Vertebral augmentation techniques use image guidance for the percutaneous placement of spinal implants that stabilize a painful osteoporotic or pathologic vertebral compression fracture. The initial implant, acrylic bone cement, was injected through a bone needle into the vertebral body, a procedure referred to as vertebroplasty. A modification of this procedure, kyphoplasty, entails the temporary use of an inflatable balloon tamp before cement injection. Other techniques and the equipment required to perform these vertebral augmentation procedures have evolved significantly during the past two decades. It is now possible to perform vertebral body reconstruction in patients with painful fractures of compromised vertebrae with excellent outcomes in terms of sustainable pain relief and marked reduction in patient morbidity.
Vertebroplasty and kyphoplasty are both standard-of-care procedures for the treatment of painful osteoporotic and pathologic vertebral compression fractures of the spinal axis. This article reviews the evolution of these treatments in the context of vertebral body reconstruction. Technical developments and improvements in vertebral augmentation are also discussed.
Several decades have passed since the first case of vertebroplasty was performed. Although this case entailed a transoral approach and the target lesion was a painful C2 aggressive hemangioma, a fundamental principle of the vertebroplasty procedure was used, which is pain relief through vertebral body stabilization as a consequence of image-guided bone needle placement and the subsequent injection of acrylic bone cement (polymethylmethacrylate). As shown in numerous prospective and retrospective studies, vertebroplasty is a safe and effective procedure for treating painful osteoporotic or pathologic fractures of the spinal axis. Nearly one decade after percutaneous vertebroplasty (PV) was in use, balloon-assisted vertebroplasty, or kyphoplasty, was developed with the goal of osteoporotic vertebral compression fracture reduction and kyphosis correction. Like vertebroplasty, kyphoplasty entails image-guided percutaneous bone needle placement. A bone needle is placed through either a transpedicular or a parapedicular route from either a bilateral or a unilateral approach. In kyphoplasty, before cement injection, a working cavity is created in the target vertebra by temporarily inflating and then removing a balloon tamp. In acute and early subacute fractures, the balloon tamp is capable of elevating the depressed vertebral endplate. A review of the published literature shows that kyphoplasty is an effective treatment for painful osteoporotic and pathologic vertebral compression fractures. In the more than two decades of the vertebroplasty procedure, thousands of patients have been successfully treated as evidenced by a significant relief of their back pain symptoms, reduction of analgesic use, and return to normal activities of daily living. Furthermore, for those patients who were initially so debilitated that they required hospitalization for pain management, these procedures have resulted in a marked reduction in hospital length of stay, with quick progression to rehabilitation therapy.
(Editor’s Note: There is considerable controversy about whether any real advantage of kyphoplasty over percutaneous vertebroplasty exists. Vertebroplasty is much less expensive and therefore has a decided advantage if no benefit of kyphoplasty otherwise exists. A position paper by multiple societies in Radiology and Neurosurgery concludes “There is no proved advantage of kyphoplasty relative to vertebroplasty with regard to pain relief, vertebral height restoration, or complications.” J Vasc Interv Radiol 2007;18:325–30.)
Vertebroplasty and kyphoplasty are the vertebral augmentation procedures that are used to treat vertebral bodies that are compromised by either an osteoporotic collapse or a neoplastic infiltration. Vertebral augmentation is the stabilization of a damaged vertebra with the placement of an implant (acrylic bone cement as the first approved agent) within the anterior column of the vertebral body. In the specific case of sacroplasty, acrylic bone cement is injected into the sacral ala to augment sacral lesions, such as sacral insufficiency fractures. Kyphoplasty reflected a change not only in the equipment required to perform vertebral augmentation but also in the treatment goal of the procedure, the vertebral compression fracture reduction through vertebral body reconstruction. Vertebral body reconstruction attempts to restore the morphologic and structural integrity of the vertebral body. The damaged vertebra is remodeled before the placement of an implant. The objective of this procedure is to maximally restore the biomechanical properties of the treated vertebra. A working cavity is created within the vertebral body using the balloon tamp and, at times, a curette. Attempts are made to repair and restore the alignment of the vertebral endplates.
Not all vertebral compression fractures are the same. These fractures occur at different locations of the spinal axis, such as the midthoracic spine (T5–T8), the thoracolumbar junction (T10–L2), or the sacrum. These fractures are the result of varying severities of osteoporosis, osteonecrosis, or neoplastic infiltration, all of which compromise the load-bearing trabecular and cortical matrix of the vertebral body. The morphologic and structural alterations that are present can likewise be variable. Furthermore, osteoporotic fractures can be acute, subacute, or chronic. Chronic fractures may have healed, albeit in a deformed state, and may not be an actual source of pain. Similarly, host factors (comorbidities, patient activity level before sustaining the fracture, preexisting spine conditions) in patients with vertebral compression fractures are obviously variable. Given these observations, it is not surprising that several instruments and implants have been developed to treat this less than homogeneous group of patients.
Advances in vertebral body reconstruction techniques can be categorized into 6 major types:
1. Bone access needles
2. Cavity creation devices
3. Coaxial cement conduits
4. Cement delivery systems
5. Implants
6. Pathologic fracture treatment.
These advancements have occurred in an attempt to improve the efficiency, effectiveness, and safety of the vertebral augmentation procedure. The objective of vertebral augmentation, after all, is to place the implant within the vertebral body, avoiding, for example, implant migration such as cement extravasation and providing optimal anterior column stabilization.
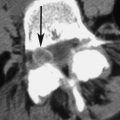
Bone access
Developments in percutaneous bone needle access have focused primarily on curved needles ( Fig. 1 ). These needles have either a fixed curve or an adjustable curve to control directionality. The advantage of curved needle technology is the ability to use only a unilateral approach via a single skin puncture. A second potential advantage of curved needle technology is the selective placement of the needle tip into predetermined target areas of the damaged vertebra, with delivery of the implant to the targets. Because they are deployed through a straight guide cannula or have adjustable curves, these curved needles have somewhat flexible tips that do not always precisely navigate through the vertebral body. Clogging of the needle lumen with hardening cement may occur, requiring removal of the needle. The theoretical potential for breakage of the needle tip or cementing of the needle into the vertebra must be avoided.
Cavity creation
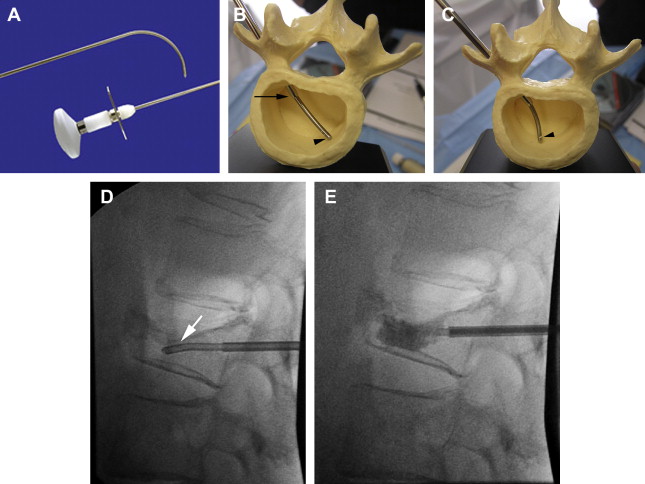
Several devices that can create a working cavity for subsequent implant deposition have been developed for clinical use. The first of these devices, a bone curette, was developed for the kyphoplasty procedure ( Fig. 2 ). This curette possesses an adjustable wedge or mushroom-shaped tip that can be angled up to 90°, in 30° increments, relative to the shaft of the device. The curette, however, must be used with an 8-gauge guide cannula. Another cavity-creation device has a tip that can be variably adjusted to 90° and can be placed through a 10-gauge guide cannula (OpitMed, Ettlingen, Germany). Both of these devices have a built-in fail-safe mechanism that allows the sculpting tip to remain attached in a neutral position, thus allowing device extraction, when the device tip breaks within the sclerotic bone.
Another cavity-creation device uses an adjustable flexible tip with variable angulation; this device must be deployed through a guiding cannula (see Fig. 2 ). Other fixed-tip systems are available for use as well; the smallest of these can be deployed through a 10.5-gauge–sized cannula (see Fig. 2 ). A goal for cavity creation is to facilitate controlled implant delivery. The clear advantage of this maneuver is that it minimizes or prevents extravertebral migration of the implant, in particular cement extravasation with its adverse consequences. Cavity creation is a form of vertebral body remodeling, but in and of itself does not result in correction of vertebral endplate deformities or restoration of vertebral body height loss.
(Editor’s note: There are now reports that cavity creation can actually weaken the bone by removing its residual bone elements compressed during the process of compression fracture. Constructs such as those created with Kyphon may be weaker, and therefore subsequently loose height gained compared to Vertebroplasty; eg, Kim MJ, Lindsey DP, Hannibal M, et al. Vertebroplasty versus kyphoplasty: biomedical behavior under repetitive loading conditions. Spine 2006;31:2079–84) .
Cavity creation
Several devices that can create a working cavity for subsequent implant deposition have been developed for clinical use. The first of these devices, a bone curette, was developed for the kyphoplasty procedure ( Fig. 2 ). This curette possesses an adjustable wedge or mushroom-shaped tip that can be angled up to 90°, in 30° increments, relative to the shaft of the device. The curette, however, must be used with an 8-gauge guide cannula. Another cavity-creation device has a tip that can be variably adjusted to 90° and can be placed through a 10-gauge guide cannula (OpitMed, Ettlingen, Germany). Both of these devices have a built-in fail-safe mechanism that allows the sculpting tip to remain attached in a neutral position, thus allowing device extraction, when the device tip breaks within the sclerotic bone.
Another cavity-creation device uses an adjustable flexible tip with variable angulation; this device must be deployed through a guiding cannula (see Fig. 2 ). Other fixed-tip systems are available for use as well; the smallest of these can be deployed through a 10.5-gauge–sized cannula (see Fig. 2 ). A goal for cavity creation is to facilitate controlled implant delivery. The clear advantage of this maneuver is that it minimizes or prevents extravertebral migration of the implant, in particular cement extravasation with its adverse consequences. Cavity creation is a form of vertebral body remodeling, but in and of itself does not result in correction of vertebral endplate deformities or restoration of vertebral body height loss.
(Editor’s note: There are now reports that cavity creation can actually weaken the bone by removing its residual bone elements compressed during the process of compression fracture. Constructs such as those created with Kyphon may be weaker, and therefore subsequently loose height gained compared to Vertebroplasty; eg, Kim MJ, Lindsey DP, Hannibal M, et al. Vertebroplasty versus kyphoplasty: biomedical behavior under repetitive loading conditions. Spine 2006;31:2079–84) .
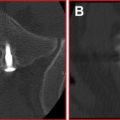
Coaxial cement conduits
Coaxial cement conduits were first used with the kyphoplasty procedure ( Fig. 3 ). These bone-filler devices facilitate controlled implant delivery. In the case of the acrylic bone cement, they prevent obstruction or occlusion of the primary needle cannula with hardened cement. Access to the vertebral body is maintained, and the operator is not pressured to administer acrylic bone cement in a shorter period of time. Alternatively, the operator can use more viscous cement in situations such as closure of endplate defects that require the use of thicker cement. Thirteen-gauge–sized coaxial cement conduits have been developed for use in the vertebroplasty procedure using smaller gauge needle systems, such as a 10.5-gauge cannula ( Fig. 4 ). Stylets or plungers, rather than syringes or hydraulic cement delivery systems, can be used to deliver the thicker cement when necessary. The cement can be delivered in small 0.2 to 0.3 mL aliquots, using an inject-and-step-back method to significantly reduce the operator radiation exposure during cement injection while at the same time avoiding cement leakage. Use of coaxial cement conduits is a viable, efficient, and safe alternative for the injection of acrylic bone cement.