Wegener Granulomatosis, Lung
Helen T. Winer-Muram, MD
Key Facts
Terminology
Classic Wegener granulomatosis (WG) triad: Sinus, lung, & renal disease
Multisystem disease of unknown etiology characterized by necrotizing granulomatous small-vessel vasculitis
Imaging Findings
Multiple cavitary lung nodules & large airway narrowing
Nodules: Most common manifestation (70%)
Multiple, < 10 in number
Cavitation (50%)
Parenchymal: Ground-glass opacities or consolidation (50%)
Usually represents hemorrhage (seen in 15% of patients with WG)
Wedge-shaped peripheral consolidation: Infarcts or airway involvement
Diffuse ground-glass opacities (“bat wing”) with subpleural sparing
Top Differential Diagnoses
Metastases
Septic Emboli
Pneumonia: Bacterial, Fungal
Pathology
2.4x risk of pulmonary malignancy
50% have pulmonary infection during course of treatment
Clinical Issues
c-ANCA
Sensitivity (90%), specificity (70%)
Median survival without treatment: 5 months
TERMINOLOGY
Abbreviations and Synonyms
Classic Wegener granulomatosis (WG) triad: Sinus, lung, & renal disease
Definitions
Multisystem disease of unknown etiology characterized by necrotizing granulomatous small-vessel vasculitis
Pulmonary involvement occurs at some stage in > 90% of patients (10% lung only)
IMAGING FINDINGS
General Features
Best diagnostic clue: Multiple cavitary lung nodules & large airway narrowing
Patient position/location: Lung nodules tend to be bronchocentric or subpleural & peripheral
Size: Nodules range up to 10 cm
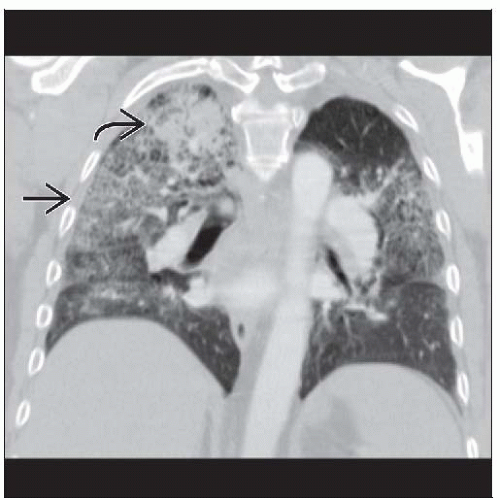
CT Findings
Nodules: Most common manifestation (70%)
Morphology
Multiple (75%), usually < 10 in number, can coalesce into large masses
Usually 2-4 cm, rounded or oval
Margin: Sharp or ill-defined from surrounding hemorrhage
CT halo sign: Nodule with surrounding ground-glass due to hemorrhage
Nodules may be seen with consolidation or ground-glass opacities
Cavitation (50%)
Thick-walled > thin-walled (thin-walled usually chronic)
Inner margin irregular and shaggy; outer margin often spiculated
Air-fluid levels uncommon; however, may contain necrotic debris
Rapid enlargement or air-fluid levels suggest hemorrhage or superinfection
Distribution
Parenchymal: Ground-glass opacities or consolidation (50%)
Usually represents hemorrhage
± Nodules
Various distribution and patterns
Wedge-shaped peripheral consolidation: Infarcts or airway involvement
Focal mass-like
Diffuse ground-glass opacities (“bat wing”) with subpleural sparing
May have “crazy-paving” pattern
May have reverse halo sign
Cavitation (5%)
Adenopathy (15%)
Always associated with parenchymal disease (< 2 cm short axis diameter)
Larger nodes should suggest superimposed infection or malignancy
Pleura (20%)
Thickening or effusion: 20%, pneumothorax rare
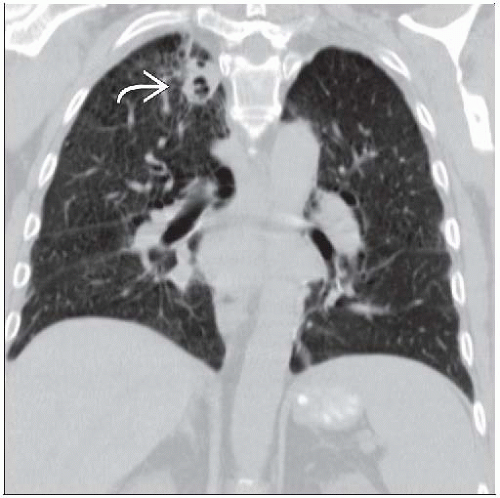
Evolution
Active disease correlated with nodules, masses, or parenchymal disease
Post-therapy
Parenchymal findings should start to clear within 1 week
If no improvement, suspect superinfection
Complete normalization averages 1 month (2-6 weeks)
35% total clearance
50% partial clearance
Larger masses and cavitated nodules more likely to resolve
Relapse
Frequently in areas of previous disease
Involves airways more often
Appearance of pulmonary relapse different in 25%
Radiographic Findings
Asymptomatic radiographic lung involvement (10-30%)
Echocardiographic Findings
Echocardiographic abnormalities related to WG (35%)
Pericardial effusion (20%)
Imaging Recommendations
Best imaging tool: CT more sensitive, particularly for evaluating possible airway involvement
Protocol advice
Usually performed without contrast because of renal insufficiency
Including glottis is helpful because of frequent subglottic involvement
Multiplanar reconstructions are particularly useful for evaluating airways
DIFFERENTIAL DIAGNOSIS
Pneumonia: Bacterial, Fungal
Radiographic findings can be identical
Differentiate by culture or special stains
Lung Cancer, Non-Small Cell
Squamous cell carcinoma most likely to cavitate
Usually solitary
Metastases
Sharply marginated and variably sized
Squamous cell carcinoma or sarcoma histology more common
Septic Emboli
Nodules evolve rapidly and cavitate, blood culture positive
Source: Indwelling catheters, IV drug abuse
Rheumatoid Necrobiotic Nodules
History of joint disease
Usually small and subpleural
Spontaneous pneumothorax common (uncommon in WG)
Lymphomatoid Granulomatosis
Triad: Lung, skin, and nerve (central or peripheral)
Multiple cavitary lung nodules identical to WG
Pulmonary-Renal Syndromes
Microscopic polyangiitis
No necrotizing granulomatous inflammation
Antineutrophil cytoplasmic antibody vasculitis
Churg-Strauss syndrome
Peripheral blood eosinophilia > 10% & asthma
Antineutrophil cytoplasmic antibody vasculitis
Goodpasture syndrome
Antiglomerular basement membrane antibodies
Pulmonary hemorrhage & glomerulonephritis
Polyarteritis nodosa
Renal infarcts, renal arterial disease, lung involvement much less common than WG
Systemic lupus erythematosus
Autoimmune disorder characterized by antinuclear antibodies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree