Vascular Access
Establishing reliable vascular access in an emergency situation is of critical importance. Many factors, including body habitus, volume depletion, shock, history of injection drug use, congenital deformity, and cardiac arrest, can make obtaining vascular access in the critically ill or injured patient extremely difficult. The introduction of point-of-care ultrasound into emergency and acute care settings has been an important advance for facilitating rapid and successful vascular access.
 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS
For central access, the use of an anatomic landmark-guided approach has been the traditional practice. Internal jugular vein location traditionally relies on the sternocleidomastoid muscle and clavicular landmarks; the femoral vein relies on the inguinal ligament and femoral artery pulsation landmarks; and the subclavian vein relies on clavicular landmarks. In many patients, however, these landmarks may be distorted, obscured, or nonexistent. In addition, normal variations in the anatomic relationship of the internal jugular vein may make cannulation difficult.1 In the emergent situation, attempting central vascular access with poor external landmarks is frequently approached using a “best guess” estimate of the vessel location. This may lead to multiple needle passes to locate the vessel. Excessive bleeding, inadvertent arterial puncture, vessel laceration, pneumothorax, and hemothorax are some of the potential complications of central vascular access. The incidence of complications increases when multiple attempts are required for cannulation.2–5 In patients with an underlying coagulopathy (pathologic or therapeutic), multiple attempts can carry significant morbidity due to hemorrhage.6,7
The introduction of point-of-care ultrasound has been very effective in assisting with the placement of central venous access catheters. For internal jugular vein cannulation, ultrasound use has been described by numerous disciplines, including emergency medicine, critical care medicine, anesthesiology, obstetrics/gynecology, nephrology, surgery, and radiology.2,3,8–10 When compared to the external landmark approach, ultrasound-guided internal jugular vein cannulation results in fewer complications and is more effective in time-to-cannulation and first-attempt success.2,6,11–15 For femoral vein cannulation, the ultrasound-guided approach was found to be more successful than the landmark approach in patients presenting in cardiac arrest.16
Peripheral venous access is less invasive and is used more commonly in the emergency and acute care settings than central access. The inability to find an adequate peripheral vein generally requires that the clinician consider central venous access. Traditionally, successful peripheral venous cannulation requires that a vein first be visualized or palpated. Some peripheral veins that are not readily apparent on the skin surface can be clearly visualized with the use of ultrasound, which may obviate the need for central access.16,17 The basilic and cephalic veins of the arm are superficial veins that are not generally visible but are readily cannulated using ultrasound guidance. Basilic vein cannulation has been shown to be very successful in the ED setting in patients in whom it was difficult to obtain other peripheral vascular access.18 Basilic vein cannulation is readily learned by novice users.19 In addition, basilic veins have been cannulated using ultrasound in patients requiring prolonged outpatient IV access.20
Evidence supporting the use of ultrasound for vascular access has become overwhelming. In 2001, a report published by the Agency for Healthcare Research and Quality (AHRQ) on patient safety in health care included a chapter strongly advocating the use of ultrasound in central venous catheterization.21 The resulting scientific and policy positions favor the use of ultrasound for central venous access stronger than any other point-of-care ultrasound application. The National Institute for Clinical Excellence (NICE) has also recommended that central venous catheters be inserted under ultrasound guidance.22
 CLINICAL INDICATIONS
CLINICAL INDICATIONS
Indications for ultrasound guidance for vascular access are as follows:
 To confirm vessel location prior to landmark-based approach. This is termed as the static approach with ultrasound for IV access. The patient is positioned and the ultrasound transducer is placed on the patient to confirm the predicted landmark-based anatomy. The transducer is then removed, and the patient is prepped for vascular access via the standard landmark-based technique. This can be performed by a single operator and does not require additional adjunctive equipment such as a sterile transducer sleeve. This approach is particularly useful when the patient is unable to assume the standard position for cannulation, when time is of the essence, or when the target vessel is discovered to be large and superficial during the pre-scan phase. One randomized trial demonstrated that the static technique is superior to the traditional landmark technique for central venous cannulation.14
To confirm vessel location prior to landmark-based approach. This is termed as the static approach with ultrasound for IV access. The patient is positioned and the ultrasound transducer is placed on the patient to confirm the predicted landmark-based anatomy. The transducer is then removed, and the patient is prepped for vascular access via the standard landmark-based technique. This can be performed by a single operator and does not require additional adjunctive equipment such as a sterile transducer sleeve. This approach is particularly useful when the patient is unable to assume the standard position for cannulation, when time is of the essence, or when the target vessel is discovered to be large and superficial during the pre-scan phase. One randomized trial demonstrated that the static technique is superior to the traditional landmark technique for central venous cannulation.14
 To assist in real-time cannulation under direct ultrasound visualization. This is termed as the dynamic approach. The ultrasound transducer is inserted into a sterile sleeve and placed on the patient after the sterile prep. The operator can then watch the needle entering the vessel under real-time ultrasound guidance. This technique can involve one or two operators.23 With two operators, real-time vessel visualization can be maintained throughout the entire procedure. With a single operator, ultrasound guidance stops prior to guidewire insertion in order to free up the nondominant hand. The dynamic technique takes full advantage of the benefits of ultrasound-assisted vascular access, and is the approach advocated in the AHRQ report. It should be emphasized that the fine motor skills required for this procedure are not automatic. Practice on models and/or phantoms is recommended in order to achieve steady control of the transducer (with the nondominant hand) while aligning the needle and target within the narrow imaging sector of the probe. Although this method may require more training and patient preparation time, it can save precious minutes when routine landmarks are not evident in the critically ill or injured patient.
To assist in real-time cannulation under direct ultrasound visualization. This is termed as the dynamic approach. The ultrasound transducer is inserted into a sterile sleeve and placed on the patient after the sterile prep. The operator can then watch the needle entering the vessel under real-time ultrasound guidance. This technique can involve one or two operators.23 With two operators, real-time vessel visualization can be maintained throughout the entire procedure. With a single operator, ultrasound guidance stops prior to guidewire insertion in order to free up the nondominant hand. The dynamic technique takes full advantage of the benefits of ultrasound-assisted vascular access, and is the approach advocated in the AHRQ report. It should be emphasized that the fine motor skills required for this procedure are not automatic. Practice on models and/or phantoms is recommended in order to achieve steady control of the transducer (with the nondominant hand) while aligning the needle and target within the narrow imaging sector of the probe. Although this method may require more training and patient preparation time, it can save precious minutes when routine landmarks are not evident in the critically ill or injured patient.
 To minimize the number of vascular access attempts. In certain clinical situations, definitive access is needed in patients at risk for significant complications from multiple vascular attempts. Patients with therapeutic anticoagulation, disseminated intravascular coagulation, thrombocytopenia, hemophilia, or any condition that adds significant risk to vascular access attempts can benefit from the higher first-attempt success rate afforded by ultrasound.
To minimize the number of vascular access attempts. In certain clinical situations, definitive access is needed in patients at risk for significant complications from multiple vascular attempts. Patients with therapeutic anticoagulation, disseminated intravascular coagulation, thrombocytopenia, hemophilia, or any condition that adds significant risk to vascular access attempts can benefit from the higher first-attempt success rate afforded by ultrasound.
 To assist in alternative peripheral access. Alternative peripheral vascular access is important in many patients. Either static or dynamic ultrasound techniques can be used to locate and facilitate cannulation of peripheral vessels. Saphenous, basilic, and cephalic veins are all easily located with ultrasound but difficult to locate with surface visualization. External jugular veins may also be located with ultrasound when anatomic limitations make surface visualization difficult. Some clinical situations require vascular access but choosing a central approach may add unwarranted risk. Ultrasound-guided approach to peripheral veins allows for reliable access without the need for central venous access. This has been shown to be helpful in both adults and children.16,24
To assist in alternative peripheral access. Alternative peripheral vascular access is important in many patients. Either static or dynamic ultrasound techniques can be used to locate and facilitate cannulation of peripheral vessels. Saphenous, basilic, and cephalic veins are all easily located with ultrasound but difficult to locate with surface visualization. External jugular veins may also be located with ultrasound when anatomic limitations make surface visualization difficult. Some clinical situations require vascular access but choosing a central approach may add unwarranted risk. Ultrasound-guided approach to peripheral veins allows for reliable access without the need for central venous access. This has been shown to be helpful in both adults and children.16,24
 To facilitate arterial puncture or cannulation. Ultrasound can be used to locate arteries for puncture or cannulation. Radial, brachial, and femoral arteries are easily located with ultrasound. Both dynamic and static techniques can be used to facilitate arterial puncture.
To facilitate arterial puncture or cannulation. Ultrasound can be used to locate arteries for puncture or cannulation. Radial, brachial, and femoral arteries are easily located with ultrasound. Both dynamic and static techniques can be used to facilitate arterial puncture.
 ANATOMICAL CONSIDERATIONS
ANATOMICAL CONSIDERATIONS
At times it may not be easy to distinguish veins from arteries with B-mode ultrasound. Recognition of key sonographic characteristics can help distinguish veins from arteries. In comparison to arteries, veins have several distinct sonographic features: (1) they are more easily compressed, (2) have thinner walls, and (3) have no arterial pulsation. In addition, central veins possess characteristic triphasic venous pulsations that can be distinguished from arteries. The addition of color flow is a useful adjunct on ultrasound units used for vascular access.
CANNULATION OF THE INTERNAL JUGULAR VEIN
Ultrasound allows for easy localization of the internal jugular vein (Videos 21-1: Central Vascular Access Tips and 21-2: Central Vascular Access Examples). In addition, the carotid artery can be distinguished from the adjacent internal jugular vein. The internal jugular vein lies deep to the sternocleidomastoid muscle and is lateral and superficial to the carotid artery. Using the sternocleidomastoid muscle as the external landmark, the internal jugular vein sits below the bifurcation of the sternal and clavicular heads of the muscle (Figures 21-1 and 21-2). It is important to note that the relative relationship of the carotid artery with the internal jugular vein may change with head position. Specific technical details of internal jugular vein cannulation are provided below.
Figure 21-2. Ultrasound image of the large internal jugular vein and deeper carotid artery. Transducer position (A) and corresponding ultrasound image (B). CA = Carotid artery, IJ = Internal jugular vein.
CANNULATION OF THE SUBCLAVIAN VEIN USING A SUPRACLAVICULAR APPROACH
Placement of a central venous catheter into the subclavian vein at the junction with the internal jugular vein is possible using ultrasound guidance (Figure 21-3A,B). The use of ultrasound for the traditional infraclavicular approach to subclavian vein catheter placement is limited by the large acoustic shadow created by the clavicle in some patients. In contrast, the supraclavicular approach allows for adequate sonographic visualization of the proximal subclavian vein anatomy, and the internal jugular/innominate vein confluence.
Figure 21-3. Placement of the transducer to facilitate visualization of the internal jugular/subclavian vein junction using a supraclavicular approach (A). The transducer should be angled to sweep the view into the upper thorax below the clavicle. Transverse view of the “venous lake” created by the combined subclavian vein and internal jugular vein (B).
CANNULATION OF THE SUBCLAVIAN/AXILLARY VEIN USING AN INFRACLAVICULAR APPROACH
For this approach, place the ultrasound transducer initially just below and in contact with the clavicle. Orient the transducer in long axis over the proximal axillary vein, which travels parallel to the deltopectoral groove. Approach the axillary vein from a more peripheral location near the anterior axillary line if the vein is prominent. Alternately, a more central approach (at the midclavicular line area) will allow the needle/catheter to enter the vein just before it courses below the clavicle to become the subclavian vein. The later approach often requires that the transducer be placed partially over the clavicle so that needle entry for longitudinal (in-plane) visualization is closer to the clavicle (Figure 21-4).
Figure 21-4. Transducer placement for cannulation of the subclavian/axillary vein using the infraclavicular approach. (Courtesy of Michael Blaivas, MD)
CANNULATION OF THE FEMORAL VEIN
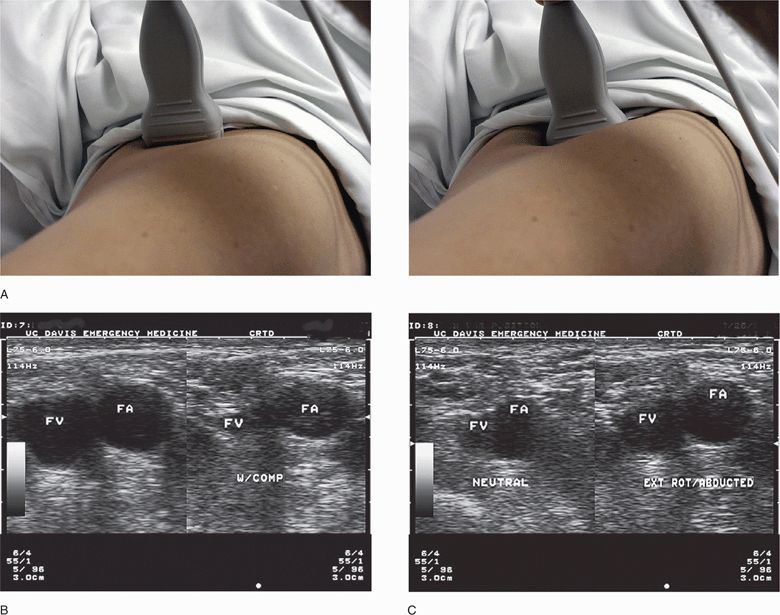
Place the transducer in a transverse position just below the mid-portion of the inguinal ligament. Identification of the key vascular structures begins just below the inguinal ligament and medial to the femoral arterial pulsation. Use the compression technique to distinguish the readily compressible vein from the less compressible artery (Figure 21-5). In addition, appreciating the variable relationships of the vascular structures with respect to limb position is important. Utilize either the static or dynamic technique for femoral vein cannulation. Limit the use of the femoral vein for central venous access in adults to emergency situations because of higher complication rates.21
Figure 21-5. Femoral vein (FV): Gentle pressure is applied to the transducer to identify venous structures by their easy compressibility. (A) FV collapses with compression, and the femoral artery (FA) retains its shape even with compression. (B) FV position is seen to vary with hip abduction and external rotation. (C) In neutral position (left frame), the vein is closely opposed to the FA; however, when the hip is abducted and rotated, the vein is displaced from the artery (right frame). (A, Courtesy of Michael Blaivas, MD)
PERIPHERAL VENOUS CANNULATION
Ultrasound will permit localization of veins that often do not have consistent anatomic relationships or are too deep to be readily palpable (Video 21-3: Peripheral Vascular Access). Of note, the superficial venous structures are easily collapsed with even slight pressure of the transducer on the skin. This feature of collapsibility is useful for distinguishing between veins and arteries. Superficial veins may not be identified, however, if they are collapsed by inadvertent excessive pressure on the transducer. Placing a tourniquet on the extremity to maximize vein dilation is also advisable. Once a suitable vein is identified, the process of IV catheter placement is largely unchanged from standard practice using routinely available venous catheters. With respect to ultrasound guidance in peripheral venous access, either the static or dynamic technique may be successfully utilized. Ultrasound use for peripheral IV access has been shown to decrease the number of needle sticks and time to successful cannulation, and can be readily employed by novice users.16,17
CANNULATION OF THE EXTERNAL JUGULAR VEIN
Since the external jugular vein is superficial, it is often readily identified by visualization and palpation without ultrasound assistance (Figure 21-6). However, limited range of motion (i.e., cervical spine precautions) or adiposity may make this vessel difficult to cannulate without ultrasound guidance.
Figure 21-6. Transverse ultrasound of the external jugular vein (arrow) and internal jugular vein (IJ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS CLINICAL INDICATIONS
CLINICAL INDICATIONS ANATOMICAL CONSIDERATIONS
ANATOMICAL CONSIDERATIONS TECHNIQUE AND NORMAL ULTRASOUND FINDINGS
TECHNIQUE AND NORMAL ULTRASOUND FINDINGS COMMON VARIANTS AND OTHER ABNORMALITIES
COMMON VARIANTS AND OTHER ABNORMALITIES PITFALLS
PITFALLS CASE STUDIES
CASE STUDIES