Magnetic resonance (MR) imaging of the spine is increasingly being used in the evaluation of spinal emergencies because it is highly sensitive and specific in the diagnosis of acute conditions of the spine. The prompt and accurate recognition allows for appropriate medical and surgical intervention. This article reviews the MR imaging features of common emergent conditions, such as spinal trauma, acute disc herniation, infection, and tumors. In addition, we describe common MR imaging sequences, discuss challenges encountered in emergency imaging of the spine, and illustrate multiple mimics of acute conditions.
Key points
- •
Magnetic resonance (MR) imaging of the spine is increasingly being performed for the evaluation of emergent conditions.
- •
MR imaging can readily differentiate between acute and chronic fractures identified by computed tomography (CT), and is sensitive and specific in detecting and describing ligament, disc, and spinal cord injury.
- •
MR imaging is preferred over CT in the evaluation of acute back pain in patients with history of malignancy or infection.
- •
MR imaging protocols should be tailored for a specific indication so as to increase the sensitivity and specificity of the examination, and decrease scan time.
Introduction
The role of MR imaging is expanding in the assessment of patients in the emergent setting. However, MR imaging has several limitations due to its longer scan times, higher expense, and the need for highly trained personnel. For this reason, the radiologist and referring clinicians should discuss the indication for the study before the MR examination.
Also, the familiarization with appropriate MR imaging protocols for specific indications enables an appropriate utilization of MR imaging as a diagnostic tool, provides a higher degree of diagnostic certainty, and avoids unnecessary costs and delays to the patient and referring physician.
Introduction
The role of MR imaging is expanding in the assessment of patients in the emergent setting. However, MR imaging has several limitations due to its longer scan times, higher expense, and the need for highly trained personnel. For this reason, the radiologist and referring clinicians should discuss the indication for the study before the MR examination.
Also, the familiarization with appropriate MR imaging protocols for specific indications enables an appropriate utilization of MR imaging as a diagnostic tool, provides a higher degree of diagnostic certainty, and avoids unnecessary costs and delays to the patient and referring physician.
Protocols and sequences
A detailed patient’s history is essential before the study is started. There are elements that are critically important, such as presence of devices or implants that are contraindicated for an MR examination (eg, electronic spine stimulator devices, cardiac pacers, defibrillators) or that may degrade examination quality (eg, spinal fusion hardware). Others include a history of malignancy or renal insufficiency, a documented history of reactions to gadolinium-based contrast agents, previous spine surgery, and clinical suspicion or risk factors for an infection (eg, current or recent central line use, suspected infections outside the spine, history or suspicion of intravenous drug use, and/or immunocompromised status).
The MR imaging sequences that should be incorporated in the emergency MR imaging spine protocol are listed in Table 1 .
| Sequence | Structures Evaluated | Disease Processes |
|---|---|---|
| T1WI | Bone marrow | Fractures, spine metastases, osteomyelitis |
| Epidural space | Hematoma, abscess | |
| T2WI | Spinal cord | Cord edema/inflammation or demyelination |
| T2WI with fat suppression | Bone marrow | Fractures, bone metastases, osteomyelitis |
| Spinal cord | Cord edema/inflammation or demyelination | |
| Paraspinal soft tissues | Edema/fluid collections | |
| STIR | Alternative to T2W fat suppression sequence | Similar to T2WI-FS |
| PDWI | Spinal cord | Demyelination |
| DWI | Bone marrow | Osteomyelitis/discitis |
| Epidural space | Epidural abscess | |
| Spinal cord | Spinal cord infarction | |
| Anywhere | Neoplasm | |
| T2*-GRE WI | Spinal cord | Hemorrhage (trauma cases) |
| T1WI with contrast and fat suppression | Bone marrow | Osteomyelitis/discitis |
| Metastases | ||
| Epidural space | Epidural phlegmon/abscess | |
| Spinal cord | Active inflammation/demyelination, leptomeningeal or dural metastases | |
| Paraspinal soft tissues | Abscess | |
| Anywhere | Neoplasm |
T1-weighted imaging (T1WI) is used to assess for any osseous abnormalities that may replace or infiltrate the normal fat-containing bone marrow, such as metastasis, edema, or infection. T1WI also provides information regarding the anatomy and signal characteristics of peri-spinal soft tissues.
