(1)
Department of Medical Imaging, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
(2)
Department of Medical Imaging and Radiological Sciences, Institute of Radiological Research Chang Gung University, Taoyuan, Taiwan
7.1 Retroperitoneal Liposarcoma
Case 1

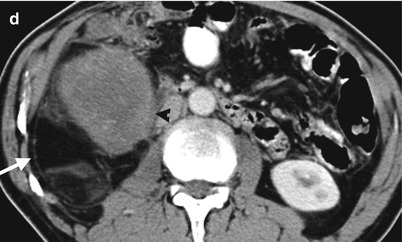
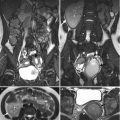
Fig. 7.1
Computed tomography (CT) shows imaging findings of a retroperitoneal liposarcoma with identifiable fatty and soft tissue parts. Scout image of CT (Fig. 7.1a) shows a large space-occupying lesion (arrow) of the right abdomen with displacement of bowel loops. Unenhanced (Fig. 7.1b) and enhanced (Fig. 7.1c) axial CT images at right renal lower pole level show a right retroperitoneal tumor (arrows) surrounding the right kidney without obvious renal involvement. There are identifiable fatty parts (white arrowheads) in this tumor. Enhanced axial CT at the right infrarenal level (Fig. 7.1d) shows an obvious enhancing soft tissue part (black arrowhead) in addition to the fatty part of this retroperitoneal tumor. A retroperitoneal liposarcoma is considered on CT. Histological examination of surgical specimen of the tumor reveals a retroperitoneal well-differentiated liposarcoma.
Case 2
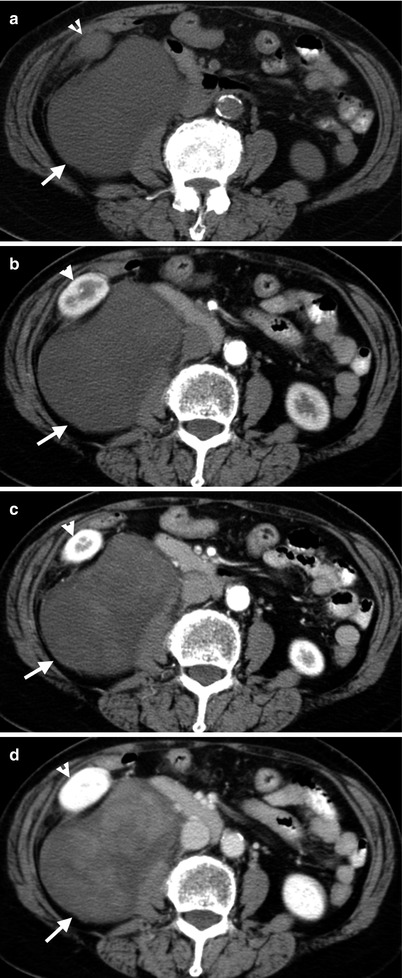
Fig. 7.2
Computed tomography (CT) and magnetic resonance imaging (MRI) illustrate imaging characteristics of a retroperitoneal myxoid liposarcoma. Unenhanced (Fig. 7.2a), enhanced early corticomedullary phase (Fig. 7.2b), enhanced late corticomedullary phase (Fig. 7.2c), and enhanced nephrographic phase (Fig. 7.2d) CT images show gradually increased enhancement of a right retroperitoneal tumor (arrows) with an ill-defined reticular pattern. Note the tumor has a density lower than the adjacent muscle, simulating a cyst on unenhanced image. The right kidney (arrowheads) is displaced anteriorly and laterally by this tumor. A myxoid liposarcoma is impressed on CT and has been proved by subsequent histological examination of resected tumor specimen.
Key Diagnostic Features
The most common retroperitoneal sarcoma is liposarcoma [1]. On computed tomography (CT), a retroperitoneal tumor containing fat and soft tissue parts suggests a diagnosis of a retroperitoneal liposarcoma [1, 2]. The diagnosis of fat in a tumor on CT is based on its low density which is identical to that of subcutaneous, peritoneal, or retroperitoneal fat by visual inspection. A measured mean density of a region of interest less than −10 Hounsfield units on CT also provides a quantitative way for fat detection. On magnetic resonance image (MRI), fat appears as a high signal intensity region on T1-weighted images (T1WI) and has signal drop on T1-fat-suppressed (T1FS) images [2]. The detectability of gross fat on images of retroperitoneal liposarcomas is somewhat related with histological subtypes [1]. Well-differentiated liposarcoma often has detectable fat on CT or MRI, and other subtypes of liposarcomas may not have detectable fat [1]. On CT, myxoid liposarcomas are characterized by pseudocystic appearance on unenhanced images and increased reticular or swirl enhancement over time on enhanced images [1]. On MRI, myxoid liposarcomas appear as a homogeneous mass of low signal intensity on T1-weighted images and high signal intensity on T2-weighted images (T2WI) [1]. Other subtypes (i.e., pleomorphic and dedifferentiated) of liposarcomas without detectable fat could have similar appearance as other sarcomas [1].
