air bubbles (white arrowheads). A right renal calyceal stone (black arrowhead) is depicted. There are pancreatic head calcifications due to chronic pancreatitis.
Key Diagnostic Features
Emphysematous pyelonephritis is the collection of abnormal air in the renal parenchyma. It occurs most commonly in diabetes mellitus patients. In classical form of emphysematous pyelonephritis, there is no fluid mixed with air density, which reflects poor immune status of the patients. Thus, classical emphysematous pyelonephritis is diagnosed by visualization of air density replacing normal parenchyma, and thus, unenhanced CT is usually sufficient for its diagnosis. If the whole kidney is involved in emphysematous pyelonephritis, plain radiograph of the kidney, ureter, and bladder demonstrates a kidney with air collection showing high contrast to its adjacent structures.
Main Differential Diagnoses
1.
Renal abscess
A renal abscess appears as a mass of mixed cystic and air density or purely cystic density with a thickened wall. The presence of fluid in patients with renal infection reflects better immune response of the patients than that of patients with emphysematous pyelonephritis.
2.9 Xanthogranulomatous Pyelonephritis
Case 14
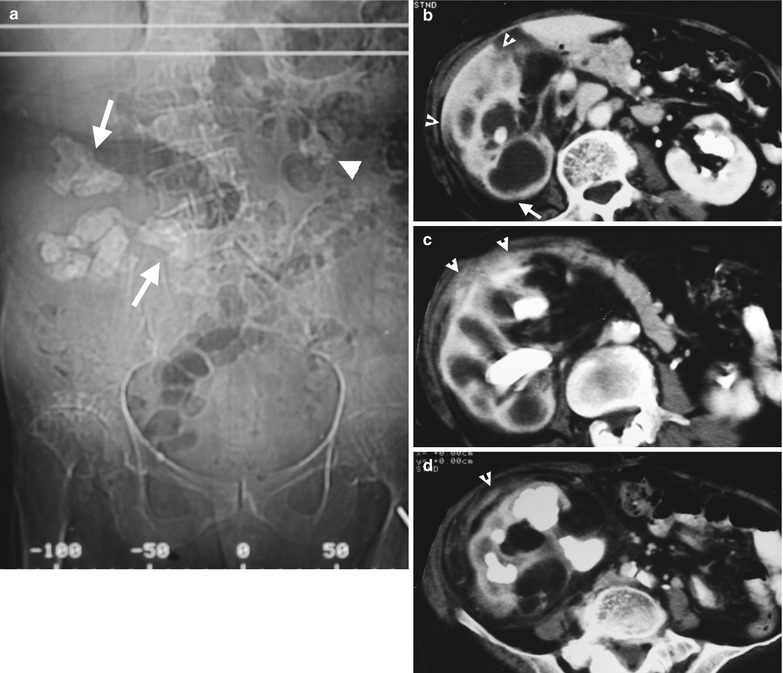
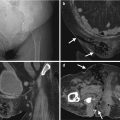
Fig. 2.19
Computed tomography (CT) shows typical imaging sign of xanthogranulomatous pyelonephritis. Figure 2.19a, CT scout film shows right renal staghorn stone (arrows) and left renal stones (arrowhead). Figure 2.19b, enhanced axial CT image at the right renal upper pole level shows obvious enlargement of the right kidney with hypodense areas having rim enhancement (arrow). There is obvious extrarenal inflammation (arrowheads) between the right kidney and the liver. Figure 2.19c, enhanced axial CT image at the right renal midportion level shows extrarenal inflammation abutting anterior abdominal wall. Note the intrarenal hypodense area surrounding the right renal staghorn stone. Figure 2.19d, enhanced axial CT image at the right renal lower pole level shows inflammation (arrowhead) at the right perinephric area. Note the right kidney has no excretion function on all images.
Case 15
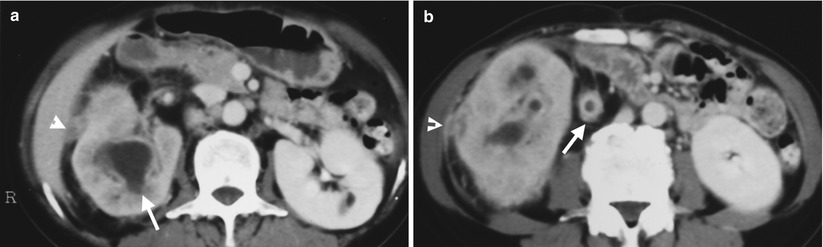
Fig. 2.20
Enhanced computed tomography (CT) shows imaging findings of a 71-year-old woman proven to have right xanthogranulomatous pyelonephritis by histological examination of surgical specimen for a right nephrectomy. Figure 2.20a, enhanced CT at the right renal upper pole level shows no contrast medium excretion of the right kidney with dilated calyx (arrow) and right extrarenal inflammatory soft tissue nodule (arrowhead). Figure 2.20b, enhanced CT at the right renal midportion shows inflammation of the right renal parenchyma with direct extension to the right perinephric space and right perinephric fascia (arrowhead). Strong enhancement of walls of the right renal dilated calyces and right ureter (arrow) is depicted.