T2-weighted imaging (T2WI) depicts spinal cord lesions that are hyperintense relative to the surrounding spinal cord and result in effacement of cerebrospinal fluid (CSF). Paraspinal soft tissue edema and fluid collections are best seen on T2WI sequences.
T2-weighted sequences with fat suppression (T2WI-FS) use lipid signal-specific fat suppression to provide accurate suppression of fat signal and excellent anatomic detail. T2WI-FS is sensitive to magnetic field inhomogeneity and may result in suboptimal fat suppression at the interface between air, fat, bone, or in the presence of metallic implants or foreign bodies.
Short tau/T1 inversion recovery (STIR) is a fat-suppression technique that is relatively insensitive to field inhomogeneity, although signal-to-noise ratio is typically decreased relative to T2WI-FS. Signal suppression in STIR is not lipid specific and T1 signal associated with proteinaceous fluid (such as mucous or hemorrhage) also can be suppressed.
Proton density–weighted imaging (PDWI) is best for characterizing T2-hyperintense lesions of the spinal cord that are obscured on heavily T2-weighted acquisitions, and can be added or substituted if cord lesions are of primary clinical concern (eg, multiple sclerosis). PDWI is incorporated into protocols designed to identify disc herniation due to good anatomic detail and spatial resolution.
T2*-weighted gradient-recalled echo imaging (T2*WI or GRE) or newer susceptibility-weighted imaging (SWI) are commonly included in MR imaging spine trauma protocols to increase examination sensitivity for detection of hemosiderin-containing blood products within the spinal cord or epidural space.
Diffusion-weighted imaging (DWI) has a complementary role in the imaging of spinal cord neoplasms, epidural abscesses, and cord infarction, but is not included in the routine emergent spine MR imaging protocol.
Contrast-enhanced T1-weighted fat-suppressed imaging (T1WI-FS + Gd) is useful in patients with history of tumor, infection, or recurrent disc herniation following surgery. Fat suppression is necessary to identify enhancement that would otherwise be obscured or equivocal due to high T1-weighted marrow or paraspinal soft tissue signal. In the spinal cord, T1WI-FS + Gd identifies regions of cord inflammation, active demyelination, or neoplasm.
Selection of a proper field of view (FOV) is a tradeoff between scan time and spatial resolution. A large FOV allows evaluation of multiple spinal levels at a lower spatial resolution in a given time interval, and can be performed in multiple stages with a sagittal view extending from the skull base to the upper thoracic spine, and another from the lower thoracic spine to the lumbosacral junction. Large FOV protocols are indicated for unknown or multiple suspected noncontiguous levels of involvement (eg, metastatic disease to bone, suspected epidural abscess or disseminated osteomyelitis, or multiple age-indeterminate compression fractures). On the other hand, a small FOV is best for evaluating fewer spinal levels at greater spatial resolution in a given time interval.
Magnet field strength in emergent evaluation is less critical. Images acquired at 1.5 T are typically adequate for assessing fractures, cord lesions/hemorrhage, epidural fluid collections, and disc herniation. However, higher field-strength systems (eg, 3.0 T and higher) are increasingly becoming available.
Spine trauma
Trauma is the most common indication for spinal MR imaging. Most spinal injuries are caused by motor vehicle collisions (MVCs), with the remainder resulting from sports-related injuries, falls, and violent acts. Young men are disproportionately commonly affected by spine trauma, although the average age is increasing in most developed countries because of the longer life expectancy of the population.
The incidence of spinal injuries at different segments is related to the anatomic variability of the spinal column. The cervical spine is the shortest in length; however, smaller bone and ligament structures, greater flexibility and articulation, and mass of the head predispose the cervical spine to injury, predominately at the C2 and C6-C7 levels.
The thoracolumbar region (T11-T12 though L3-L4) represents the second most common region of traumatic injury within the spine. Injury is less common at the upper thoracic levels due to the rigid and protective rib cage, and at the lumbosacral junction where osseous and supporting ligamentous structures are more robust. Uncommon patterns of spinal injuries are encountered in patients with predisposing conditions, such as osteopenia, ankylosing spondylitis, metastatic or primary bone lesions, and history of previous spine injury and/or surgery.
Upper cervical spine trauma
Injuries of the upper cervical spine (occiput through C2) may be considered separately from those below the level of C2 because of the unique anatomy of the spine at these levels and the distinct patterns of injury. Cervical spine fractures below the level of C2 (subaxial fractures) are described in terms similar to the thoracic and lumbar levels and are considered separately in the following paragraphs.
- •
Atlanto-occipital and atlanto-axial dislocation-type injuries result from flexion, flexion-distraction, or flexion-rotation mechanisms. This can be seen on multidetector CT (MDCT) or radiography directly or indirectly with the use of several metrics (eg, Powers ratio, basion-dental interval, the basion-posterior axial interval).
However, MR imaging is important in assessing the integrity of the atlanto-occipital ligaments (anterior, posterior, and lateral), atlanto-axial ligaments (anterior and posterior), capsular ligaments, cruciate ligament of the atlas, and alar ligaments of the dens ( Fig. 1 ).
- •
C1 (Jefferson) burst fractures are caused by axial loading of the cervical spine. This represents a fracture of the anterior and posterior arches of C1, as the wedge-shaped lateral masses of C1 are displaced laterally between the larger and more robust occipital condyles and the lateral masses of C2 ( Fig. 2 ). Although the osseous injury is best detected on MDCT, MR imaging is critical for evaluating the involvement of the cruciate ligament of the atlas, which is important in assessing the stability of the injury.
Fig. 2
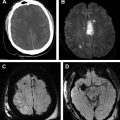
C1 burst fracture (Jefferson): 40-year-old man presents neck pain after MVC. ( A ) Fractures of the anterior and posterior arches of C1 is seen in initial CT. ( B ) T2WI demonstrates large prevertebral fluid hematoma ( white arrowheads ). ( C ) T2WI -FS demonstrates increased signal in the deep soft tissue of the neck posteriorly consistent with interspinous ligament injury ( arrowheads ), and intact tectorial membrane ( arrow ) and posterior atlanto-occipital and atlanto-axial ligaments ( open arrows ). ( D ) PD sequences more clearly depict the intact tectorial membrane ( arrow ) and posterior atlanto-occipital and atlanto-axial ligaments ( open arrows ). The anterior arch of C1 is not seen on the sagittal images due to lateral displacement ( dashed circle ). The anterior arch of C1 is not seen on the sagittal images due to lateral displacement ( dashed circle , B-D ).
- •
Odontoid fractures are caused by flexion or extension injuries, often in conjunction with other injuries of the cervical spine.
An isolated type I odontoid fracture is typically stable and involves the dens above the level of the transverse ligament. A type II odontoid fracture is considered unstable, commonly involves the base of the odontoid process at the junction of the body of C2, and is associated with a high rate of nonunion with conservative, nonoperative management ( Fig. 3 ). A type III odontoid fracture extends from the base of the odontoid inferiorly into the body of C2 and is also considered unstable.
- •
C2 (Hangman) fractures (ie, traumatic spondylolisthesis of C2) are the result of sudden hyperextension and distraction of the head and upper neck with axial loading of the posterior elements of C2. MDCT readily detects pars interarticularis fractures, degree of anterolisthesis, and facet joint dislocation, and is sufficient for commonly used grading systems (ie, Effendi, Levine). Although the fracture is intrinsically unstable, spinal cord injury is uncommon except in high-grade fractures. MR imaging is used to assess injury of the cord, vertebral arteries, ligaments, and evidence of a prevertebral hematoma or marrow edema ( Fig. 4 ).
Fig. 4
Traumatic C2 spondylolysis (“Hangman fracture”): 38-year-old man status post MVC with steering wheel injury to mandible. CT images demonstrate anterior subluxation of C2 with ( A , arrowheads ) bilateral spondylolisthesis ( B , C , circles ) consistent with a “Hangman fracture.” Sagittal MR imaging T2WI-FS ( D , arrowheads ) and spondylolisthesis of C2 ( E , F , circles ). Prevertebral hematoma ( D , black star ) and edema of the interspinous ligaments ( D , arrows ) is present.
Mimic: Chronic compression fractures due to remote trauma or osteopenia with adjacent marrow edema secondary to active disc arthropathy (ie, Modic changes) can mimic acute traumatic marrow edema.
- •
Flexion teardrop and extension- type injuries have similar radiographic and CT features. The primary role of MR imaging is to detect spinal cord injury. In flexion teardrop injuries, anterior compression and posterior distraction causes widening and dislocation of the posterior element and facet joints. The posterior translation of the major fracture fragment with respect to the cervical spine inferiorly, and loss of vertebral body height anteriorly is also seen ( Fig. 5 ).
Fig. 5
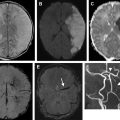
Flexion teardrop fracture, C5 with cord contusion and hemorrhage in a 51-year-old woman following MVC, quadriplegia. Sagittal T2WI ( A ) demonstrates disruption of the cortex of C5 anteriorly and C6 posteriorly, teardrop fragment, disruption of the anterior and posterior longitudinal ligaments ( arrowheads ). There is evidence of cord contusion and hemorrhage ( arrows ) with a prevertebral hematoma from C1 to C5 ( asterisk ). Sagittal STIR ( B ) depicts marrow edema at C5 (black asterisk ), prevertebral hematoma (white asterisk ), interspinous ligament injury ( arrowheads ), and cord swelling with edema. Fluid in the predental space suggests additional injury at the C1-C2 level ( circle ). Sagittal GRE ( C ) confirms cord hemorrhage as central susceptibility within the cord ( white arrows ). Axial T2WI ( D ) at the level of the dens demonstrates disruption of the transverse ligament on the right ( arrow ) and absence of flow void with the left vertebral artery ( arrowhead ) consistent with occlusion.
In extension injuries, anterior distraction and posterior compression forces result in widening of the disc with preserved vertebral body height ( Fig. 6 ).
In equivocal cases, marrow edema involving the posterior elements or anterior longitudinal ligament disruption suggests an extension-type injury. Anterior vertebral body marrow edema or interspinous ligament injury suggests a flexion injury.
Mimic: Incompletely fused anterior endplate osteophytosis, or calcification of the anterior longitudinal ligament, can mimic a teardrop fracture.
Subaxial cervical, thoracic, and lumbar spine trauma
Fractures and ligamentous injuries of the subaxial cervical spine are comparable to fractures of the thoracic and lumbar spine. The “3-column” model divides the osseous and supporting ligamentous structures of the vertebral column into 3 adjacent columns: anterior, middle, and posterior.
The anterior column includes the anterior half of the vertebral body, anterior portion of annulus fibrosis, and the anterior longitudinal ligament. The middle column includes the posterior half of the vertebral body, posterior portion of the annulus fibrosis, and the posterior longitudinal ligament. The posterior column includes the neural arch, facet joints and capsules, and the interspinous ligaments.
Other classification systems, such as the thoracolumbar injury classification severity score, also can be used. This includes description of the morphology, mechanism of injury, and displacement of the spinal column (ie, compression, burst, translational/rotational, or distraction type injuries) and ligamentous injury with the neurologic assessment of injury are all combined to determine a conservative versus operative management.
- •
Compression fractures result from an axial loading or flexion injury. The anterior portion of the vertebral body is most commonly involved resulting in a wedge fracture .
However, fractures may include the superior endplate, inferior endplate, or anterior cortex, and contiguous levels may be involved. Paraspinal hematoma may be present.
If the posterior column is not involved, compression fractures are typically stable and are not associated with acute spinal cord injury. Marrow edema is characteristic, seen as decreased T1WI, increased T2WI-FS, and STIR signal relative to the adjacent marrow. The burst fracture is a more severe injury, involving all 3 columns, often with herniation of the nucleus pulposus into the adjoining endplates, comminuted vertebral body fractures, and loss of vertebral body height. Stability of the vertebral column at the level of injury is determined by the integrity of the anterior and posterior longitudinal ligaments and of the posterior elements, including the facet joints and neural arch and associated ligaments. Posterior displacement of fracture fragments can result in stenosis of the spinal canal ( Fig. 7 ).
- •
Isolated spinous process fractures are usually caused by a direct blow to the dorsal spine ( Fig. 8 ). An evaluation of the interspinous, anterior longitudinal, and posterior longitudinal ligaments is necessary to confirm spinal stability.