Case presentation
A 12-year-old male with a history of autism presents with cough for the past 3 weeks. There was initially fever to 102 degrees Fahrenheit, but this lasted for 2–3 days, then resolved. He was seen by his primary care provider 2 weeks ago and was diagnosed with a viral upper respiratory infection. He has not had congestion, vomiting, diarrhea, or abdominal pain. There is no report of choking or concern for foreign body ingestion. He has been eating and drinking well. Examination reveals a temperature of 99 degrees Fahrenheit, a heart rate of 90 beats per minute, a respiratory rate of 20 breaths per minute, a blood pressure of 110/75 mm Hg, and an oxygen saturation of 93% on room air. He appears comfortable and in no respiratory distress. He has no stigmata of allergies. His pulmonary examination reveals scattered rhonchi without crackles; there is slight bibasilar wheezing. He has no rash.
Imaging considerations
Imaging is often employed in the evaluation of children with respiratory complaints. The differential diagnosis can be broad, and the imaging modality that a clinician may employ is dependent on history and physical examination.
Plain radiography
Pediatric patients with suspected viral etiology or uncomplicated bacterial pneumonia do not generally require imaging. Plain radiography is an excellent first-line imaging choice in patients who are not following an expected clinical course, if there are concerns for complications from a previously diagnosed pulmonary infection, the child is severely ill, or if there is an alternative diagnosis under consideration, such as foreign body ingestion. Two views of the chest are needed to allow for proper and complete visualization of chest anatomy, including areas obscured by the heart and mediastinal structures. Plain radiography does have limitations, including variability with image interpretation and image technique, which may make it difficult to obtain meaningful studies in select patients.
Viral infection is the most common cause of pneumonia in the pediatric population. While controversial, radiography is often used to confirm a suspected bacterial etiology and has been shown to correlate well with that diagnosis in children who have Pneumococcus species as a cause of their pneumonia; children with a normal radiograph who have been diagnosed with clinical bacterial pneumonia are not prone to have pneumococcal infection. In one study, the majority of children hospitalized with severe community-acquired pneumonia had radiographs demonstrating alveolar infiltrates, and those with upper lobe infiltrates along with effusions were found to have more serious disease. (For a complete discussion of bacterial pneumonia and radiography, please see Chapter 37 : Community-Acquired Pneumonia).
Ultrasound
Interest in sonography to aid in the diagnosis of pneumonia has increased. Ultrasound has the advantage of a lack of ionizing radiation and is fairly inexpensive compared to other imaging modalities. Ultrasound has proven adept at locating effusions and is more sensitive than computed tomography. , Consolidation can be detected, seen as a hypoechogenic area with poor border definition, but distinguishing between atelectasis and true pneumonia can be difficult, affecting accurracy. , Other studies have shown ultrasound to be effective at diagnosing community-acquired pneumonia in selected patients and may result in shorter length of stay and lower costs compared to chest radiography. Standardized usage for transthoracic ultrasound to aid diagnosing pediatric pneumonia is a developing practice. Studies thus far have shown this modality may be useful, either as a first-line test or as an adjunct to better define abnormal plain radiography findings, although this modality requires specific training to perform appropriately and the noted accuracy may not be generalizable to providers without skill in thoracic ultrasound.
Computed tomography
Computed tomography is generally not a first-line imaging modality. Use of this technology may be indicated in children with complex illness or when a diagnosis is uncertain.
Imaging findings
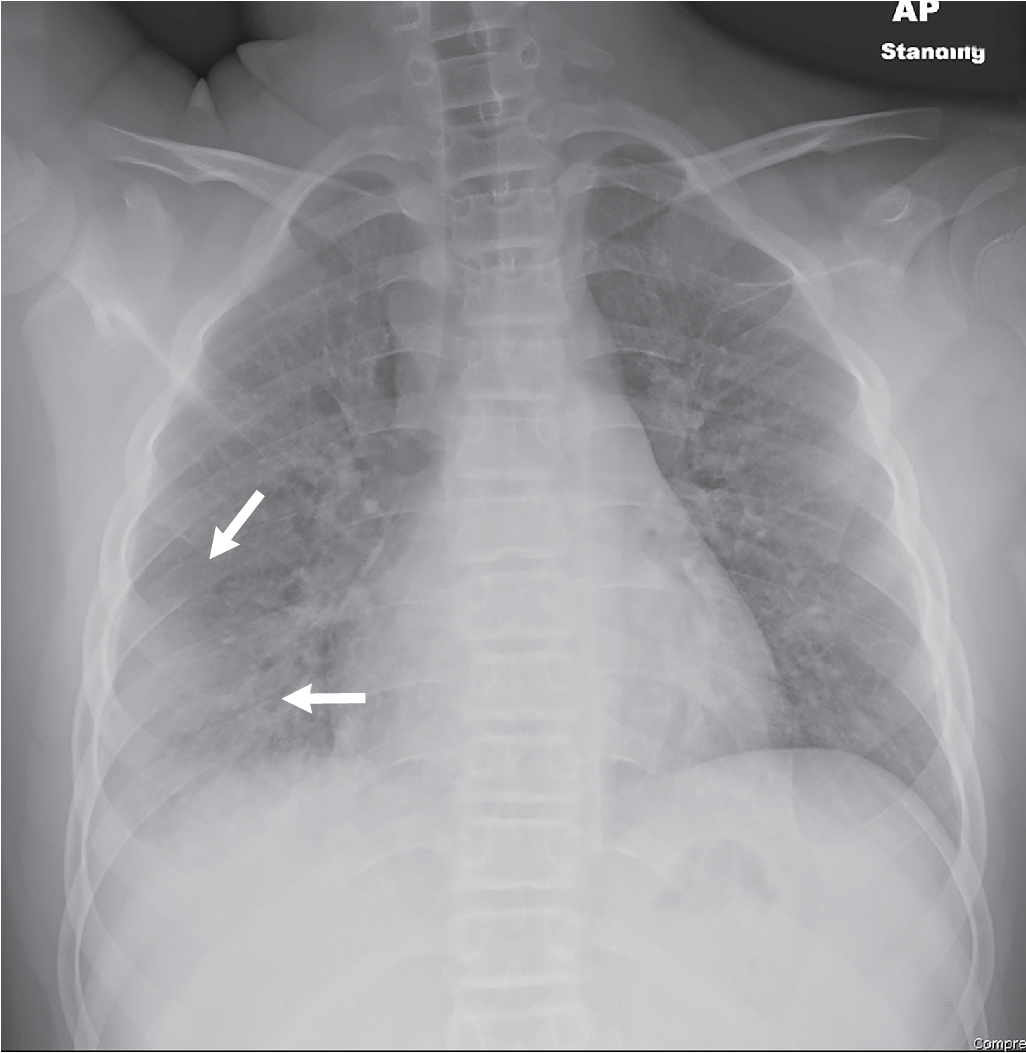
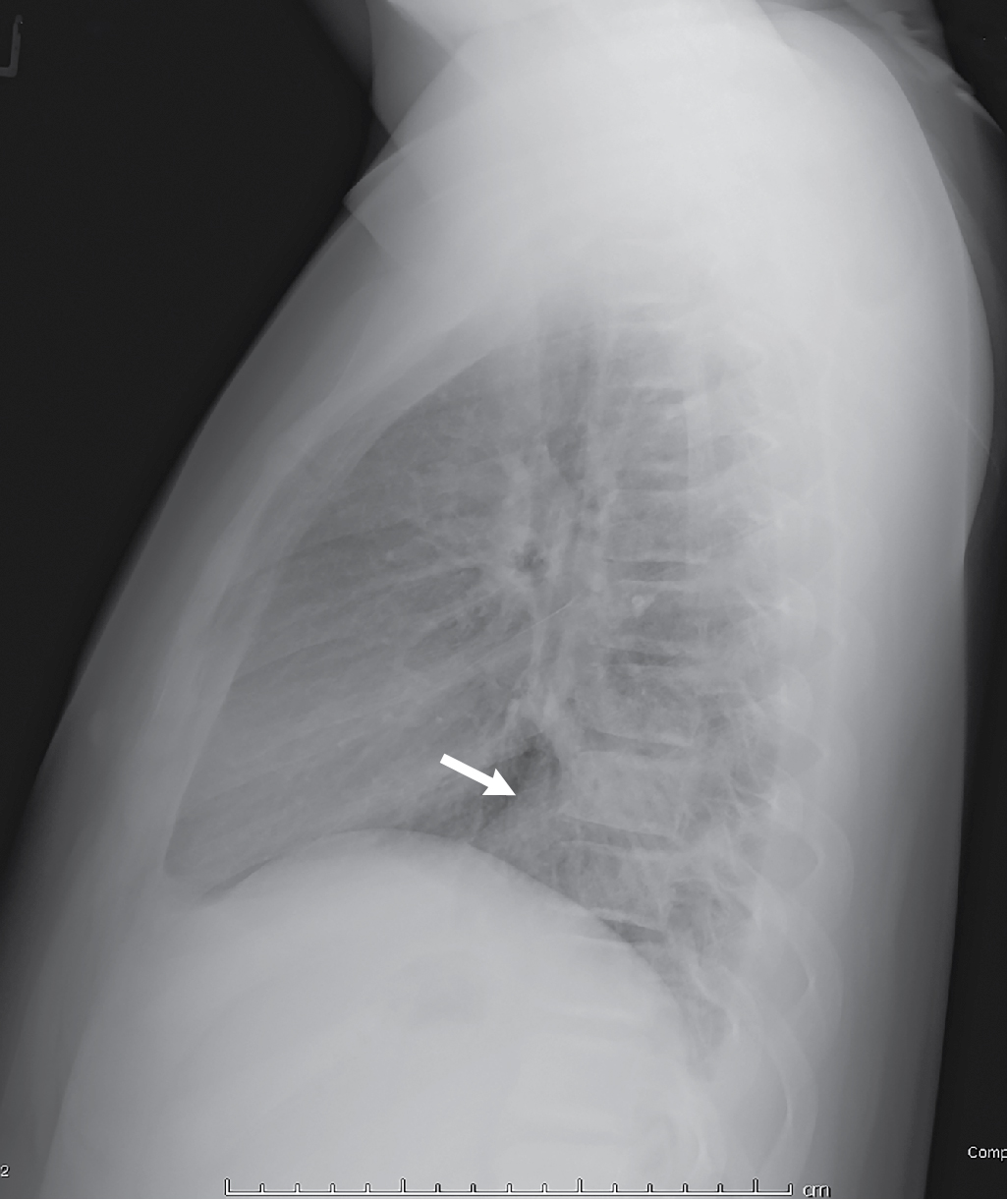
The patient had two-view radiography of the chest. The images demonstrate interstitial opacities in the lungs, with a hazy more focal parenchymal opacity in the right lower lung, best seen on the AP view. There are no signs of pleural effusion/fluid. The cardiac silhouette is normal with a left-sided aorta ( Figs. 39.1 and 39.2 ).