Main Differential Diagnoses
1.
Other retroperitoneal sarcomas
In the absence of detectable fat or imaging characteristics of a myxoid tumor, a retroperitoneal liposarcoma may not be distinguishable from other sarcomas on imaging studies [1].
2.
Angiomyolipomas with retroperitoneal involvement
The presence of aneurysmal dilatation, bridging vessel sign, and linear vascularity in a retroperitoneal fatty tumor with coexisting discrete fatty tumors in the kidney suggests the diagnosis of angiomyolipoma rather than liposarcoma [2].
3.
Retroperitoneal teratoma
Retroperitoneal teratoma is a retroperitoneal tumor containing fat as well. However, retroperitoneal mature teratomas usually have fluid content, fat-fluid layering, and calcifications in addition to fat [1].
7.2 Malignant Fibrous Histiocytoma of the Retroperitoneum
Case 3
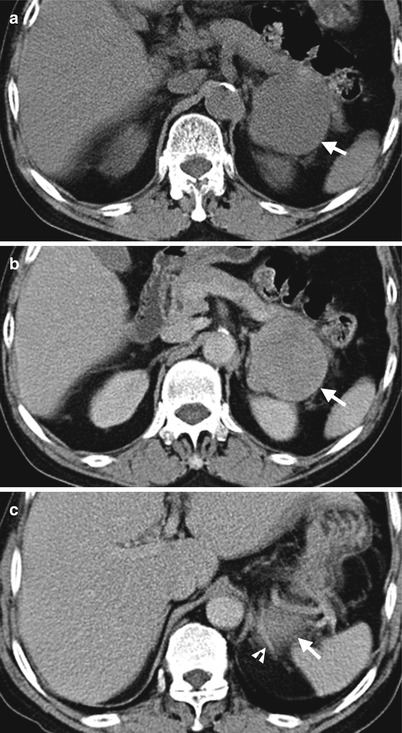
Fig. 7.3
Computed tomography (CT) shows imaging findings of a malignant fibrous histiocytoma (MFHS) in the left retroperitoneum. Unenhanced (Fig. 7.3a) and enhanced (Fig. 7.3b) axial CT at left renal upper pole show a well-defined soft tissue mass (arrows) between the left kidney and pancreatic tail. The left kidney is slightly compressed by this tumor. Enhanced axial CT at the left suprarenal level (Fig. 7.3c) shows this tumor (arrow) abutting lateral limb (arrowhead) of the left adrenal gland. Histological examination shows an MFHS of 8 cm in largest diameter.
Key Diagnostic Features
Malignant fibrous histiocytoma (MFHS) is the third most common retroperitoneal sarcoma [3]. MFHS typically presents as a large well-defined tumor of soft tissue density similar to that of muscle on unenhanced CT and heterogeneous enhancement after contrast medium administration [3]. Necrosis is common in large MFHS [3]. Calcification is occasionally found (7–20 %) in MFHS with reported “ringlike” or “lumpy” appearance [3]. About 40 % of MFHS has close proximity to the kidney with renal invasion, compression, or displacement [3].
Main Differential Diagnoses
1.
Other retroperitoneal sarcomas
On computed tomography (CT), MFHS has a nonspecific picture, which is similar to retroperitoneal leiomyosarcoma or pleomorphic and dedifferentiated liposarcoma [3].
7.3 Retroperitoneal Leiomyosarcoma
Case 4
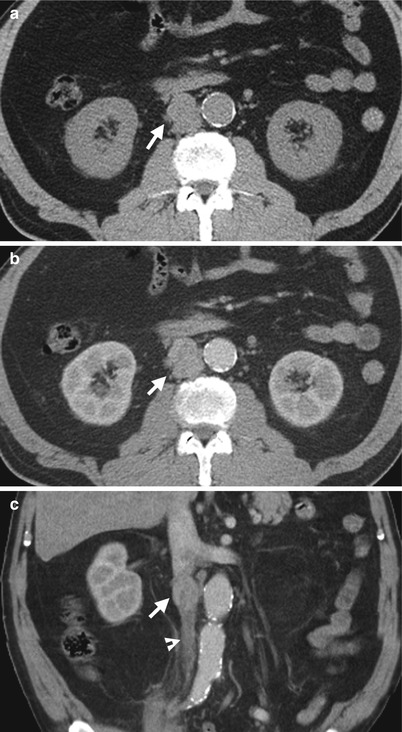
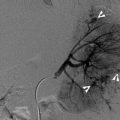
Fig. 7.4
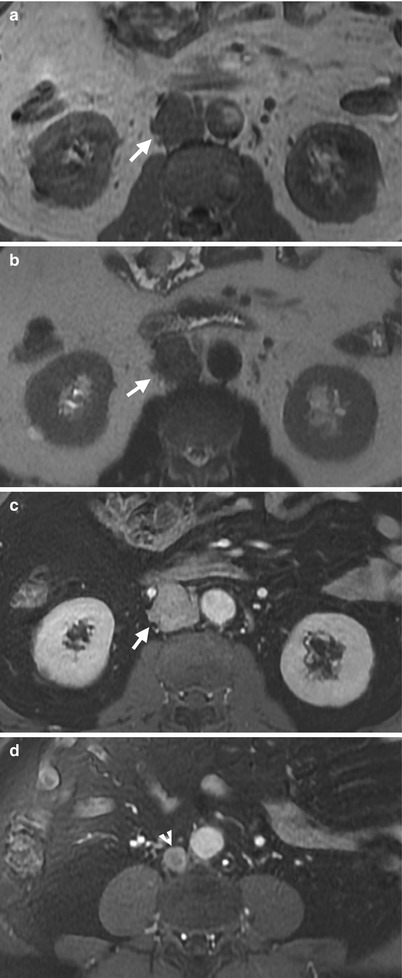
Fig. 7.5
Computed tomography (CT) and magnetic resonance imaging (MRI) show a retroperitoneal leiomyosarcoma with involvement of the inferior vena cava (IVC). Unenhanced (Fig. 7.4a) and enhanced (Fig. 7.4b) axial CT images show a solid tumor (arrows) with irregular profiles and similar density to the muscles. Nearly complete non-visualization of the IVC suggests a tumor involvement. Coronal enhanced CT (Fig. 7.4c) shows ill-defined border between this tumor (arrow) and opacified cranially located IVC as well as a long segment of caudal IVC containing thrombosis (arrowhead). Unenhanced axial T1-weighted image (Fig. 7.5a) and T2-weighted image (Fig. 7.5b) on MRI show low signal intensity of this tumor (arrow) on both pulse sequences. The IVC is completely obliterated by this tumor. Enhanced T1-fat-suppressed image at the kidney (Fig. 7.5c) and lower abdomen (Fig. 7.5d) level shows moderate enhancement of this tumor (arrow) with IVC thrombosis (arrowhead). At surgery, an IVC origin tumor is impressed by tumor involvement of the IVC wall and retrocaval tumor extension with IVC thrombosis. Histological examination reveals a leiomyosarcoma.
Key Diagnostic Features
Leiomyosarcoma (MFHS) is the second most common retroperitoneal sarcoma [3]. Retroperitoneal leiomyosarcomas come from vessels, remnant of Wolffian or Mullerian duct, or spermatic cord [3]. A retroperitoneal tumor with contiguous extension to the vessel (most commonly IVC) on images suggests the diagnosis of a leiomyosarcoma [3]. This is because other sarcomas rarely have intravascular tumor extension [3]. Retroperitoneal leiomyosarcoma without intravascular extension (about 60 % of leiomyosarcomas) usually presents as a large tumor with obvious central necrosis [3] and thus heterogeneous density on CT as well as heterogeneous signal intensity on MRI [1]. On the other hand, leiomyosarcomas of intravascular location in the IVC are usually of smaller sizes without necrosis and have densities similar to muscle on CT [3] as well as low signal intensity on MRI.
