This article presents the magnetic resonance protocols, imaging features, diagnostic criteria, and complications of commonly encountered emergencies in pancreaticobiliary imaging. Pancreatic trauma, bile leak, acute cholecystitis, biliary obstruction, and pancreatitis are discussed. Various classifications and complications that can arise with these conditions, as well as artifacts that may mimic pathology, are also included.
Key points
- •
Magnetic resonance (MR) plays a role in the evaluation of several acute pancreaticobiliary conditions, including cholecystitis, pancreatitis, biliary obstruction, pancreatic trauma, and bile leak.
- •
Several MR imaging features may be used to assist in diagnosis and classification of pancreatic and biliary emergencies, including specific complications.
- •
Several imaging artifacts and pitfalls exist in the MR imaging of pancreaticobiliary emergencies that can mimic pathology.
Introduction
Acute abdominal symptoms are a common cause of emergency department visits in the United States. According to the results of a 2010 survey, the Department of Health and Human Services reported 7 million emergency department visits for noninjury abdominal pain in 2007 to 2008. Disorders of the biliary system and pancreas constitute a large portion of these conditions, with approximately 250,000 admissions for acute pancreatitis and more than 700,000 emergent cholecystectomies performed annually in the United States. Cross-sectional imaging has become an invaluable tool in the clinicians’ armamentarium to aid in the diagnosis and triage of patients presenting with acute abdominal conditions.
Technological advances in multidetector CT (MDCT) over the past several years, particularly involving the increased speed of acquisition and reduced radiation dose, have made it the workhorse of emergency abdominal imaging. The widespread utility of MDCT in abdominal emergencies is well established.
Despite its secondary role to MDCT, certain clinical scenarios may require evaluation with MR imaging. MR cholangiopancreatography (MRCP), first described in 1991 by Wallner and colleagues, has become an essential tool for imaging the pancreas and biliary system. Heavily T2-weighted images enable rapid and noninvasive evaluation of the biliary tree and localization of pathology. In addition, MR may provide relevant information in patients evaluated for pancreatic or biliary trauma, bile leaks, acute cholecystitis, biliary obstruction, or pancreatitis. When compared with MDCT, MR also offers the distinct advantage of avoiding ionizing radiation.
Introduction
Acute abdominal symptoms are a common cause of emergency department visits in the United States. According to the results of a 2010 survey, the Department of Health and Human Services reported 7 million emergency department visits for noninjury abdominal pain in 2007 to 2008. Disorders of the biliary system and pancreas constitute a large portion of these conditions, with approximately 250,000 admissions for acute pancreatitis and more than 700,000 emergent cholecystectomies performed annually in the United States. Cross-sectional imaging has become an invaluable tool in the clinicians’ armamentarium to aid in the diagnosis and triage of patients presenting with acute abdominal conditions.
Technological advances in multidetector CT (MDCT) over the past several years, particularly involving the increased speed of acquisition and reduced radiation dose, have made it the workhorse of emergency abdominal imaging. The widespread utility of MDCT in abdominal emergencies is well established.
Despite its secondary role to MDCT, certain clinical scenarios may require evaluation with MR imaging. MR cholangiopancreatography (MRCP), first described in 1991 by Wallner and colleagues, has become an essential tool for imaging the pancreas and biliary system. Heavily T2-weighted images enable rapid and noninvasive evaluation of the biliary tree and localization of pathology. In addition, MR may provide relevant information in patients evaluated for pancreatic or biliary trauma, bile leaks, acute cholecystitis, biliary obstruction, or pancreatitis. When compared with MDCT, MR also offers the distinct advantage of avoiding ionizing radiation.
Normal anatomy and imaging technique
The pancreas is a retroperitoneal organ that arises from the endodermal lining of the duodenum. It is formed by fusion of the dorsal and ventral pancreatic buds. The main pancreatic duct (MPD) (duct of Wirsung) drains the body of the pancreas, whereas in some patients the accessory pancreatic duct of Santorini drains into the minor papilla. Certain congenital anomalies can occur that may be relevant in acute abdominal conditions later in life (discussed later).
The 3 components of the portal triad are the hepatic artery, portal vein, and bile duct. The left and right hepatic ducts join shortly after the porta hepatis to form the common hepatic duct. The common hepatic duct joins the cystic duct to form the common bile duct, which runs in parallel to the pancreatic duct until they merge to form the hepatopancreatic ampulla of Vater. Variant ductal anatomy may have implications in diagnosis and clinical management (discussed later).
