Diseases of the vascular system encompass a wide range of pathologic conditions with myriad clinical presentations. Appropriate diagnosis and management of these disorders require accurate depiction of the vascular anatomy, its variants, and pathologic abnormalities. Precise assessment of the vascular anatomy has been facilitated by an array of imaging techniques that provide accurate and excellent illustration of the arterial and venous structures. Technologic advances in noninvasive imaging techniques such as multidetector computed tomography (MDCT) and magnetic resonance imaging have opened new paradigms in vascular imaging and have limited the need for invasive catheter angiography. A sound knowledge of vascular anatomy and its variants is crucial for successful practice of vascular imaging. Although detailed description of vascular anatomy and its variants is beyond the scope of this chapter, this discussion describes the salient aspects of vascular anatomy and their variants.
Head And Neck
Arterial System
Common Carotid artery
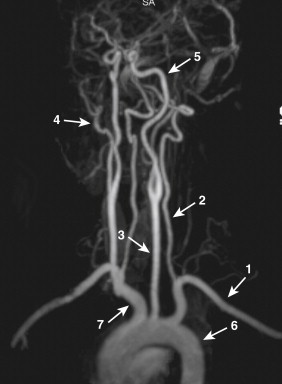
The common carotid arteries (CCAs) represent the main arterial supply of the head and neck ( Fig. 15-1 ). Both CCAs have a similar course and branching pattern within the head and neck but differ in their origin. Whereas the right CCA arises from the brachiocephalic trunk, the left CCA originates from the arch of the aorta. Each CCA divides into two main branches at the level of the upper border of the thyroid cartilage: the external carotid artery (ECA) and the internal carotid artery (ICA).
External Carotid Artery
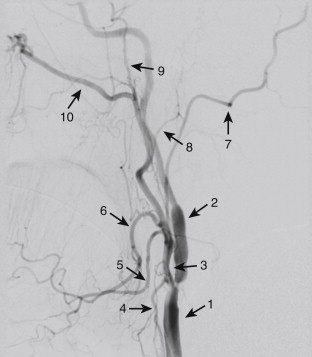
The ECA supplies a greater portion of the neck, the face, and the external portion of the soft tissues of the head ( Fig. 15-2 ). After its origin from the CCA, the ECA has a curved course and terminates by dividing into the maxillary and superficial temporal arteries. Each ECA has eight branches in the head and neck that can be divided as follows: medial branch (ascending pharyngeal), anterior branches (superior thyroid, lingual, and facial), posterior branches (occipital and posterior auricular), and terminal branches (superficial temporal and maxillary).
Internal Carotid Artery
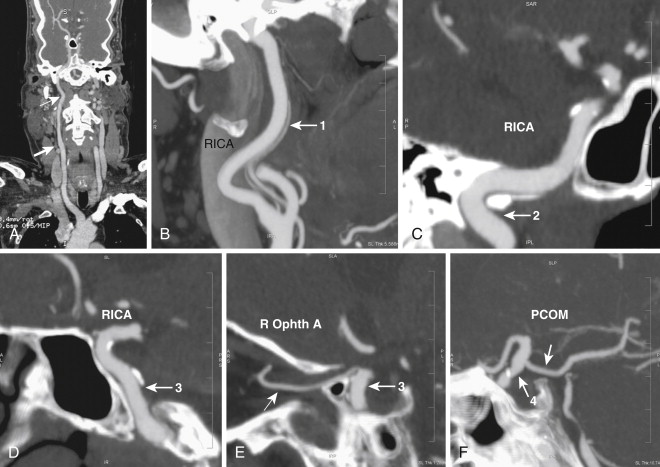
The ICA constitutes the main vascular supply to a greater portion of the brain and the orbital structures ( Fig. 15-3 ). It also supplies a portion of the forehead and the nose. After its origin from the CCA, the ICA has a tortuous course before its termination within the cranial cavity. The ICA has been divided into the following four portions, based on its course: the cervical portion, petrous portion, cavernous portion, and supraclinoid portion. The cervical portion of the ICA does not give any branches. Each ICA gives off the following branches: cervical portion (no branches), petrous portion (caroticotympanic artery and artery of the pterygoid canal), cavernous portion (hypophyseal, cavernous, anterior meningeal, and ophthalmic branch), and supraclinoid portion (anterior cerebral, middle cerebral, posterior communicating, and choroidal branch).
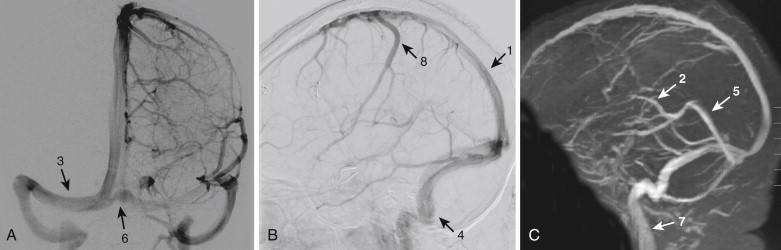
Intracranial Circulation
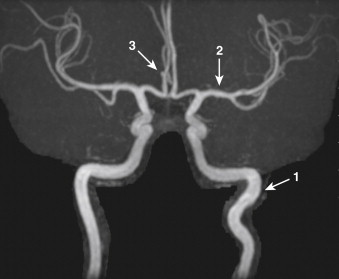
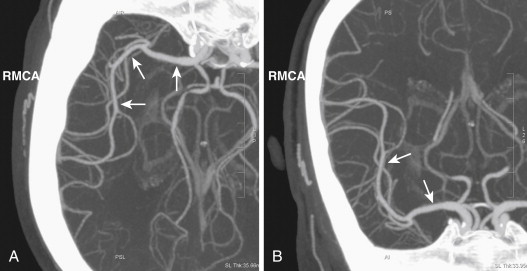
The brain derives its arterial supply from the ICA (through the anterior cerebral artery [ACA] and middle cerebral artery [MCA]) and the vertebral arteries ( Fig. 15-4 ). The ACA arises from the supraclinoid portion of the ICA and runs medially into the longitudinal fissure over the corpus callosum ( Fig. 15-5 ). The right and left ACAs communicate with each other through the anterior communicating artery (ACOM). The ACA gives several branches to the medial portion of the cerebral hemispheres and ends at the posterior aspect of the corpus callosum by anastomosing with the posterior cerebral arteries (PCAs). The MCA, the largest terminal branch of ICA, runs laterally in the sylvian fissure and divides into several branches that supply the lateral portion of the cerebral hemispheres ( Fig. 15-6 ). The posterior communicating artery (PCOM) branch of the ICA runs posteriorly and communicates with the PCA, which is a branch of the basilar artery. The PCOM gives off several branches, which supply the medial surface of the thalami and the walls of the third ventricle. The anterior choroidal branch of the ICA supplies the hippocampus and the tela choroidea and choroid plexus of the third ventricle.
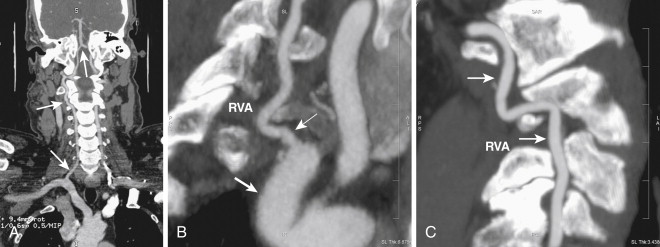
Vertebrobasilar System
The two vertebral arteries on each side along with the basilar artery together form the vertebrobasilar system, which supplies posterior portion of the brain, the cerebellum, and the brainstem ( Fig. 15-7 ). The vertebral arteries arise from the first portion of the subclavian artery on each side. After originating from the subclavian artery, they course for a short interval in the neck and then enter the foramen transversarium of the cervical vertebral bodies. Within the foramen transversarium, the vertebral arteries course cranially in a vertical direction and reach the base of the skull, where they curve to enter the posterior fossa through the foramen magnum and are located anterior to the brainstem. The two vertebral arteries unite at the region of the medulla to form the basilar artery. The basilar artery then courses anterior to the pons and terminates by branching into two PCAs on each side. The vertebrobasilar system has the following branches: the posterior inferior cerebellar artery, which arises from the vertebral artery; the anterior inferior cerebellar artery, which arises from the basilar artery; the superior cerebellar artery; the pontine arteries; and the PCAs ( Fig. 15-8 ).
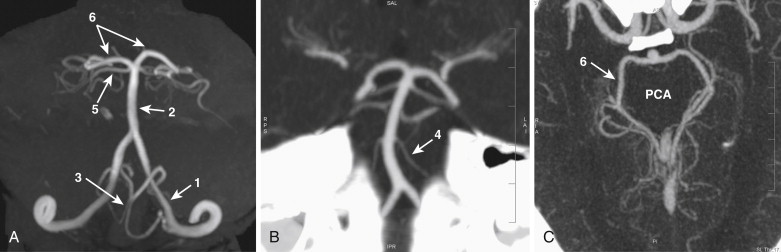
Circle of Willis
The circle of Willis is a tangle of arteries at the base of the brain that forms a crucial anastomotic network between the ICA and the vertebrobasilar arterial systems. The circle of Willis is formed anteriorly by the ACA and the ACOM and posteriorly by the PCA and the PCOM ( Fig. 15-9 ).

Venous System
The venous system of the brain consists of the cerebral and cerebellar veins, which drain into the cranial venous sinuses located within the dura mater. These veins are extremely thin because they lack a muscular wall, and they do not have any valves.
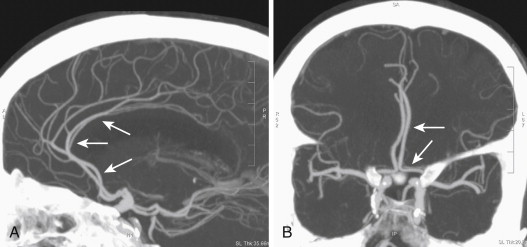
Cerebral Veins
The cerebral veins are broadly classified into the external group (superior cerebral, inferior cerebral, and middle cerebral vein) and the internal group (internal cerebral vein and vein of Galen). The superior cerebral vein drains the superior, lateral, and medial surfaces of the cerebral hemispheres and drains into the superior sagittal sinus. The middle cerebral vein is situated in the sylvian fissure and drains into the cavernous or the sphenoparietal sinus. The middle cerebral vein is connected to the superior sagittal sinus through the great anastomotic vein of Trolard and the transverse sinus through the posterior anastomotic vein of Labbe. The inferior cerebral vein drains the basal portion of the cerebral hemispheres and drains into the superior cerebral veins, middle cerebral veins, or the basal veins. The basal vein is formed by the union of the anterior cerebral vein, the deep middle cerebral vein, and the inferior striate veins. The basal vein travels backward and terminates in the internal cerebral vein. The internal cerebral veins drain the deep parts of the cerebral hemispheres and are formed at the interventricular foramen by the union of the terminal and choroid veins. The internal cerebral veins run backward and, after receiving the basal veins on each side, unite to form the great cerebral vein of Galen. The great cerebral vein ends in the anterior portion of the straight sinus.
Cerebellar Veins
The cerebellar veins consist of the superior and inferior cerebellar veins. The superior cerebellar veins drain into the straight sinus, the transverse sinus, and the superior petrosal sinus, whereas the inferior cerebellar veins drain into the transverse, superior petrosal, and occipital sinuses.
Dural Sinuses
The dural sinuses are venous channels draining the brain. These sinuses are positioned within the two layers of dura mater and are devoid of any valves ( Fig. 15-10 ). The superior sagittal sinus begins at the foramen cecum, travels backward within the convex portion of the midline falx cerebri, and continues as the transverse sinus (usually right). The superior sagittal sinus is triangular in section; it gradually widens as it travels backward from its origin and receives drainage from the superior cerebral veins and diploic veins. Numerous communications exist between the superior sagittal sinus and the veins of the nose and scalp. The inferior sagittal sinus is situated within the posterior half of the free margin of the falx cerebri and terminates in the straight sinus. The straight sinus is located at the line of junction of the falx cerebri situated with the tentorium cerebelli. It begins at the posterior portion of the inferior sagittal sinus, extends backward, and continues as the transverse sinus (the opposite side to the transverse sinus formed by superior sagittal sinus). The straight sinus receives the great cerebral vein and the superior cerebellar veins and communicates with the confluence of sinuses.
The transverse sinus begins at the internal occipital protuberance. On the right side, the transverse sinus usually is a continuation of the superior sagittal sinus, whereas on the left side, it is a continuation of the straight sinus. Each transverse sinus passes laterally and anteriorly along the attached margin of the tentorium cerebelli, curves medially and inferiorly, and continues as the sigmoid sinus before it terminates in the internal jugular vein at the jugular foramen. The transverse sinus formed by the superior sagittal sinus is larger than that formed by the straight sinus. The transverse sinuses receive drainage from the superior petrosal sinuses and from the inferior cerebral and inferior cerebellar veins. The occipital sinus is situated along the attached margin of the falx cerebelli and joins the confluence of the sinuses. The confluence of the sinuses refers to the dilated distal portion of the superior sagittal sinus that is lodged on the internal occipital protuberance. The confluence of sinuses gives rise to the transverse sinus and receives blood from the occipital sinus.
The cavernous sinuses are placed on either side of the body of the sphenoid bone and have a reticulate structure traversed by numerous filaments. The cavernous sinuses contain the ICA and abducent nerve along the medial wall, and several cranial nerves (oculomotor, trochlear, and trigeminal nerve) course along the lateral wall. The cavernous sinuses receive blood from the superior ophthalmic vein and the sphenoparietal sinus, and they communicate with the transverse sinus through the superior petrosal sinus. The bilateral cavernous sinuses communicate through two intercavernous sinuses situated anterior and posterior to the hypophysis cerebri. The superior ophthalmic vein begins at the inner angle of the orbit as the nasofrontal vein and communicates with the angular vein. The inferior ophthalmic vein begins in the floor of the orbit and joins the pterygoid venous plexus before it ends in the cavernous sinus. The superior petrosal sinus connects the transverse sinus with the cavernous sinus and receives cerebellar venous drainage. The inferior petrosal sinus connects the cavernous sinus with the superior bulb of the internal jugular vein and receives venous drainage from the pons, medulla, and cerebellum.
Vertebral Venous System
The vertebral venous plexuses drain the venous blood from the vertebral column, the spinal meninges, and the surrounding musculature. The intercommunicating vertebral venous plexuses are categorized as external (outside vertebral canal) and internal (inside vertebral canal). The external vertebral venous plexuses have anterior and posterior groups that drain the vertebral bodies and posterior vertebral elements, respectively. The external venous plexuses freely communicate with the basivertebral and intervertebral veins. The internal vertebral venous plexuses have paired anterior and posterior groups that receive blood from the bones and spinal medulla. The cranial most portion of the internal venous plexuses forms a complex network of veins at the foramen magnum that communicate with the vertebral veins, the basilar plexus, and the occipital sinus. The internal and external vertebral venous plexuses drain into the intervertebral veins, which terminate in the vertebral, intercostal, lumbar, and lateral sacral veins at the corresponding levels. The spinal medulla is drained by two median longitudinal and four lateral longitudinal veins that form a plexus over the spinal medulla. These veins end in the intervertebral veins at the corresponding level, and at the base of the skull they communicate with the vertebral veins, the inferior cerebellar veins, or the inferior petrosal sinuses.
Thorax
Arterial System
The major arterial structures within the thorax are the aorta and the pulmonary arteries.
Aorta
The intrathoracic portion of the aorta includes the ascending aorta, the arch of aorta, and the descending aorta up to the aortic hiatus in the diaphragm, beyond which it continues as the abdominal aorta.
Ascending Aorta
The ascending aorta begins at the upper part of the left ventricle at the ventricular outflow tract, and its origin is termed the aortic root. The aortic root is situated to the right and posterior relative to the subpulmonary infundibulum. The ascending aorta at its origin has three bulbous dilatations called the aortic sinuses that correspond to the segments of the aortic valve. It then ascends for a short distance and continues as the arch of the aorta. The branches of the ascending aorta include the right and left coronary arteries, which arise in the region of the aortic sinuses.
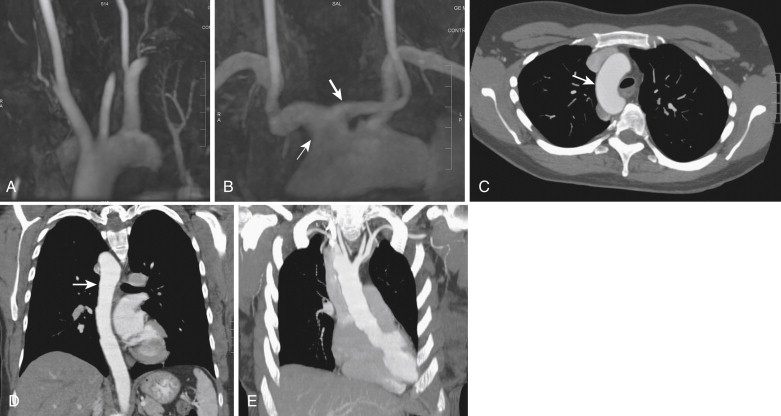
Aortic Arch
The aortic arch curves backward and to the left to continue as the descending thoracic aorta. The three principal branches of the arch of aorta are the brachiocephalic trunk, the left CCA, and the left subclavian artery ( Fig. 15-11 ). The brachiocephalic trunk is the largest branch and divides into the right CCA and the right subclavian artery.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