7.4 Lymphoma With Retroperitoneal Involvement
Case 5
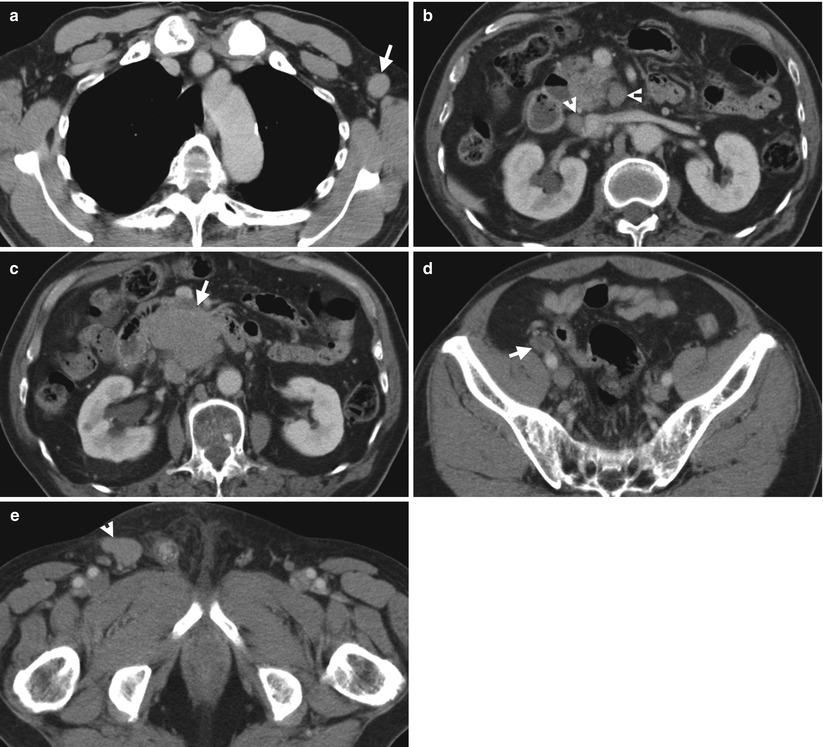
Fig. 7.6
Computed tomography (CT) shows imaging findings of lymphoma with axillary, retroperitoneal, and pelvic cavity involvement. Enhanced axial CT at upper chest level (Fig. 7.6a) shows an enlarged lymph node (arrow) at the left axillary region. Enhanced axial CT at the left renal vein level (Fig. 7.6b) shows two enlarged lymph nodes (arrowheads): one anterior to the inferior vena cava (IVC) and another anterior to the left renal vein. Enhanced axial CT (Fig. 7.6c) at 1.5 cm caudal to Fig. 7.6b shows a large mass (arrow) adjacent to the IVC by confluence of enlarged lymph nodes. Enhanced axial CT at pelvic cavity (Fig. 7.6d) shows a right external iliac lymph node involvement (arrow). Enhanced axial CT at inguinal area (Fig. 7.6e) shows a right inguinal lymph node enlarged (arrowhead). All these findings are consistent with histological evidence of lymphoma by biopsies.
Case 6
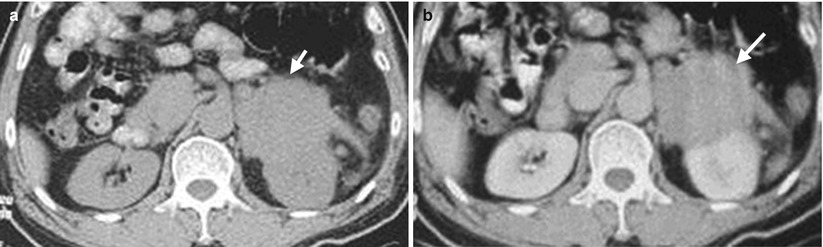
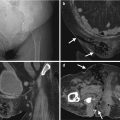
Fig. 7.7
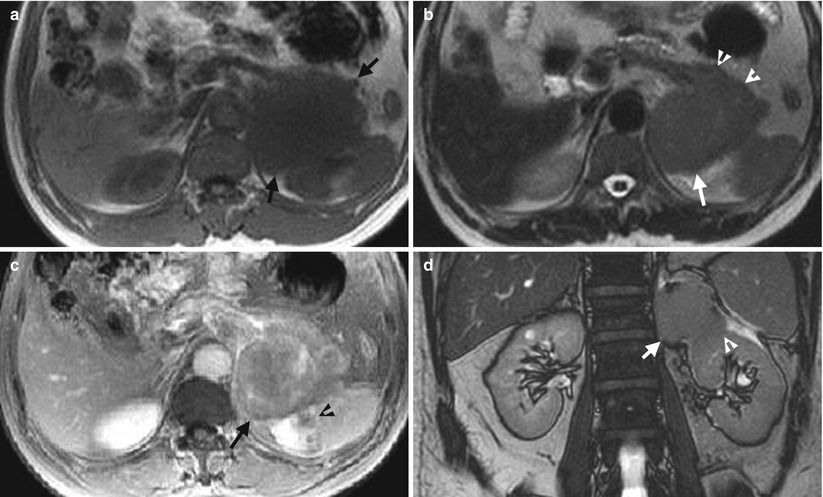
Fig. 7.8
Computed tomography (CT) and magnetic resonance imaging (MRI) illustrate imaging characteristics of a left retroperitoneal lymphoma involving the left retroperitoneal space, left adrenal gland, left kidney, pancreatic tail, and spleen. Unenhanced (Fig. 7.7a) and enhanced CT (Fig. 7.7b) at left renal upper pole level show a left retroperitoneal tumor (arrows) with obliteration of fat plane to left renal upper pole. This tumor has homogeneous density on both unenhanced and enhanced CT images. Unenhanced axial T1-weighted image (Fig. 7.8a) and T2-weighted (Fig. 7.8b) images of MRI show low signal intensity of this tumor (arrows) on both pulse sequences. In contrast to the normal appearance of the right adrenal gland, the left adrenal gland could not be visualized, suggestive of probable left adrenal involvement by this tumor. Pancreatic tail involvement (arrowheads) could be depicted as well. Enhanced axial T1-fat-suppressed image (Fig. 7.8c) shows splenic involvement (arrowhead) by this tumor. Unenhanced coronal image (Fig. 7.8d) shows this tumor (arrow) with heterogeneous enhancement and involvement of the left renal upper pole (arrowhead). There is absence of enlarged lymph node of the abdomen and pelvic cavity on CT and MRI (not shown). A retroperitoneal sarcoma is suspected preoperatively. However, histological examination of the resected tumor reveals a B-cell lymphoma.
Key Diagnostic Features
About one-third of retroperitoneal malignant tumors are lymphomas [3]. Retroperitoneal lymphomas are usually distinguishable from primary retroperitoneal sarcomas [4]. The presence of enlarged lymph node in addition to a dominant retroperitoneal mass suggests the diagnosis of retroperitoneal lymphoma [5]. Para-aortic lymph node involvement is present in about 25 % of non-Hodgkin lymphomas and 55 % of Hodgkin lymphomas [3]. Non-nodal involvement of lymphoma could be depicted on computed tomography (CT) or magnetic resonance imaging (MRI), which is usually present in non-Hodgkin lymphoma and not found in Hodgkin lymphoma [3]. The involved lymph nodes or non-nodal sites of retroperitoneal lymphomas are typically homogeneous soft tissue masses on both unenhanced and enhanced images without necrosis, fatty density, cystic area, or calcifications on CT [3, 4]. Retroperitoneal lymphomas may sometimes have a dominant retroperitoneal mass which has a characteristic growth pattern of tumor extension between and surrounding existing structures (e.g., vessels) and has a homogeneous density as well [2, 3]. On MRI, retroperitoneal lymphomas always present as high signal intensity on diffusion-weighted images by water restriction effect of tumors with high cellularity [5]. The signal intensity on T2-weighted images and enhancement of retroperitoneal lymphomas however vary from homogeneous to heterogeneous appearances [5].
Main Differential Diagnoses
1.
Retroperitoneal sarcomas
A minority (23 %) of non-Hodgkin lymphoma may present as a solitary retroperitoneal mass of large size and heterogeneous density which could be confused with retroperitoneal sarcomas [4]. Image-guided biopsy may help to establish the histological diagnosis of lymphoma and to differentiate from retroperitoneal sarcomas.
7.5 Retroperitoneal Lymph Node Metastasis
Case 7
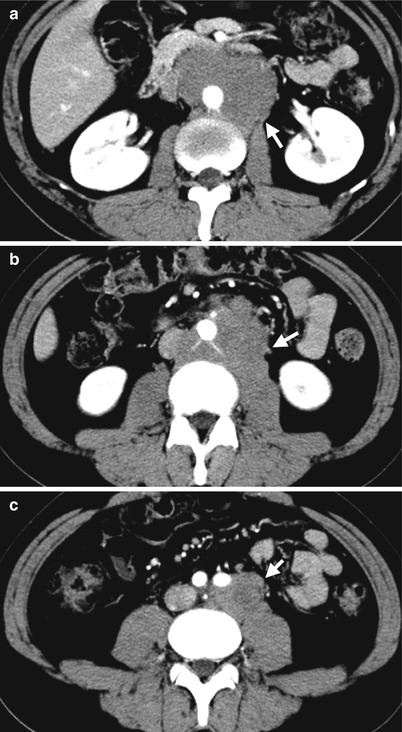
Fig. 7.9
Computed tomography (CT) shows imaging findings of retroperitoneal lymph node metastasis from a testicular seminoma. Enhanced axial CT images at renal midportion level (Fig. 7.9a), renal lower pole level (Fig. 7.9b), and infrarenal level (Fig. 7.9c) show lobulated soft tissue mass (arrows) surrounding the aorta and extending to the aortocaval and left common iliac areas, representing lymph node metastasis from a left testicular seminoma (not shown).
Case 8
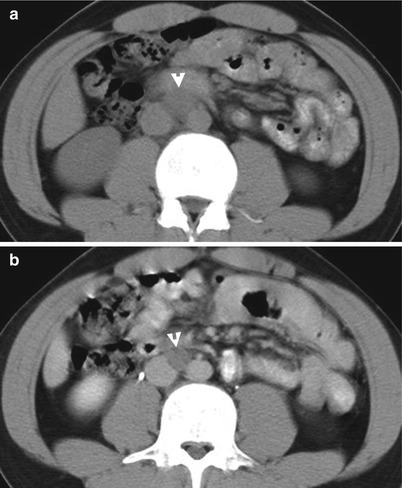
Fig. 7.10
Computed tomography (CT) shows imaging findings of a metastatic lymph node. Unenhanced (Fig. 7.10a) and enhanced (Fig. 7.10b) axial CT images at the right renal lower pole show an enlarged lymph node (arrowheads) between the aorta and inferior vena cava as lymph node metastasis from a mixed germ cell tumor of the right testis.
Key Diagnostic Features
Lymph node metastasis from a primary malignant tumor could appear as a solitary or multiple discrete nodules along the lymphatic drainage, which are easier to be recognized as enlarged lymph nodes by their anatomical locations on computed tomography (CT) or magnetic resonance imaging. On the other hand, lymph node metastasis could present as a large retroperitoneal mass with or without coexisting enlarged discrete lymph nodes as well. Almost any primary malignant tumor could metastasize to the retroperitoneal lymph nodes [3]. Thus, lymph node metastasis should be listed in the differential diagnosis of any retroperitoneal mass, and a search for a primary malignant tumor on images should be done [3]. The testis should be examined and surveyed because retroperitoneal lymph node metastasis from testicular malignancy is common [3].
7.6 Castleman’s Disease
Case 9
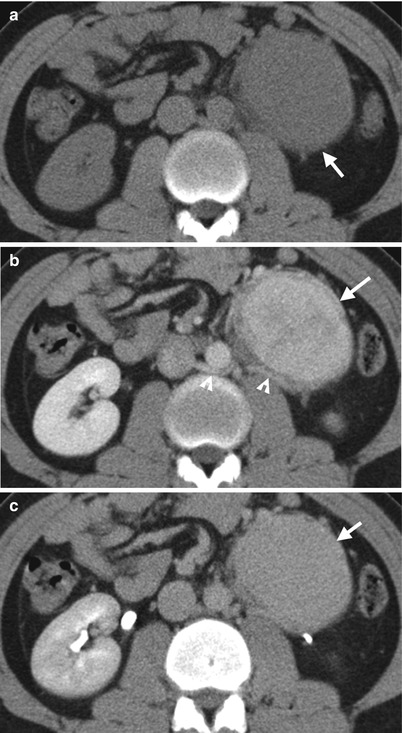
Fig. 7.11
Computed tomography (CT) shows imaging characteristics of Castleman’s disease of hyaline vascular type in the left retroperitoneum. Unenhanced (Fig. 7.11a), enhanced nephrographic phase (Fig. 7.11b), and enhanced excretory phase (Fig. 7.11c) CT images show an oval solid tumor (arrows) at the left para-aortic area of the left retroperitoneum with homogeneous density and enhancement. The tumor adheres to retroaortic left renal vein (arrowheads).
Case 10
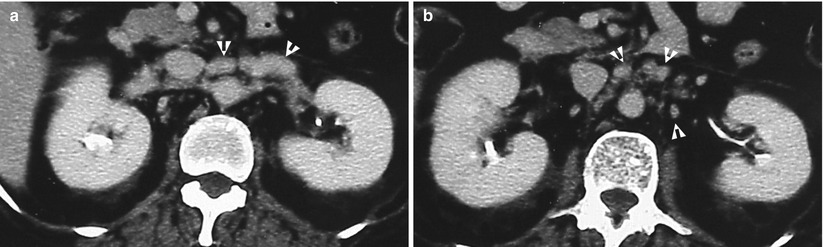
Fig. 7.12
Computed tomography (CT) shows imaging characteristics of Castleman’s disease of plasma cell type. Enhanced renal axial CT images at the right renal upper pole (Fig. 7.12a) and right renal midportion (Fig. 7.12b) show multiple para-aortic lymph nodes (arrowheads) of variable sizes, which have been proved as Castleman’s disease of plasma cell type later.
Key Diagnostic Features
Retroperitoneal Castleman’s disease is rare [6]. Castleman’s disease is most commonly seen in the mediastinum although it could occur in any site of the body with lymphatic tissue [6]. Castleman’s disease is categorized as hyaline vascular type and plasma cell type by histology [6]. By involved solitary or multiple lymph node sites, Castleman’s disease is classified as unicentric and multicentric diseases [7]. Hyaline vascular type of retroperitoneal Castleman’s disease typically shows homogeneous density and homogeneous moderate to strong enhancement on computed tomography (CT), as well as hypointense on T1-weighted image and hyperintense on T2-weighted image on magnetic resonance imaging (MRI) [6, 7]. Hyaline vascular type of retroperitoneal Castleman’s disease typically presents with unicentric disease as a solitary mass [6]. When retroperitoneal Castleman’s disease of hyaline vascular type occurs in pararenal locations, it could have encasement, adhesion, or displacement of the ipsilateral renal pedicles with preservation of vascular patency [6]. Plasma cell type of retroperitoneal Castleman’s disease is even rarer than hyaline vascular type and usually presents with multicentric diseases [6]. Plasma cell type of Castleman’s disease is usually less enhanced than hyaline vascular type.
Main Differential Diagnosis
1.
Retroperitoneal lymphoma
The differentiation of retroperitoneal lymphoma from retroperitoneal Castleman’s disease could be difficult. Of retroperitoneal lymphoma presenting as a solitary mass, it usually has a lobulated, confluent appearance with large size. On the other hand, retroperitoneal Castleman’s disease of unicentric disease is usually a round or oval mass with small size.
7.7 Retroperitoneal Schwannoma
Case 11
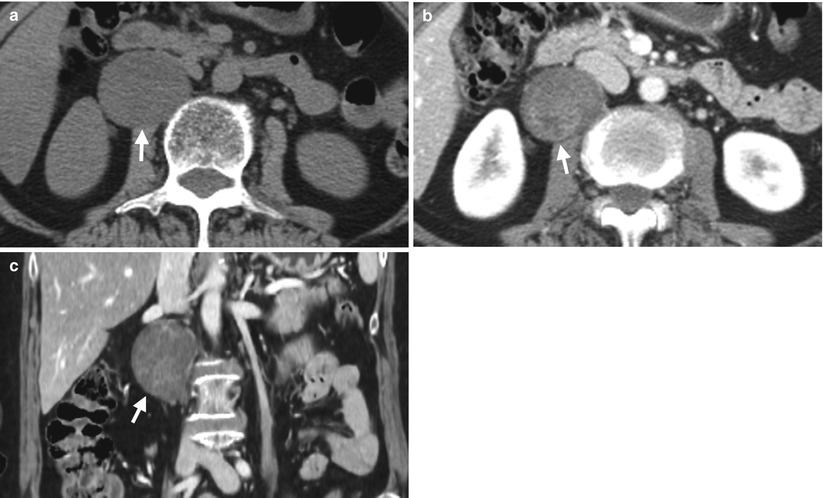
Fig. 7.13
Computed tomography (CT) shows imaging characteristics of a right retroperitoneal schwannoma. Unenhanced axial (Fig. 7.13a), enhanced axial (Fig. 7.13b), and enhanced coronal (Fig. 7.13c) CT images show a well-defined and oval tumor (arrows) at the right paraspinal area. It shows pseudocystic appearance on unenhanced image and ill-defined enhancement after contrast medium administration. Histological examination shows a schwannoma with myxoid change.
Case 12
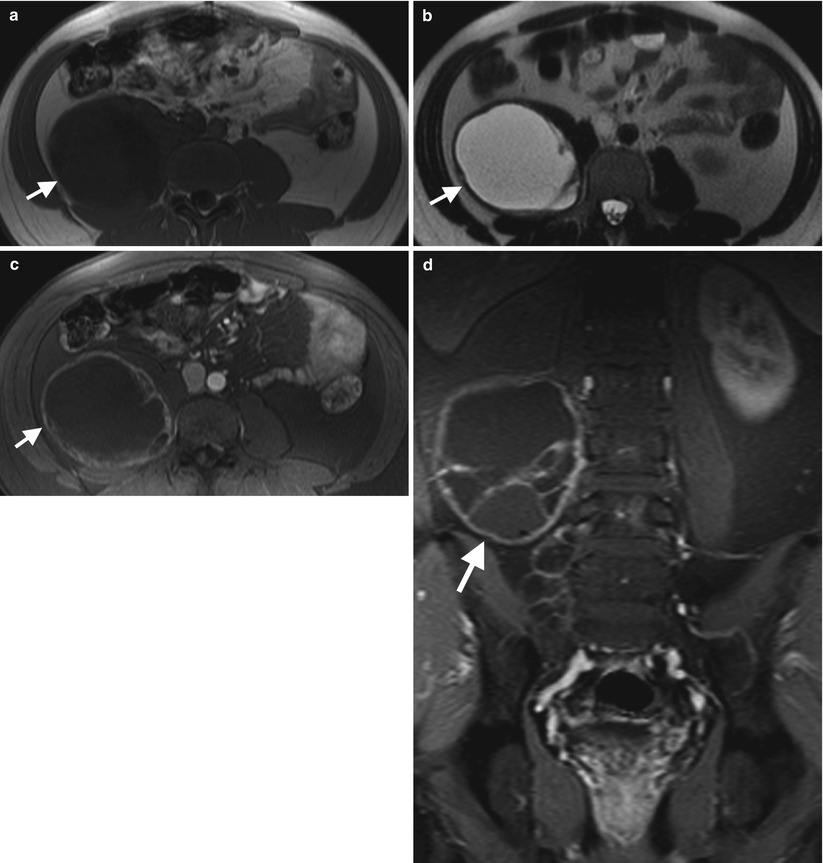
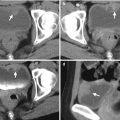
Fig. 7.14
Magnetic resonance imaging (MRI) shows imaging characteristics of a right retroperitoneal schwannoma. Unenhanced axial T1-weighted (Fig. 7.14a) and T2-weighted (Fig. 7.14b) images show a right retroperitoneal tumor with low signal intensity on T1-weighted image and high signal intensity on T2-weighted image, simulating a cyst. Enhanced T1-fat-suppressed images of axial (Fig. 7.14c) and coronal (Fig. 7.14d) scans show enhancement of several septa and irregular wall of this retroperitoneal tumor (arrows). Histological examination of this mass reveals a schwannoma.
Key Diagnostic Features
Schwannoma is also called neurilemoma [3]. Retroperitoneal schwannomas are usually located at paraspinal or presacral areas [3]. On images, retroperitoneal schwannoma usually presents as a round or oval mass with well-defined border without invasion to the adjacent structures by its benign nature [3]. The density, signal intensity, and enhancement of retroperitoneal schwannomas depend on the histological composition [1, 3]. Retroperitoneal schwannoma with myxoid stroma shows “pseudocystic” appearance on computed tomography (CT) and hyperintense on T2-weighted image of magnetic resonance imaging (MRI). Areas of cystic degeneration in retroperitoneal schwannomas show non-enhancing low density on CT, low signal intensity on T1-weighted image, and high signal intensity on T2-weighted images. The cellular tissue of retroperitoneal schwannomas show low signal intensity on both T1-weighted and T2-weighted images of MRI [1]. Retroperitoneal schwannomas with myxoid stroma or cystic degenerations have heterogeneous enhancement on CT and MRI. Nonetheless, small retroperitoneal schwannomas have more homogeneous enhancement than large ones [1].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree