Imaging Modalities of The Upper Extremity
Imaging of the arterial and venous systems is an important component of the evaluation in many vascular disorders involving the upper extremity. This chapter provides a brief overview of vascular imaging, including ultrasonography (US), computed tomographic angiography (CTA), magnetic resonance angiography (MRA), and digital subtraction angiography.
Real-time grayscale and color Doppler US is used to evaluate both the arterial and venous systems of the upper extremity. Arterial interrogation may be performed to assess for suspected limb ischemia, arterial stenosis, or patency of a hemodialysis arteriovenous fistula or graft. Assessment of the integrity of the venous side of the dialysis graft or fistula with US is also highly accurate, as is the evaluation of thrombosis or compression of upper extremity veins. US can investigate flow hemodynamics along with vessel lumen and wall morphology. It is, however, operator dependent, does not fully evaluate central thoracic upper extremity arterial inflow and venous anatomy.
CTA has proved to be an adequate imaging modality of upper extremity vasculature. Hellinger et al. proposed four upper extremity CTA protocols: aortic arch with upper extremity runoff, upper extremity runoff, upper extremity indirect computed tomographic venography, and upper extremity direct computed tomographic venography based upon different clinical indications. The authors highlight the various clinical scenarios in which CTA is useful. An update of indications and scan parameters was published several years later in the same journal.
Contrast-enhanced MRA aids in treatment planning and preoperative mapping of various vascular disorders of the upper extremity. It evaluates vascular integrity and patency, which may be compromised in cases of trauma, atherosclerosis, vasculitis, and malignancy. MRA not only defines the site, degree, and extent of stenosis or occlusion but can also demonstrate collateral pathways in these processes. Advantages of contrast-enhanced MRA in the upper extremity include its noninvasive nature, lack of flow artifact, multiangular projection capability, ability to delineate the small vessels of the hand, and the possibility for 4D imaging. Limitations of this imaging technique in the upper extremity include limited coverage of 40 to 50 cm, variable circulation time among individuals, and potential overlapping of the arteries and veins in the hand. Other considerations include the effects of partial volume averaging and susceptibility artifacts, which may lead to an overestimation of stenosis.
Digital subtraction angiography is the gold standard for vascular imaging of the upper extremity; however, it is an invasive procedure and is currently reserved for situations in which clinical questions remain despite information provided by the above-described noninvasive imaging modalities. It may also be used as the primary diagnostic modality when direct hemodynamic analysis is required for treatment planning or when there is intent to perform endovascular intervention in one combined procedure.
Arterial Anatomy of The Upper Extremity
Subclavian Artery
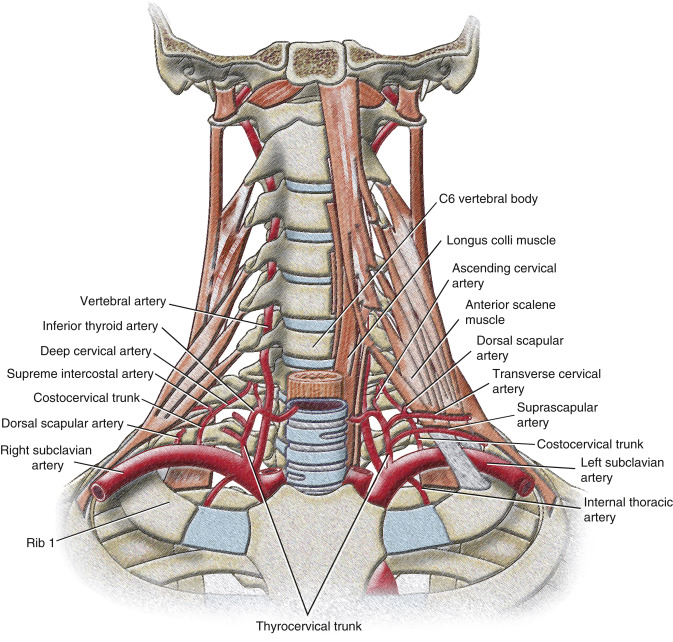
The arterial blood supply of the upper extremity originates with the subclavian artery, whose typical diameter is 8 to 10 mm. The right subclavian artery arises from the brachiocephalic trunk and the left subclavian artery directly from the aortic arch ( Fig. 9.1 ). From its origin to the lateral border of the first rib, the subclavian artery supplies blood to the upper part of the chest, arms, and central nervous system (via the vertebral artery). The subclavian artery is divided into three segments based on its medial, posterior, or lateral relationship to the anterior scalene muscle. The first segment of the right subclavian artery begins at its origin from the brachiocephalic (innominate) trunk posterior to the upper border of the right sternoclavicular joint. It arches superolaterally, passes anterior to the extension of the pleural cavity in the root of the neck, and extends to the medial margin of the right anterior scalene muscle. It ascends 2 to 4 cm above the clavicle. The first segment of the left subclavian artery begins as a direct branch of the aortic arch after the origin of the left common carotid artery at the level of the third and fourth thoracic intervertebral disk spaces. It also ascends into the neck and arches laterally to the medial border of the left anterior scalene muscle. The second segment of the subclavian artery is posterior to the anterior scalene muscle. It is short and the most superior part of the vessel. The third segment descends from the lateral margin of the anterior scalene muscle and extends to the lateral border of the first rib, where it becomes the axillary artery. This portion is the most superficial part of the artery and lies partly in the supraclavicular triangle, the lower and smaller subdivision of the posterior cervical triangle.