Imaging Protocols
At the authors’ institution, abdominal MR with MRCP sequences using phased-array surface body or torso coils is standardized ( Table 1 ), but certain modifications may be implemented to address a specific clinical question. The contrast agent of choice at the authors’ institution is gadobenate dimeglumine. In select cases where detection of a ductal leak is required, gadoxetate disodium may be used, with additional delayed hepatocellular phase images acquired 10 to 20 minutes after the injection of contrast. Currently the use of hepatobiliary contrast agents to detect bile leak is off-label. If a hepatocyte specific agent, such as gadoxetate disodium, is administered, MRCP and other T2-weighted sequences must be acquired prior to contrast administration to prevent T2 shortening in the biliary tree (discussed later).
| Parameter | T1-weighted In-phase and Out-of-phase | T2-weighted SPIR | T2-weighted Single-shot Turbo Spin-echo | Diffusion (b = 0, 600 s/mm 2 ) | Magnetic Resonance Cholangiopancreatography | T1-weighted 3-D Gradient-recalled Echo SPIR (THRIVE) |
|---|---|---|---|---|---|---|
| Field of view, mm | 400 | 400 | 400 | 400 | 300 | 400 |
| Technique | Gradient-recalled echo | Fast spin-echo | Fast spin-echo | Diffusion | Fast spin-echo for 2-D, 3-D TSE for 3-D | Gradient-recalled echo |
| Scanning mode | Multisection, dual-echo | Multisection | Multisection, 2-D | Multisection, 2-D | Multisection, 2-D or 3-D | 3-D |
| Repetition time (ms) | 180 | 2000 | ∞ | 3.6 | 8000 | 3.6 |
| Echo time (ms) | 2.3 (out of phase)/4.6 (in phase) | 80 | 80 | 1.8 | 800 | 1.7 |
| Section thickness (mm) | 5 | 5 | 5 | 7 | 40 for 2-D, 1.6 for 3-D | 4 |
| Flip angle | 90 | 90 | 90 | 60 | 90 | 15 |
| Sense reduction factor | 1.8 | 2 | 2 | 2 | 2 | 1.7 |
| Respiration control | Breath holding | Respiratory triggering a | Respiratory Triggering a | Respiratory triggering a | Respiratory triggering a | Breath holding |
a May perform with breath-hold technique as tolerated by patient.
In addition, MRCP sequences are typically performed when evaluating for pancreaticobiliary pathology. When feasible, patients are administered a negative oral contrast agent immediately prior to imaging to reduce or eliminate the background signal of the proximal gastrointestinal tract. Prior to its discontinuation, an oral suspension of ferumoxsil was routinely administered in the authors’ department. Subsequently, the authors have switched to oral administration of pineapple juice. MRCP is typically acquired with both 2-D and 3-D techniques in the authors’ department. 2-D MRCP technique is performed using a heavily T2-weighted fat-suppressed single-shot turbo spin-echo (TSE) with 40-mm slice thickness. Six breath-hold or respiratory-triggered images are acquired in the coronal oblique plane at various angles centered about the head of the pancreas. 2-D MRCP images have the advantage of rapid acquisition. 3-D MRCP images are acquired in the coronal plane using a 3-D TSE technique. Although acquisition time is significantly longer than using a 2-D technique, 3-D MRCP imaging allows high-resolution imaging of the biliary tree and the ability to perform multiplanar reconstructions. Maximum intensity projection reformats are acquired in the coronal oblique plane, and additional multiplanar reconstructions may be performed for additional information, including the distinction between choledocholithiasis and air in the duct (discussed later).
Imaging findings and pathology
Pancreatic Trauma
Although MR acquisition times have decreased with advances in technology, MDCT remains the imaging modality of choice in the setting of blunt and penetrating abdominal trauma due to its speed, availability, and high spatial resolution. Select patients with blunt pancreaticobiliary injury on MDCT may benefit, however, from additional MR imaging.
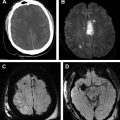
Pancreatic injury in the setting of blunt abdominal trauma is uncommon, with reported incidences ranging from approximately 2% to 12%. The associated mortality is considerable, however, and may be as high as 30% to 50%, largely secondary to concomitant injuries. Factors associated with poor outcomes include a delay in the time to diagnosis, high-grade injury, and disruption of the MPD. Elevated serum amylase may be present, but the clinical presentation of pancreatic injury is variable and nonspecific. Blunt pancreatic injuries occur more commonly in the body of the gland, accounting for two-thirds of cases, and are typically caused by a crushing impact against the vertebral column. Because the main cause for morbidity and mortality is disruption of the MPD, assessment for ductal injuries is critical. Deep lacerations (involving greater than 50% of the thickness of the pancreas) are predictive of ductal disruption and may be detected using T1-weighted postcontrast and T2-weighted sequences. Direct injury to the duct may be visible using T2-weighted sequences, including MRCP images ( Fig. 1 ).
Pancreatic lacerations, defined as irregular linear, low-attenuation regions in the pancreatic parenchyma on MDCT, may be either superficial (when involving <50% of the parenchymal thickness) or deep (>50% of the parenchymal thickness). The sensitivity of MDCT for pancreatic injury is limited, ranging from 47% to 60%. A deep pancreatic laceration is traditionally considered indirect evidence of a MPD injury, and further evaluation with endoscopic retrograde cholangiopancreatography (ERCP) may be warranted if duct integrity is questionable on MR.
Due to the invasive nature of ERCP and its associated complications, particularly in unstable trauma patients, MRCP offers a noninvasive alternative to evaluate the extent of pancreatic injury and MPD involvement. A recent single-center prospective study by Panda and colleagues compared MDCT and MRCP in patients with blunt abdominal trauma using laparotomy as the gold standard. The study found that both MDCT and MRCP performed well in the evaluation of pancreatic injury and suggested that the combination of these modalities increased diagnostic confidence and allowed for more accurate evaluation of MPD involvement. Thus, when pancreatic laceration is suspected, in particular deep lacerations, further evaluation of the MPD with MRCP (if feasible) may be appropriate. Alternatively, an ERCP should be performed.
Bile Leak
Bile leaks may occur after blunt or penetrating hepatic injury or surgical intervention and can present a diagnostic challenge. The lack of specific symptoms may result in a delay in diagnosis. Some of the more common symptoms associated with bile leak include abdominal discomfort, anorexia, and lethargy. Left undiagnosed and untreated, bile leaks can progress to bilomas and bile peritonitis. Eventually, superimposed infection of the intraperitoneal fluid can result in peritonitis and sepsis, often requiring surgical intervention.
Traditionally, hepatobiliary scintigraphy has been used to diagnose bile leaks. Poor anatomic detail and low spatial resolution, however, limit the ability of scintigraphy to precisely localize the source of a bile leak. The addition of single-photon emission CT images may improve the sensitivity and specificity for the detection of leaks but with the disadvantage of increased exposure to ionizing radiation.
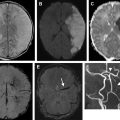
With the advent of gadolinium-based hepatobiliary contrast agents, such as gadoxetate disodium, which has 50% renal excretion and 50% hepatic excretion, MRCP may now play a role in the evaluation of patients with suspected bile leaks. Its use for this purpose is currently off-label, but at least 1 recent study has demonstrated improved detection and localization of bile leaks when compared with traditional MRCP ( Fig. 2 ).
Gadolinium-based hepatobiliary contrast agents result in T1 shortening of excreted bile, rendering it hyperintense on T1-weighted images. Biliary excretion may begin as early as 10 minutes after intravenous contrast administration, and fat-saturated T1-weighted images to assess for bile leak may be acquired at 20 minutes. Key imaging findings include extraluminal accumulation of contrast in the liver parenchyma or around the liver or free spillage into the peritoneal cavity. Secondary signs of bile leak parallel those seen in other imaging modalities, including a collapsed gallbladder, pericholecystic or perihepatic fluid collections, and ascites.
Acute Cholecystitis
Acute cholecystitis is one of the most common surgical emergencies, with a prevalence of approximately 5%. In approximately 90% to 95% of cases, acute cholecystitis is due to gallstone impaction in the neck of the gallbladder or cystic duct. Cholelithiasis is present in approximately 10% of the population, with a higher prevalence seen in middle-aged and elderly women. As a result of the obstruction, bile stasis, ischemia, and development of systemic infection can occur. Because cystic duct obstruction leads to increased intraluminal pressure and the gallbladder wall is weakened by ischemia, subsequent gallbladder perforation can result.
Diagnostic imaging plays a central role in the Tokyo Guidelines, which seek to improve the diagnostic sensitivity and specificity for acute cholecystitis and acute cholangitis. Several imaging modalities are used to assist in the diagnosis of acute cholecystitis, primarily including ultrasound (US), but MDCT and MR imaging may be helpful in select cases. Since its introduction in 1991, MRCP has been an invaluable tool to evaluate the biliary tree.
Imaging features of acute cholecystitis are common to US, MDCT, and MR imaging ( Box 1 ) and include cholelithiasis, gallbladder distention to a diameter greater than 40 mm or length greater than 10 cm, gallbladder wall thickening, pericholecystic fluid, and perihepatic fluid (the so-called C sign). CT and MR imaging may also show hyperenhancement of the adjacent liver on postcontrast arterial-phase images. Although not routinely the first modality of choice due to the speed, accuracy, and low cost of abdominal US, MR imaging is more sensitive for the detection of gallstones impacted in the gallbladder neck or cystic duct. The sensitivity and specificity of MR for detection of cholecystitis when any one of these imaging features is present on MR have been reported at 88% and 89%, respectively ( Fig. 3 ).
- •
Gallbladder distention >40 mm in diameter (or ≥ 10 cm in length)
- •
Gallbladder wall thickening >3 mm
- •
Pericholecystic fluid
- •
Perihepatic fluid (the C sign)
- •
Hyperenhancement of the adjacent liver
Certain forms of cholecystitis also demonstrate unique imaging features and may be readily classified on MR imaging. Emphysematous cholecystitis is a distinct entity and has a different pathogenesis from typical acute calculous cholecystitis. It is more commonly seen in patients with underlying diabetes mellitus and atherosclerotic disease. Small-vessel ischemia results in gallbladder wall inflammation and necrosis, allowing gas to enter the gallbladder wall. Although US and CT are extremely sensitive for detection of air in the gallbladder wall, this finding may also be detectable by MR. Air in the gallbladder wall appears as signal voids. Air may also be visible as susceptibility artifact on gradient-echo imaging. Other imaging features of emphysematous cholecystitis overlap with gangrenous cholecystitis and include irregular wall thickening or asymmetric heterogeneous hyperintense signal in the gallbladder wall on T2-weighted images ( Fig. 4 ).