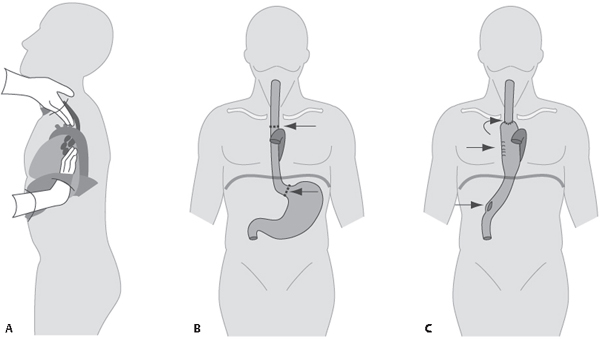
CASE 193 49-year-old man diagnosed with esophageal cancer six months earlier and treated with surgery PA (Fig. 193.1A) and lateral (Fig. 193.1B) chest X-rays demonstrate evidence of a right thoracotomy with associated rib deformity. Surgical clips are seen in the right tracheobronchial angle, perihilar region, and left upper quadrant. There is a partial silhouette of the right interlobar artery, dorsal spine, and cardiophrenic angle by a curvilinear opacity extending from the cardiophrenic angle to the clavicle. Contrast-enhanced axial (Figs. 193.1C, 193.1D, 193.1E) and coronal (Figs. 193.1F, 193.1G, 193.1H) CT (mediastinal window) shows postoperative changes of an Ivor Lewis intrathoracic esophagectomy and esophagogastric anastomosis. The neoesophagus or gastric tube has been placed in the right paravertebral space. Esophageal cancer is the third most common gastrointestinal malignancy and one of the most prevalent cancers in the world. Surgery is the mainstay of treatment for patients with early-stage disease. Locally advanced disease in non-surgical patients is managed with chemotherapy and radiation therapy. Esophageal resection with various forms of reconstruction benefits many patients with esophageal cancer suffering from dysphagia. Esophageal resection can be performed using either a transthoracic or transhiatal technique. • Ivor Lewis procedure. The most commonly performed procedure for treatment of mid- and distal esophageal cancers. An initial laparotomy to mobilize the stomach is followed by a right thoracotomy. The esophagus is excised en bloc and the thoracic duct is ligated. Lymph nodes along the celiac trunk, splenic and common hepatic arteries, and periesophageal, aortopulmonary and subcarina are dissected. A high cervical intrathoracic anastomosis, above the azygos vein, is created between the proximal esophageal remnant and stomach, forming the neoesophagus (Figs. 193.1A, 193.1B, 193.1C, 193.1D, 193.1E, 193.1F, 193.1G, 193.1H, 193.2A, 193.2B). The neoesophagus is most commonly positioned in the posterior mediastinum prevertebral space, but may also be placed in the right paravertebral or anterior mediastinal substernal space. Pyloromyotomy or pyloroplasty is performed to prevent post-vagotomy gastric outlet obstruction from pylorospasm (Fig. 193.2A). • McKeown procedure. This procedure involves a midline laparotomy, anterolateral thoracotomy, and cervicotomy. Stomach mobilization, lymphadenectomy, and esophageal resection are performed in a manner similar to the Ivor Lewis. The primary difference is that the cervical esophagogastric anastomosis is created in the neck as opposed to the thorax, reducing the potential for sepsis from anastomotic dehiscence. • Left thoracoabdominal thoracotomy. This approach is optimal for lower esophageal and gastric cardia cancer because it provides simultaneous exposure of the upper abdomen and posterior mediastinum through a single incision. Extensive lymphadenectomy can be performed and concomitant left lung lesions resected. The lower esophagus is resected and the stomach mobilized. The esophagogastric anastomosis is performed behind the transverse aorta. Fig. 193.1 Fig. 193.2 Artist’s illustration of the Ivor Lewis transthoracic esophagectomy (A). Laparotomy is performed to mobilize the stomach, perform a pyloromyotomy (lower arrow, second figure), and dissect regional lymph nodes. Subsequently, a right thoracotomy is performed to remove the esophagus and dissect those regional nodes (arrows, first figure). The neoesophagus is created by joining the esophageal remnant and stomach high in the thorax (upper arrows, second figure). Contrast-enhanced chest CT (B) of an Ivor Lewis esophagectomy shows the mobilized neoesophagus positioned as is seen most commonly, in the prevertebral posterior mediastinal space. This procedure is performed for resection of distal esophageal or gastric cardiac neoplasms. Two incisions are made. First, a cervicotomy paralleling the sternocleidomastoid muscle provides access to the proximal esophagus. Second, a supraumbilical-to-xiphoid incision provides access to the distal esophagus. Combined but “blinded” circumferential dissection and mobilization of the intrathoracic esophagus and lymphadenectomy are performed as the surgeon places his or her hand through both the cervical and abdominal incisions. The cervical esophagus is divided, and the stomach with the attached esophagus is removed through the supraumbilical incision. The esophagus is resected. A partial proximal gastrectomy and pyloromyotomy are performed and the cervical esophagogastric anastomosis created (Fig. 193.3). Since a formal thoracotomy is avoided, peri-operative respiratory problems are less of an issue and anastomotic leaks are more easily managed. Fig. 193.3 Artist’s illustration of the various stages of trans-hiatal esophagectomy. Initially, a cervical incision is made to access the proximal esophagus and a supraumbilical incision to access the distal esophagus. The surgeon then places the hands through the upper and lower incisions and “blindly” dissects and mobilizes the intrathoracic esophagus (A)
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Discussion
Discussion
Background
Transthoracic Esophagectomy


Trans-Hiatal Esophagectomy without Thoracotomy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree