Fig. 16.1
VHSG (volume rendering projection)
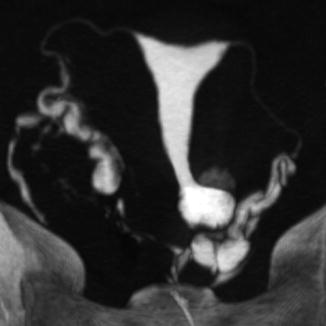
Fig. 16.2
VHSG (maximum intensity projection)
Technical parameters in the CT equipment with either 64 [5] or 256 rows are shown in Table 16.1.
Table 16.1
Technical parameters in CT equipment with 64 vs 256 rows
Technical parameters | 64 rows | 256 rows |
|---|---|---|
Slice thickness | 0.9 | 0.625 |
Reconstruction interval | 0.45 | 0.3 |
KV | 100 | 80 |
mAs | 100–150 | 100–150 |
Scan time acquisition | 5 s | 1.5 s |
Radiation dose (mSv) | 0.9 | 0.3 |
Once the images are acquired, they are transferred to the workstation for different reconstructions: multiplanar reconstruction (MPR), maximal intensity projection (MIP), volume rendering (VR), and endoscopic views.
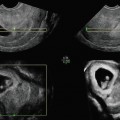
Multiplanar reconstructions (coronal, sagittal, and oblique) allow for the evaluation of the cervix, uterus, and fallopian tubes, as well as extrauterine structures, while the curved MPR evaluates all the female structures in a single plane (Fig. 16.3).
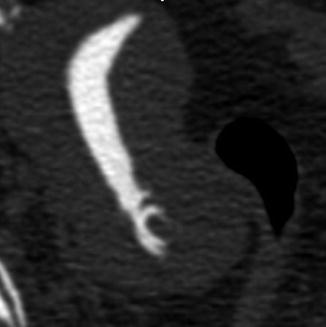
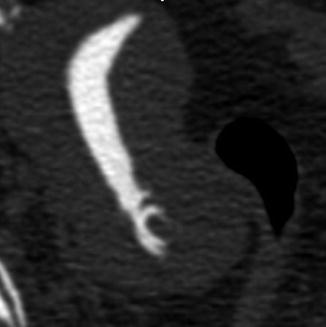
Fig. 16.3
VHSG (multiplanar reconstruction of an endocervical polyp)
Maximal intensity projection (MIP) images provide excellent definition of the fallopian tubes in a tridimensional format with grey tones, detecting the presence of hydrosalpinx and tubal obstructions (Fig. 16.2).
Volume rendering reconstructions provide tridimensional views of the reproductive tract, with a window that recognizes the endoluminal contrast. These reconstructions detect a large spectrum of uterine and tubal pathology such as cervical stenosis, polyps, and tubal disease (Figs. 16.4, 16.5, and 16.6).
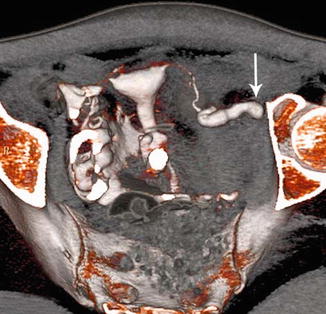
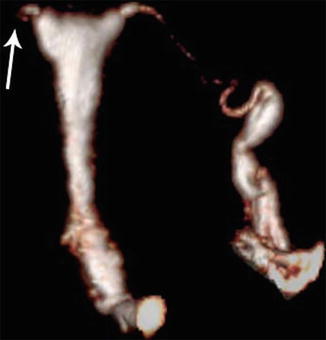
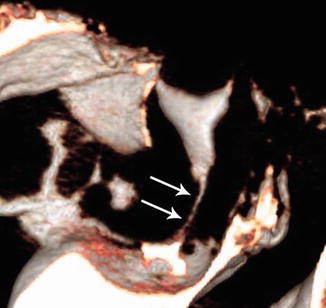
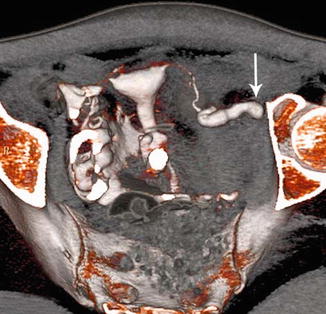
Fig. 16.4
VHSG (volume rendering in tubal disease)
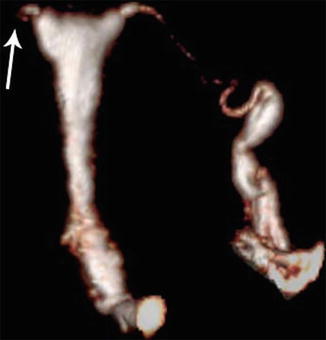
Fig. 16.5
VHSG (volume rendering in tubal disease)
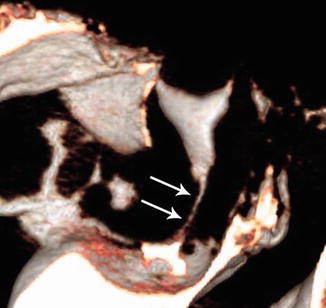
Fig. 16.6
Cervical stricture
Virtual endoscopy algorithm of reprocessing images confirms the findings encountered with the previous methods and provides intraluminal information similar to a conventional hysteroscopy and falloposcopy (Figs. 16.7 and 16.8).
