Veins of the Abdomen and Pelvis
The external iliac vein is the continuation of the femoral vein; it begins at the inguinal ligament, and joins the internal iliac vein, thereby forming the common iliac vein. The external iliac vein is medial to the iliac artery. This vein is usually valveless.
Tributaries
Inferior epigastric vein
Deep circumflex iliac vein
Pubic vein
Veins of the Pelvis (Figs. 20.1, 20.2)
External Iliac Vein
Internal Iliac Vein (Fig. 20.3)
Internal Iliac Vein (Fig. 20.3)
Several veins converge superiorly in the great sciatic foramen to form the internal iliac vein, to join the external iliac vein, forming the common iliac vein anterior to the sacroiliac joint.
Tributaries
Origin outside the pelvis
Superior gluteal veins
Inferior gluteal veins
Internal pudendal veins
Obturator vein
Anterior to the sacrum
Lateral sacral veins
Origin in visceral venous plexus
Middle rectal veins
Rectal venous plexus
Prostatic venous plexus
Vesical plexus
Dorsal veins of the penis and penile venous plexus
Uterine plexuses
Vaginal plexuses
Superior Gluteal Veins (Fig. 20.4)
Venae comitantes of the superior gluteal artery. These veins enter the pelvis through the greater sciatic foramen, above the muscle piriformis, and join the internal iliac vein as a single trunk.
Inferior Gluteal Veins
Venae comitantes of the inferior gluteal artery. These veins arise proximal and posteriorly in the thigh and anastomose with the medial circumflex femoral and first perforating veins. They enter low in the greater sciatic foramen, joining the internal iliac vein, and connect with the superficial gluteal veins through the gluteal perforating veins.
Internal Pudendal Veins (Fig. 20.5)
Venae comitantes of the internal pudendal artery, commencing in the prostatic venous plexus and ending in the internal iliac vein. These receive veins from the penile bulb and the scrotal (or labial) and inferior rectal veins. The deep dorsal vein of the penis ends in the prostatic plexus, but is connected through that plexus to the internal pudendal veins.
Obturator Vein
This vein commences in the proximal adductor region and enters the pelvis through the obturator foramen, coursing a retroperitoneal path, passing between the ureter and the internal iliac artery to join the internal iliac vein.
These veins are interconnected by the sacral venous plexus and follow the lateral sacral arteries.
Middle Rectal Vein
This vein arises from the rectal venous plexus, receiving tributaries from the bladder, prostate, and seminal vesicle.
The rectal venous plexus surrounds the rectum and is connected anteriorly to the vesical plexus in males and to the uterovaginal plexus in females. It has an internal rectal plexus, under the rectal and anal epithelium, and an external rectal plexus outside the muscular layer. In the anal canal, the internal plexus has longitudinal dilations, most prominent in the left lateral, right anterolateral, and right posterolateral sectors. These veins are apt to become varicose and will be known as
internal hemorrhoids. The internal plexus drains mostly to the superior rectal vein but connects extensively with the external rectal plexus. The external rectal plexus drains inferiorly by the inferior rectal veins, a tributary of the internal pudendal vein. The external rectal plexus drains in the middle to a middle rectal vein, a tributary of the internal iliac vein. The superior rectal vein is the beginning of the inferior mesenteric vein and drains the superior part of the external rectal plexus. The veins in the subcutaneous part of the external rectal plexus may thrombose and form the so-called external hemorrhoids.
internal hemorrhoids. The internal plexus drains mostly to the superior rectal vein but connects extensively with the external rectal plexus. The external rectal plexus drains inferiorly by the inferior rectal veins, a tributary of the internal pudendal vein. The external rectal plexus drains in the middle to a middle rectal vein, a tributary of the internal iliac vein. The superior rectal vein is the beginning of the inferior mesenteric vein and drains the superior part of the external rectal plexus. The veins in the subcutaneous part of the external rectal plexus may thrombose and form the so-called external hemorrhoids.
The wide anastomoses between the rectal venous plexus and the internal iliac vein, as well as with the inferior mesenteric vein, establish communication between the portal and systemic venous systems.
Prostatic Venous Plexus
The periprostatic venous plexus is composed of a superficial and a deep plexus. The deep plexus is popularly known as Santorini plexus. The periprostatic plexus is originated from the deep dorsal vein of the penis, when this vessel leaves the penis under the Buck fascia, and penetrates the pelvis passing under the symphysis of the pubis. After penetrating the pelvis, the vein divides into three major branches: the superficial branch and the right and left deep lateral venous plexuses (Figs. 20.6, 20.7). The superficial branch is centrally located and emerges in the retropubic adipose tissue between the pubic–prostatic ligaments, overlying the bladder neck and the prostate (Figs. 20.8, 20.9). This vein often has communicating branches over the bladder and into the endopelvic fascia (Fig. 20.8). Mostly (80% of cases), this vein is really a single midline vessel, presenting early or late bifurcation in 20% of cases. In 10% of cases this superficial vein may be double or may have other anatomic variations. In 10% of cases, the superficial vein is absent.
The lateral venous plexuses (deep plexus, Santorini) pass posterolaterally, beneath the visceral or preprostatic fascia (Figs. 20.10, 20.11, 20.12) and communicate freely with the internal iliac vein (hypogastric vein) through the pudendal, obturator, and vesical venous plexuses. The deep venous plexus (Santorini plexus) can be visualized in dissected specimens only after opening the endopelvic fascia and its right and left condensations, which unite the prostate to the dorsal surface of the pubis (the so-called “pubic–prostatic ligaments”) (Figs. 20.10, 20.11, 20.12).
Because the lateral plexuses (deep plexus) anastomose freely with other pelvic plexuses, any laceration of this structure can lead to considerable blood loss during any kind of retropubic surgery. In addition, although the periprostatic plexus communicates with the paravertebral venous network (Batson plexus), osseous metastases constitute the most common form of hematogenous metastasis of prostatic carcinoma, which occurs through this paravertebral plexus. The most frequent sites involved are the pelvic bone, lumbar spine, femora, thoracic spine, and ribs.
Vesical Plexus
The vesical plexus covers the lower bladder and the prostatic base in males and is connected to the prostatic venous plexus in males and to the vaginal venous plexus in females. It is drained by several vesical veins, tributaries of the internal iliac vein.
There is a superficial and a deep dorsal vein of the penis. The superficial dorsal vein of the penis drains the prepuce and skin, and is positioned longitudinally along the penis, draining to the external pudendal veins. The superficial dorsal vein of the penis receives, along its course, flow from the corpora cavernosa penis through circumflex veins. The deep dorsal vein of the penis runs backward in the midline, under the fibrous penile sheath. It receives blood flow from the glans penis and corpora cavernosa penis, through the circumflex veins. It reaches the prostatic venous plexus after dividing into right and left branches, but has also communications with the internal pudendal veins (Figs. 20.11, 20.18, 20.19, 20.20, 20.21, 20.22, 20.23, 20.24). The deep dorsal vein of the penis has a venous valve beneath the symphysis pubis.
The superficial venous system of the penis including the superficial dorsal vein drains into the superficial femoral vein through the external pudendal vein and the saphenous vein (Figs. 20.25, 20.26, 20.27, 20.28).
The corpora cavernosa penis is formed by sinusoids surrounded by smooth muscle and connective tissues with high wall tonus. The sinusoidal vascular space and arterial inflow are limited in the flaccid state. The venous outflow is unimpeded. During erection, after neurostimulation or intracavernosal papaverine injection, the sinusoidal smooth muscle relaxes, and distended sinusoids compress and obstruct peripheral venules against tunica albuginea. Simultaneously, resistance to arterial flow decreases until cavernosal pressure approaches systolic pressure (Chapter 19, Fig. 19.18).
The crura of the corpora cavernosa penis are drained by crural perforating veins, which are tributaries of the internal pudendal veins (Fig. 20.13).
Uterine Plexuses
The uterine venous plexus extends laterally in the broad ligaments, communicating with the ovarian and vaginal plexuses. The uterine plexus is drained by the uterine vein, which is a tributary of the internal iliac vein (Figs. 20.29, 20.30a).
Vaginal Plexuses
The vaginal plexuses connect with the uterine, vesical, and rectal plexuses and are drained by vaginal veins to the internal iliac veins.
Common Iliac Veins
The common iliac vein arises from the junction of the external and the internal iliac veins at the level of the sacroiliac joint. The common iliac vein follows an oblique direction
ending at the level of the fifth lumbar vertebra, joining the contralateral common iliac vein to form the inferior vena cava. The right common iliac vein is almost vertical, whereas the left is oblique and longer. The left common iliac vein crosses behind the right common iliac artery and is sometimes compressed by this vessel. The common iliac vein is joined by the iliolumbar and lateral sacral veins (Figs. 20.1, 20.2).
ending at the level of the fifth lumbar vertebra, joining the contralateral common iliac vein to form the inferior vena cava. The right common iliac vein is almost vertical, whereas the left is oblique and longer. The left common iliac vein crosses behind the right common iliac artery and is sometimes compressed by this vessel. The common iliac vein is joined by the iliolumbar and lateral sacral veins (Figs. 20.1, 20.2).
Variations
The left common iliac vein may ascend left of the aorta to the level of the left renal vein, where it crosses anterior to the aorta to join the inferior vena cava.
Median Sacral Veins
The median sacral veins are companions of the median sacral artery, anterior to the sacrum, joining into a single vein and ending in the left common iliac vein or at the junction of the common iliac veins (Figs. 20.1, 20.4).
Abdominal Veins
The inferior vena cava carries blood from all the structures and abdominal organs, below the diaphragm, being formed by the confluence of the common iliac veins. It follows an upward direction in front of the lumbar spine to the right of the abdominal aorta. The IVC reaches the liver and has an intrahepatic segment, which may be totally encircled by hepatic parenchyma. It reaches the right atrium of the heart, through the tendinous part of the diaphragm. At the entrance of the inferoposterior part of the right atrium, there is a semilunar valve of the inferior vena cava.
Variations
A number of anomalies may occur during the development phase of the inferior vena cava in fetal life. The vein may be totally replaced by two or more vessels, with failure of interconnection between the common iliac veins and persistence of a longitudinal channel on the left, supracardinal, or subcardinal veins. It may also undergo a complete transposition to the left of the aorta.
Collateral Circulation
There is a rich collateral venous network bypassing the inferior vena cava in cases of thrombosis or occlusion, either through a superficial or deep venous network. The superficial system includes the epigastric veins, the circumflex iliac, the lateral thoracic veins, the thoracoepigastric, the internal thoracic, the posterior intercostal, the external pudendal, and lumbovertebral anastomotic veins. The deep system includes the azygos vein, the hemiazygos, and the lumbar veins. The vertebral venous plexus, including the Batson venous plexus, is also in the collateral venous circuit (Figs. 20.33, 20.34).
Tributaries
Tributaries
Lumbar veins
Ascending lumbar veins
Gonadal veins
Renal veins
Suprarenal veins
Inferior phrenic veins
Lumbar Veins
There are four pairs of lumbar veins, draining the lumbar muscles and skin from the abdominal wall. The lumbar veins also drain the vertebral venous plexuses and are connected by the ascending lumbar veins. The left-side lumbar veins are longer and cross behind the abdominal aorta. The first and second lumbar veins may connect to the inferior vena cava, the ascending lumbar veins, or the lumbar azygos vein (Figs. 20.1, 20.33, 20.35).
Ascending Lumbar Veins
The ascending lumbar veins originate from the common iliac veins and make connections between the common iliac veins to the iliolumbar and lumbar veins. They ascend behind the psoas major muscles and in front of the vertebral transverse processes. Cranially they join the subcostal veins and turn medially, forming the azygos vein in the right side and the hemiazygos vein on the left (Fig. 20.35).
Gonadal Veins (Figs. 20.36, 20.37)
Testicular Veins
These veins arise from the posterior aspect of the testis and drain the epididymis to form the pampiniform plexus. They follow the spermatic cord, anteriorly to the ductus deferens, crossing the inguinal ring and the inguinal canal, ascending retroperitoneally close to the ureter, anterior to the psoas major as two or more veins with abundant collaterals and anastomoses, in both sides of the testicular artery. The left testicular vein joins in a single vessel and opens into the left renal vein to form a right angle. The right testicular vein joins in a single vessel and opens in the inferior vena cava just below the right renal vein, forming an acute angle. The testicular veins have several valves that may be nonfunctioning and cause varicoceles on the testis, mainly on the left side.
Ovarian Veins
There is a venous plexus in the broad ligament of the uterus, which communicates with the uterine plexus, from which originate the two ovarian veins in each side, following the path of the ovarian artery and coursing together in each side of the artery, opening at the inferior vena cava on the right and on the left renal vein on the left. These veins have valves and the valvular incompetence may lead to pelvic varices (Figs. 20.30, 20.36, 20.37).
Renal Veins
Intrarenal Veins
In contrast to the arteries, there is free circulation throughout the venous system and, therefore, the veins do not have a segmental model. Nevertheless, the renal venous system presents some anatomic characteristics
that are reasonably constant, and should be known during angiographic examinations.
that are reasonably constant, and should be known during angiographic examinations.
Material of Investigation
Fifty-two three-dimensional endocasts of the kidney-collecting system together with the intrarenal veins were obtained from 26 fresh cadavers of both sexes of patients, who died of causes not related to the urinary tract.
A blue polyester resin (volume approximately 15.0 mL) was injected into the main trunk of the renal vein to fill in the kidney venous tree and a yellow resin into the ureter (about 5.0 mL) to fill in the collecting system, according to the proportions and technique described previously.
Findings
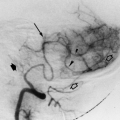
The intrarenal venous arrangement demonstrates free anastomoses between the veins. The small veins of the cortex, called stellate veins, drain into the interlobular veins, which form a series of arches (Figs. 20.38, 20.39). Within the kidney substance, these arches are arranged in arcades, which lie mainly in the longitudinal axis. There are usually three systems of longitudinal anastomotic arcades and the anastomoses occur at different levels: between the stellate veins (more peripherally), between the arcuate veins (at the base of the pyramids), and between the interlobar (infundibular) veins (close to the renal sinus) (Figs. 20.38, 20.39). These anastomoses are named as first order, second order, and third order, from the periphery to the center (Fig. 20.40).
Around the caliceal necks there are large venous anastomoses (collars like), formed mainly when the veins draining the posterior half of the kidney cross over at the necks of the minor calices to join the anterior main trunks (Fig. 20.41). There were also horizontal arches, crossing over the calices to link the anterior and posterior veins, as well as the longitudinal systems at different levels (Fig. 20.42). The venous arcades join one another in both the longitudinal and horizontal planes to produce larger veins that unite to form large trunks. The main renal vein was formed by these trunks, which course toward the hilum where they unite prior to emptying into the vena cava.
In one series, three trunks (28 of 52 casts, 53.8%) and two trunks (15 of 52 casts, 28.8%) joining each other to form the main renal vein were found (Fig. 20.43). Less frequently, four trunks (8 of 52 casts, 15.4%) or five trunks (1 of 52 casts, 1.9%) were found.
Dorsal Kidney
In 36 of 52 casts (69.2%), there was a posterior (retropelvic) vein that coursed on the back of the kidney collecting system, either to drain into the renal vein or to empty directly into the vena cava. In 25 of 52 casts (48.1%), the retropelvic vein had a close relationship with the upper infundibulum or to the junction of the pelvis with the upper calix (Fig. 20.44a). In the other 11 of 52 casts (21.1%), the retropelvic vein crossed and was related to the middle posterior surface of the renal pelvis (Fig. 20.44b). In 16 of 52 casts (30.8%), there were no veins on the posterior aspect of the renal pelvis because the veins draining the posterior region crossed anteriorly to join the main anterior trunks of the renal vein (Fig. 20.44c).
Relationship to Ureteropelvic Junction
In 40.4% of the cases (21 of 52 casts), we found a close relationship between an important tributary of the renal vein and the anterior aspect of the ureteropelvic junction (UPJ) (Fig. 20.45a). Among these cases, there was one vein anterior and another vein posterior to the UPJ, simultaneously (Fig. 20.46a, b). In the other 59.6% of cases (31 of 52 casts), the UPJ was not related to veins, either anteriorly or posteriorly (Fig. 20.45b).
Extrarenal Veins
Mostly, the renal vein is formed by the union of two (53.8% of cases) or three intrarenal trunks (28.8%). Less frequently, there were four trunks (15.4%) or five trunks (1.9%) joining to form the main renal vein. After leaving the renal hilus on each side, both renal veins drain into the inferior vena cava. The left renal vein is longer than the right vein and usually has a higher penetration into the vena cava. The left renal vein has a ventral course in relation to the abdominal aorta and is caudally located in relation to the origin of the superior mesenteric artery.
The right renal vein does not have tributaries. In contrast, the left renal vein drains an extensive body area and usually receives the left inferior suprarenal vein, the left inferior diaphragmatic vein, the left gonadal vein, and the left second lumbar vein.
Anatomic variations of the renal veins are less common than the arterial variations. Also, when anatomic variations do exist, they are more frequent in the right side (Fig. 20.47). The left renal vein almost always is single.
Material of Investigation
The extrarenal veins in 88 “in situ” kidneys were analyzed; these organs were dissected from 44 formalin-fixed cadavers of adult patients, of both sexes, who died of causes unrelated to the urinary tract.
Findings
The left renal vein was single in all of the 44 left kidneys that were analyzed. Considering the right side, in three cases, two renal veins draining to the inferior vena cava were present (7.0% of right kidneys or 3.5% of the total kidneys). Among these, in one case the two veins had similar calibers; the inferior vein was slightly greater in diameter. In the other two cases, the caliber of the inferior vein was less than one half that of the superior vein caliber.
Capsular and Perirenal Veins
There is a rich venous network around the kidneys, draining the renal capsule and with anastomoses between the intrarenal venous system and the capsular veins. The perirenal veins drain into the gonadal vein, inferior phrenic vein, and suprarenal veins. There are direct anastomoses directly with the main renal vein and with the ureteric veins (Figs. 20.1, 20.47).
Suprarenal Veins (See Chapter 18, Fig. 18.140)
There is only one draining adrenal vein for each adrenal hilum. The right adrenal vein is short and small, and opens directly and horizontally into the lateroposterior aspect of the inferior vena cava, far above the right renal vein (Figs. 20.48, 20.49, 20.50).
The left adrenal vein is longer and larger, and descends from the adrenal gland posteriorly to the body of the pancreas to open into the left renal vein, joined by a branch of the left inferior phrenic vein, about 1 cm from the inferior vena cava (Figs. 20.50, 20.51, 20.52).
Angiographically the hepatic veins of the lower group may be mistakenly identified as the right adrenal vein (Fig. 20.53). Occasionally the right adrenal vein drains into one of the small hepatic veins of the lower group.
Inferior Phrenic Veins
The inferior phrenic veins follow the same distribution as that of the companion inferior phrenic arteries on the lower diaphragmatic surface. The right inferior phrenic vein ends in the inferior vena cava, above or together with the right hepatic vein. The left is frequently double and one branch opens in the inferior vena cava or together with the left hepatic vein, whereas the other may join the left adrenal vein or the left renal vein (Fig. 20.54, and Chapter 18, 18.138, 18.139).
Hepatic Veins and Portal Venous System
Hepatic veins
Distribution of the hepatic veins
Variations of the hepatic veins
Collateral channels
Portal vein
Left gastric vein
Right gastric vein
Paraumbilical veins
Cystic veins
Splenic vein
Short gastric veins
Left gastroepiploic vein
Pancreatic veins
Inferior mesenteric vein
Superior rectal veins
Sigmoid veins
Left colic vein
Superior mesenteric vein
Jejunal and ileal veins
Ileocolic veins
Right colic vein
Middle colic vein
Right gastroepiploic
Pancreaticoduodenal veins
Anastomoses between the portal and the systemic circulations
Pancreatic venous system
Hepatic Veins
Distribution of the Hepatic Veins
The hepatic veins drain the liver parenchyma and start as interlobular veins, draining the sinusoids of the hepatic lobules. According to the classical description, these end at the sublobular veins, which will drain into the hepatic veins? The hepatic veins are valveless and are contiguous with the hepatic tissue.
There are three main hepatic veins emerging from the upper, posterior surface of the liver, opening at the inferior vena cava, and an individual vein from the caudate lobe (Figs. 20.55, 20.56, 20.57). These are called the upper group, which consists of the large, right, middle, and left hepatic veins, and the smaller caudate lobe vein, delineating four well-defined territories of drainage (Figs. 20.55, 20.56, 20.57, 20.58).
The right hepatic veins run at the right hepatic fissure, which divides the right hepatic lobe in the anterior and the posterior sectors. The right hepatic vein drains both the anterior (segments VIII and V) and the posterior (segments VI and VII) sectors of the right hepatic lobe (Fig. 20.55).
In 16 of 25 casts of liver specimens, there was only one right hepatic vein of large diameter receiving several tributaries from the several segments of the right lobe (Figs. 20.59, 20.60, 20.61, 20.62, 20.63, 20.64). There is a direct relationship between the right hepatic vein and the bifurcation of the main portal vein and the right branch of the portal vein (Fig. 20.65). Outside the liver the portal vein crosses over the inferior vena cava, and the superior mesenteric vein follows a relatively parallel pathway along the inferior vena cava (Fig. 20.66).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree