Case presentation
A 4-year-old male presents to the emergency department after his parents witnessed the ingestion of a coin. His mother states that he grabbed one out of her purse that was lying on the ground nearby. The patient is resting comfortably in the room, in no acute distress. His lungs are clear to auscultation, there is no stridor, and he is managing his secretions. His vitals are all within normal limits.
Imaging considerations
Plain radiography
Anteroposterior and lateral x-rays of the neck, chest, and abdomen should be the initial diagnostic choice when there is concern for foreign body ingestion. , This recommendation is regardless of whether the object is thought to be radiolucent or if symptoms indicate a particular location of the foreign body. Radiography will help determine the size, location, and shape of radiopaque foreign bodies and the management plan. Although radiolucent objects may not be seen on plain radiographs, there are secondary signs such as relative radiolucency, air fluid levels, free air, air trapping in lung, bowel obstruction, or soft tissue swelling that can be appreciated.
Computed tomography (CT)
A CT scan should be considered for further evaluation of foreign body ingestion when no foreign body is found on radiographs and the child is exhibiting symptoms such as difficulty breathing, wheezing, or inability to tolerate secretions, or if the likely ingestion has high-risk characteristics (such as a large object [≥25 mm in diameter or >5 cm in length]), concern for radiolucent foreign object ingestion, or a history of esophageal strictures. Although a small radiolucent foreign body could still potentially be missed, CT has been shown to be highly effective at identifying ingested foreign bodies. CT has also been found to be useful in identifying perforation, abscess formation, inflammation, peritonitis, and other complications from foreign body impaction. ,
Upper gastrointestinal series (UGI)
UGI is another useful option for foreign body ingestion, including radiolucent objects that might not appear on plain radiographs. The use of barium is not recommended due to the potential for obscuration if endoscopy is performed afterward. A water-soluble contrast should be used instead.
Point-of-care ultrasound (US)
There have been multiple cases of point-of-care US being used in the identification of foreign body ingestions in children. , The use of this modality is operator dependent, but US can be especially useful in the identification and localization of radiolucent foreign bodies. It not only provides a nonionizing radiation option but also can be done at the bedside. Foreign bodies are usually visualized as hyperechoic structures with posterior shadowing.
Magnetic resonance imaging (MRI)
MRI can also be used to evaluate for the ingestion of radiolucent foreign bodies and subsequent complications. As with CT, this additional imaging is not warranted if the patient is asymptomatic and the object is not known to have any high-risk characteristics. MRI is contraindicated in the case of any metallic foreign body.
Imaging findings
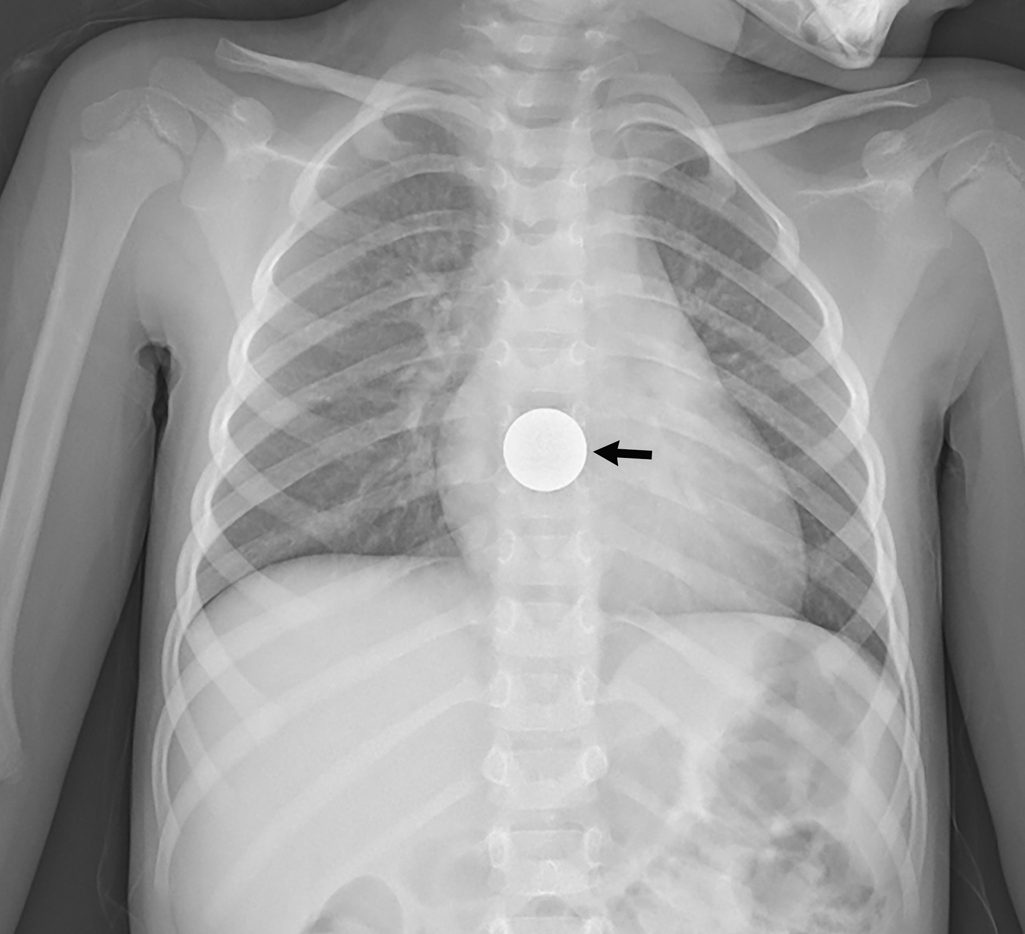
Plain radiography was obtained and demonstrated a metallic, flat, disk-shaped foreign body in the distal thoracic esophagus, likely a coin ( Figs. 19.1 and 19.2 ).

Case conclusion
The patient was admitted for observation and serial x-rays. The coin spontaneously passed into the stomach without complication and the patient was discharged home with outpatient follow-up.
Children are notorious for placing objects in their mouths. While many of these objects pass without any symptoms or perhaps awareness of the parents, they can, on occasion, become impacted in the gastrointestinal (GI) tract and cause serious complications. Children may present completely asymptomatic with a parent or witness claiming they saw a possible ingestion. When evaluating these patients in the emergency department, it is vital to determine if an ingestion occurred, what was ingested, and where the object is located and assess the potential risk to the child.
An impaction in the esophagus generally requires the most urgent management. Anatomic sites of narrowing in the esophagus that are most common for impaction include the level of the aortic arch as well as the upper (level of thoracic inlet) and lower esophageal sphincters. Patients with an esophageal foreign body can present with vomiting, pooling of secretions, refusal to eat, dysphagia, chest pain, or respiratory symptoms such as stridor or wheezing or they can be asymptomatic. Management is based on the object ingested and the degree of symptoms. Button batteries, sharp objects, multiple magnets, and large objects causing complete obstruction will require emergent removal by endoscopy. In contrast, small, round, or inert objects not causing significant symptoms can be observed for up to 24 hours from time of ingestion to see if they spontaneously pass into the stomach.
The vast majority of foreign bodies that pass spontaneously into the stomach will continue their journey through the GI tract without complication. These can generally be managed conservatively with serial radiographs as an outpatient until the object has passed. Certain objects may still need removal depending on their size and shape.
Coins
Coins are the most common foreign body ingested by pediatric patients. Due to their radiopaque nature, they are usually found on plain radiography. Anteroposterior (AP) and lateral radiographic views of the neck, chest, and abdomen, to include from the nasopharynx to the anus, should be obtained. Management will be based on the location and size of the coin.
In cases where the location of trachea versus esophagus is in question, using two views to localize the foreign body with respect to the tracheal air column is most useful. Traditional teaching has held that coins in the trachea tend to orient themselves in a sagittal plain while coins in the esophagus tend to orient themselves in the coronal plane. This was described as due to vocal cord sagittal orientation and the C-shaped cartilaginous rings of trachea that would cause coins to align sagittally, along the larger anteroposterior diameter, if in the trachea. However, this is not supported in the literature: Coins are most likely to be lodged in the esophagus, and although coins most commonly align in a coronal plane in the esophagus, a coin in the esophagus may be sagittally oriented, especially in older children. ,

Button batteries
Button batteries pose a unique risk when ingested due to their ability to cause severe caustic injury to the esophagus within a few hours of ingestion. The number of such battery ingestions has increased as they have become more available.
The type of battery can be identified from the battery code on the packaging if available. The first two numbers in a four-digit code give the diameter in millimeters. The last two numbers in the four-digit code give the height in tenth of a millimeter. For help in identification and management of battery ingestion, call the National Battery Ingestion hotline at 800-498-8666.
Prehospital management ,
Assume lithium battery ingestion unless otherwise known
Administer honey (10 mL every 10 minutes, up to six doses) IF:
- ■
Child >12 months of age
- ■
Child can swallow
- ■
Honey immediately available
- ■
Hearing aid battery not ingested
It is very important to distinguish between a button battery that requires emergent removal and a benign coin that may pass spontaneously. Two distinguishing characteristics of a button battery on radiography that can help differentiate a battery from a coin are the halo sign and step-off edge. When a button battery is visualized “en face” on a radiograph (usually on the AP view in the esophagus), there will be a lucent second ring seen along the outer edge giving the appearance of a halo ( Figs. 19.3 A and 19.4 A,B). A coin will not have the lucent second ring. When a button battery is viewed in profile (usually on the lateral view in the esophagus), there is a step-off between the anode and cathode side of the battery ( Figs. 19.3 B and 19.5 A,B), as opposed to the symmetrical edge of a coin (see Fig. 19.2 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