Variations in subclavian arterial anatomy are related to its origin and pathway. The right subclavian artery may arise above or below the sternoclavicular level as a distinct aortic arch branch, either the proximal or the distal. When it arises as the proximal branch, it is in the position of a brachiocephalic trunk, as in “classic” anatomy. If it arises as the distal branch off the aortic arch, it ascends obliquely to the right and courses behind the trachea, esophagus, and right common carotid artery. Occasionally, the left subclavian artery is combined at its origin with the left common carotid artery. Other variations in the pathway of the subclavian artery have also been described in relation to the anterior scalene muscle: perforating the muscle or, rarely, passing anterior to it.
Most of the branches of the subclavian artery arise from the artery’s first segment. Its branches include the vertebral artery, thyrocervical trunk, internal thoracic artery, and costocervical trunk ( Fig. 9.2 ). These branches all arise from the first segment of the subclavian artery on the left. On the right, the costocervical trunk usually originates from the second segment of the subclavian artery. Additionally, on either side, the dorsal scapular artery may arise from the third or, less often, the second segment of the subclavian artery or continue as the deep branch of the transverse cervical artery, a branch of the thyrocervical trunk.
Vertebral Artery
In more than 80% of cases, the vertebral artery originates from the superoposterior aspect of the first segment of the subclavian artery as its most proximal and largest branch. The vertebral artery ascends and enters the transverse foramen of the sixth cervical vertebra and continues superiorly through the foramina of the fifth through first cervical vertebrae. At the superior border of the first cervical vertebra, the artery curves medially, crosses the posterior arch of the first cervical vertebra, and passes through the foramen magnum to enter the posterior cranial fossa. The size of the vertebral arteries varies, but a left-dominant artery is more common.
Variations involving the vertebral artery are related to its origin, usually a more proximal one. The left vertebral artery originates from the aortic arch between the left common carotid and the left subclavian artery in up to 5.8% of cases ( Fig. 9.3 ). Its entrance into the cervical transverse foramen is also variable, but it most commonly enters at the level of the fifth or sixth cervical vertebra. Other rare variations involving the left vertebral artery that have been described include an origin from the aortic arch distal to the left subclavian artery, an origin from the left common carotid artery, or an origin from the external carotid artery. In less than 1% of cases, the right vertebral artery originates from the right common carotid artery or the aortic arch.

Thyrocervical Trunk
The thyrocervical trunk is the second branch of the subclavian artery arising from the superior surface distal to the vertebral artery. Near the medial border of the anterior scalene muscle, the thyrocervical trunk classically divides into the inferior thyroid, transverse cervical, and suprascapular arteries. Only slightly more than 50% of individuals have this classic anatomy. Independent origins of these vessels from the subclavian artery are common.
The inferior thyroid artery is the superior continuation of the thyrocervical trunk. It ascends anterior to the anterior scalene muscle and turns medially just below the sixth cervical transverse process. Here it passes anterior to the vertebral vessels and posterior to the carotid sheath and its contents. It finally descends on the longus colli muscle to the inferior pole of the lateral lobe of the thyroid gland.
Branches of the inferior thyroid artery include muscular branches (infrahyoid muscles, longus colli muscle, anterior scalene muscle, and the inferior pharyngeal constrictor) and pharyngeal branches (lower pharynx, thyroid, and parathyroid glands). An important muscular branch is the ascending cervical artery, which arises as the inferior thyroid artery turns medially behind the carotid sheath; it ascends on the anterior surface of the prevertebral muscles, which it supplies, and sends branches to the spinal cord.
The middle branch of the thyrocervical trunk is the transverse cervical artery. This branch passes anterior to the brachial plexus and the anterior scalene muscle, and enters and crosses the base of the posterior triangle. As it reaches the deep surface of the trapezius muscle, it divides into superficial and deep branches. The superficial branch continues on the deep surface of the trapezius muscle, and the deep branch continues on the deep surface of the rhomboid muscles near the medial border of the scapula. Alternatively, these branches may not arise in common as a transverse cervical artery. The superficial branch frequently arises directly from the thyrocervical trunk as a superficial cervical artery, and the deep branch may arise from the third or, less commonly, from the second part of the subclavian artery as the dorsal scapular artery.
The most inferior branch of the thyrocervical trunk is the suprascapular artery. It descends laterally and crosses anterior to the anterior scalene muscle, phrenic nerve, third part of the subclavian artery, and trunks of the brachial plexus. It reaches the superior scapular border, passes above the superior transverse scapular ligament, which separates it from the suprascapular nerve, and enters the supraspinatus fossa. In addition to supplying the supraspinatus and infraspinatus muscles, the suprascapular artery contributes branches to numerous structures along its course. Other alternative origins of the suprascapular artery include a direct origin from the third part of the subclavian artery or as a branch of the internal thoracic artery.
Internal Thoracic Artery
The internal thoracic artery arises from the anteroinferior aspect of the first part of the subclavian artery, directly below the origin of the thyrocervical trunk. It courses anteromedially behind the clavicle and the internal jugular and brachiocephalic veins. It descends behind the first six costal cartilages about 1 cm from the lateral sternal border, divides into numerous intermediate branches, and terminates in the musculophrenic and superior epigastric arteries at the level of the sixth intercostal space.
In the event of thoracic or abdominal aortic stenosis or occlusion, the internal thoracic arteries are important potential sources of collateral blood supply via anterior anastomoses with the intercostal arteries and inferior epigastric arteries, respectively. Additionally, the internal thoracic arteries may provide collateral blood supply to the bronchial arteries.
Costocervical Trunk
The final branch of the subclavian artery in the root of the neck is the costocervical trunk. On the left it arises from the first segment of the subclavian artery, whereas on the right it arises from the second segment. On both sides it arches back above the cervical pleura to the neck of the first rib, where it divides into the deep cervical and supreme intercostal branches. The deep cervical artery anastomoses with the descending branch of the occipital artery and branches of the vertebral artery. In most cases the deep cervical artery arises from the costocervical trunk, but on occasion it may be a separate branch of the subclavian artery. The supreme intercostal artery descends anterior to the first rib and divides to form the posterior intercostal arteries for the first two intercostal spaces.
Clinically relevant scenarios related to stenosis or occlusion of the origin of the subclavian artery involve the potential collateral blood supply, including all the branches of the subclavian and axillary arteries. Subclavian steal, which may be associated with arm pain or central neurologic symptoms, is caused by retrograde flow in the ipsilateral vertebral artery. Additionally, steal physiology may affect other vessels in the upper extremity. For example, reversal of flow can occur in smaller subclavian artery branches such as the thyrocervical trunk and the internal thoracic artery. In patients who undergo cardiac bypass surgery based on an internal thoracic artery, proximal subclavian stenosis can cause a steal phenomenon involving the internal thoracic artery that results in angina.
Axillary Artery
The axillary artery, as a continuation of the subclavian artery, begins at the lateral margin of the first rib and ends normally at the inferior border of the teres major. The axillary artery supplies the walls of the axilla and related regions and continues as the brachial artery, to supply to more distal parts of the upper limb. The axillary artery is also divided into three segments based on its relationship to the pectoralis minor muscle: proximal, posterior, and distal.
Branches of the axillary artery are highly variable in origin, but six branches are generally present ( Fig. 9.4 ). One branch, the superior thoracic artery, originates from the first segment. Two branches, the thoracoacromial and lateral thoracic arteries, originate from the second segment. Three branches, the subscapular, anterior circumflex humeral, and posterior circumflex humeral arteries, originate from the third segment. With the exception of the vertebral artery, all the axillary and subclavian artery branches have potential anastomoses with each other that become apparent in the presence of occlusive disease or vascular tumors.
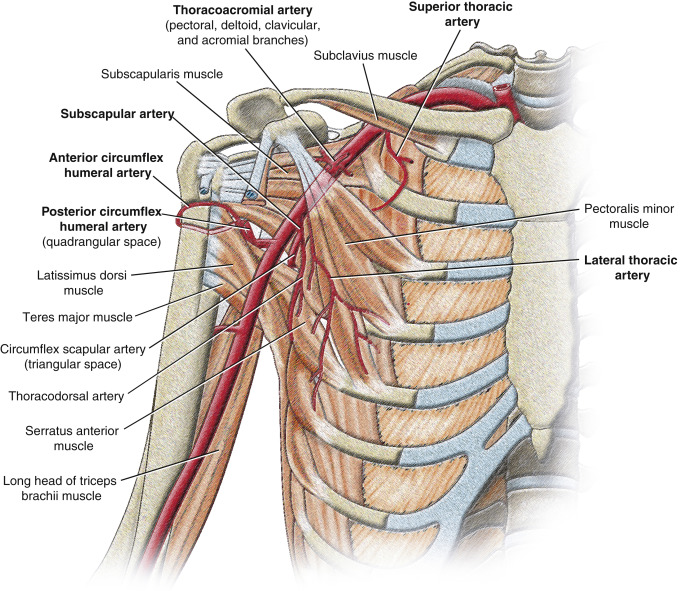
The superior thoracic artery is small and originates from the anterior surface of the first part of the axillary artery near the inferior border of the subclavius muscle. It runs anteromedially above the medial border of the pectoralis minor muscle and then passes between it and the pectoralis major muscle to the thoracic wall. It supplies these muscles and the thoracic wall and anastomoses with the internal thoracic and upper intercostal arteries.
The second segment of the axillary artery gives off two branches, the thoracoacromial and lateral thoracic arteries. The thoracoacromial artery is short and curves around the superior margin of the pectoralis minor muscle. It penetrates the clavipectoral fascia and divides into four branches, the pectoral, deltoid, clavicular, and acromial, that supply the anterior axillary wall and related regions. The pectoral branch contributes vascular supply to the breast as it descends between the pectoral muscles and anastomoses with the intercostal branches of the internal thoracic and lateral thoracic arteries. The deltoid branch often arises with the acromial and crosses the pectoralis minor to accompany the cephalic vein between the pectoralis major and deltoid, both of which it supplies.
The lateral thoracic artery also arises from the anterior surface of the second segment of the axillary artery posterior to the inferolateral margin of the pectoralis minor. It follows the lateral margin of the muscle to the thoracic wall and supplies the serratus anterior and pectoral muscles, axillary lymph nodes, and subscapularis. It anastomoses with the internal thoracic, subscapular, and intercostal arteries and the pectoral branch of the thoracoacromial artery. In females it is large and has lateral thoracic branches that curve around the lateral border of the pectoralis major and contribute to the vascular supply of the breast.
Branches of the third segment of the axillary artery include the subscapular and anterior and posterior circumflex humeral arteries. The subscapular artery, the largest branch, is the major blood supply to the posterior wall of the axilla and contributes to the blood supply of the posterior scapular region. It originates from the posterior surface of the third part of the axillary artery, follows the inferior margin of the subscapularis muscle, and then divides into its two terminal branches, the circumflex scapular and thoracodorsal arteries. The circumflex scapular artery passes through the triangular space between the subscapularis, teres major, and long head of the triceps muscles. It contributes to an anastomotic network of vessels around the scapula and anastomoses with the suprascapular artery and the deep branch (dorsal scapular artery) of the transverse cervical artery ( Fig. 9.5 ). The thoracodorsal artery, which follows the lateral border of the scapula to the inferior angle, contributes to the vascular supply of the posterior and medial walls of the axilla.