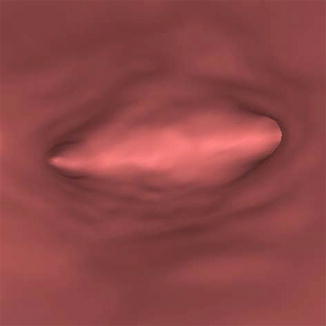
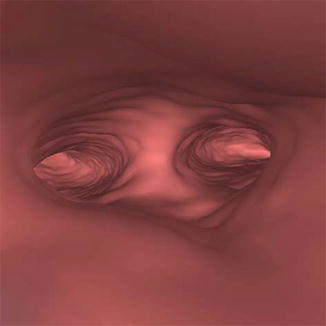
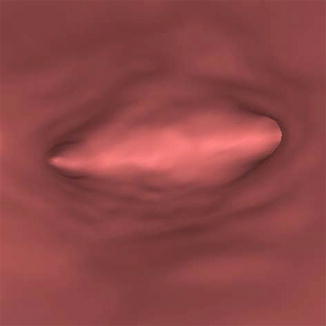
Fig. 16.7
Normal uterine cavity (endoscopy view)
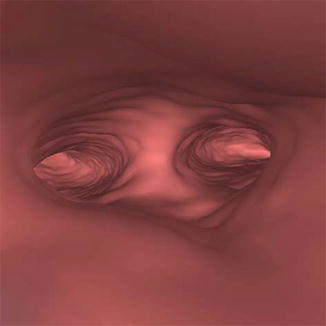
Fig. 16.8
Abnormal uterine cavity (endoscopy view)
The rate of complications with VHSG in our experience is extremely low; in over 7,000 VHSG studies performed since 2006, we did not find any cases of infection, bleeding, or other significant complications requiring hospitalization. In a few cases we observed intravascular passage of contrast, of which only one patient had an allergic reaction requiring medical treatment that improved all symptoms in a very short time.
In known cases of allergy to iodine, we use gadolinium [6], a nonallergenic paramagnetic contrast with a much higher cost (3×) than the iodine contrast and therefore should not be used routinely. We recently performed a comparative study between iodine and gadolinium (n = 50 patients, with 25 in each group) which gave the following results: gadolinium was slightly better tolerated than iodine in terms of discomfort, the density of the intraluminal images was not as intense with gadolinium, and however the overall quality of the studies was fairly similar. In addition, the amounts of radiation exposure (0.9 mSv) for both contrasts used in this particular study were also similar.
The VHSG study [7, 8] is well tolerated by our patients, and they all completed a questionnaire post-procedure to evaluate the degree of discomfort experienced, categorized from grade 0 (no discomfort) to grade IV (very severe discomfort). Over 60 % of the patients had grade 0, 20 % grade I, 16 % grade II, 1.5 % grade III, and 0.5 % grade IV. Interestingly, those patients that previously had a conventional HSG revealed much better acceptance of VHSG compared to those patients that never had a conventional HSG.
Radiation During VHSG: The obvious comparison of the amount of radiation during a VHSG study is with a conventional HSG, which itself varies a great deal depending upon the time of fluoroscopy employed and the number of films taken per study. If, for example, an HSG with 2 min of fluoroscopy and 6 films obtained was performed, it would result in a radiation exposure of 5 mSv. On the other hand, a VHSG with a 256-row multidetector CT using our latest protocols and technical parameters will produce an exposure of only 0.3–0.4 mSv. It is important to emphasize that this remarkable drop in radiation exposure with the use of the latest CT models is accomplished without compromising the quality of the studies performed.
Clinical Experience with Virtual Hysterosalpingography in Reproductive Medicine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree