Fig. 9.1
(a) Anteroposterior and (b) Y-view radiographs in an acutely injured female handball player demonstrate anterior dislocation of the right shoulder
Handball involves overhead throwing and consequently nonacute and overuse injuries with shoulder pain are a common problem among handball players. A high proportion of female elite handball players in Norway were found to have shoulder pain (36 %, 65 of 179) and unstable shoulder (29 %, 51 of 179) on clinical examination (Myklebust et al. 2013).
MRI diagnosis of a rotator cuff tear in handball players can be difficult because lesions are often small and may appear in atypical locations. Subtle articular surface tears are usually seen in young patients (Ouellette et al. 2005). Thus, MR arthrography including imaging in ABER position (i.e., abduction and external rotation) has been recommended for the evaluation of young overhead-throwing athletes (Tuite 2003). A study correlating MR arthrography and arthroscopic findings (Waldt et al. 2007) demonstrated that MR arthrography is highly accurate in the diagnosis of full-thickness rotator cuff tears and is accurate in the diagnosis of articular-sided partial-thickness tears. Limitations in the diagnosis of partial-thickness tears are mainly restricted to small articular-sided tears (Ellman grade 1) due to difficulties in distinguishing among fiber tearing, tendinitis, synovitic changes, and superficial fraying at tendon margins. For patients who are claustrophobic or have severe pain and cannot tolerate conventional MR arthrography sequences, fast MR arthrography of the shoulder joint using volumetric interpolated breath-hold examination (VIBE) sequences can be used as a substitute for standard T1-weighted fat-saturated sequences. These sequences are useful for the investigating the appearance of the rotator cuff, in particular for large articular-sided partial-thickness tears and for full-thickness tears (Vandevenne et al. 2009). In combination with clinical history and examination, MRI can help to diagnose the underlying structural changes and to assist the clinician in instituting appropriate treatment for individual athletes (Arce et al. 2013; Cowderoy et al. 2009).
9.3.1.1 Injuries of the Rotator Cuff
Broadly speaking, there are three types of rotator cuff injuries in overhead-throwing athletes such as handball players: internal impingement (posterosuperior glenohumeral impingement), external impingement, and overuse syndrome (tensile overload) (Ouellette et al. 2005; Economopoulos and Brockmeier 2012).
Internal Impingement
In the late cocking phase of the overhead-throwing cycle, during extreme ABER, there may be repetitive impaction of the posterior greater tuberosity on the supraspinatus–infraspinatus junction and posterosuperior glenoid (Fig. 9.2). This common condition in handball players is called internal or posterosuperior glenohumeral impingement, which may lead to rotator cuff tears and posterosuperior labral tears (Jobe 1997) (Fig. 9.3). Internal impingement can be either primary (i.e., without evidence of glenohumeral instability) or, more commonly, secondary (due to increased anterior shoulder laxity and instability) (Ouellette et al. 2005). On MRI, posterior supraspinatus or supraspinatus–infraspinatus junction (posterior interval) tears are seen at up to 1 cm from the greater tuberosity insertion. The tendon tears are usually small and seen at the articular surface of the rotator cuff. Thus, internal impingement rotator cuff tears are better evaluated using MR or CT arthrography where they appear as a small undersurface linear contrast extension in the tendon. ABER positioning is important in these patients since relaxation of the posterior superior rotator cuff may allow contrast to seep into a subtle tear (Tirman et al. 1994). Moreover, these patients often have associated posterosuperior labral lesions (Fig. 9.3). Cysts and impaction deformities are also commonly found at the posterior greater tuberosity in handball players with internal impingement (Ouellette et al. 2005).
Fig. 9.2
Schematic illustration of internal impingement, superior view (posterosuperior glenohumeral impingement). Repetitive impaction of the posterior greater tuberosity on the supraspinatus–infraspinatus junction and posterosuperior glenoid is common in handball players
Fig. 9.3
A 27-year-old male handball player with chronic posterosuperior glenohumeral impingement. Coronal fat-suppressed proton density-weighted MRI of the right shoulder shows bone marrow edema and cystic changes of the greater tuberosity (a, b, arrow) and tendinopathy of the articular surface of the supraspinatus tendon without a tear (b, arrowhead). Axial fat-suppressed proton density-weighted MRI of the right shoulder (c) demonstrates linear increased signal intensity under the avulsed labrum (arrow). Axial CT arthrography image (d) shows a hyaline cartilage defect with adjacent partial tearing of the labrum (GLAD lesion, arrow). Axial CT arthrography image in ABER position (e) demonstrates posterosuperior labrum fraying (arrowhead) and a large articular surface partial-thickness tear of the posterior supraspinatus tendon (arrow) which is not seen on MRI. (The ABER position allows visualization of the delamination of deeper layers of the tendon.) Contact between the rotator cuff and posterosuperior glenoid can be a normal finding. However, association with cystic changes of the greater tuberosity (b) and a “kissing” tear of the rotator cuff with a labral lesion in ABER position (e, f) is highly suggestive of internal impingement
External Impingement
External impingement can be either primary or secondary (Ouellette et al. 2005). In primary external impingement, shoulder pain occurs following contact between the coracoacromial arch and the rotator cuff. The origin of the pain is the rotator cuff itself and irritation of the interposed subacromial bursa. The large inferior torque in the deceleration phase of the throwing cycle may result in subacromial impingement (Meister 2000) (Fig. 9.4). Posttraumatic deformity, downsloping acromion, acromioclavicular degenerative change, and congenital thickening of the coracoacromial arch and os acromiale may also increase the risk of impingement (Tuite 2003). On MRI, rotator cuff tendinosis and tears associated with primary external impingement are more commonly found in older handball players and usually involve the anterior half of the supraspinatus tendon up to 1 cm from its insertion (Tuite et al. 1998). Diagnosis of tendinosis is made when there is thickening of a rotator cuff tendon with increased intermediate signal. Tears are diagnosed when fluid signal intensity or gadolinium extends into a rotator cuff tendon (Ouellette et al. 2005).
Fig. 9.4
A 29-year-old male handball player with external impingement of the shoulder. Coronal fat-suppressed proton density-weighted MRI of the left shoulder (a) demonstrates subacromial–subdeltoid bursitis (arrow) and bursal surface tendinopathy of the supraspinatus (arrowhead). This association can be a normal finding in high-level players, and physician needs to correlate with clinical findings. There is also coracohumeral ligament hypertrophy (b, arrow). Sagittal fat-suppressed proton density-weighted MRI (c) shows the bursitis (arrow) and superficial tendinopathy of the supraspinatus (arrowhead)
Coracohumeral impingement syndrome is also an important cause of pain in handball players. A decreased distance between the lateral aspect of the coracoid and the lesser tuberosity of the humerus results in impingement of the anterior rotator cuff, causing pain (Kassarjian et al. 2004). A coracohumeral distance of less than 6 mm on MRI is suggestive of impingement (Ouellette et al. 2005). Patients with coracohumeral impingement syndrome usually do not have rotator cuff tears (Paulson et al. 2001), but the presence of coracohumeral impingement increases the likelihood of a subscapularis tear (Kassarjian et al. 2004).
Secondary external impingement results from glenohumeral joint instability. It is one of the most common causes of shoulder pain in handball players. Although glenohumeral instability is the underlying etiology, secondary external impingement is uncommonly secondary to glenohumeral joint dislocation. Rather, it is usually secondary to accentuated microinstability, which is in itself typically asymptomatic (Tuite 2003).
During the late cocking and early acceleration phases of throwing, there is significant shear force across the shoulder. Over time, the anterior capsule fails, giving rise to anterior glenohumeral joint laxity and increased anterior translation during throwing (Dillman et al. 1993). Handball players with superior labrum anterior to posterior (SLAP) tears or injury to the long head of the biceps are also susceptible to secondary impingement. On MRI, supraspinatus and infraspinatus abnormalities can be seen at any location (Tuite 2003). The imaging appearance of rotator cuff tendinosis and tears seen in secondary external impingement is similar to that of primary impingement.
Overuse Syndrome
Rotator cuff overuse syndrome (tensile overload) results from repetitive traction. Although axial tendon strength is greater than that of bone, a large amount of stress at the rotator cuff during the deceleration phase of the overhead-throwing cycle is eccentric and is thought to cause tensile overload tears in normal tendons (Blevins 1997). Repetitive stress encountered in handball players also accelerates the degenerative process of the rotator cuff, resulting in early tendinosis (Tuite 2003). Tendinosis weakens tendons and increases the risk of a superimposed rotator cuff tear. On MRI, rim-rent tears (which are articular surface partial tears at the humeral tendinous insertion) can be seen from tensile overload on a normal tendon. Rim-rent tears have high signal extending between the greater tuberosity tendon insertion and the tendon. High signal violates the very distal articular surface of the affected tendon. Other tensile overload tears may be seen at the articular surface of the supraspinatus and infraspinatus tendon. These tears are commonly small and best appreciated on MR arthrography in the ABER position as fluid intensity or as gadolinium transgressing the low-intensity line on the articular surface of rotator cuff tendons (Tuite 2003).
9.3.1.2 Injuries of the Proximal Biceps Brachii
Proximal biceps tears may occur in a stable shoulder in the late cocking phase and deceleration phase of the throwing cycle. During the late cocking phase, there is biceps contraction to limit torsion forces in ABER. In the deceleration phase, the biceps strongly contract to resist glenohumeral joint distraction. Maximum elbow flexion torque occurs before maximal shoulder compressive forces, in ideal throwing mechanics. If maximal forces at the elbow and shoulder are applied at the same time, there is increased biceps strain and therefore increased risk of biceps injury. Tendinosis or tears of the long head of the biceps may also occur secondary to external impingement under the coracoacromial arch, as described earlier (Ouellette et al. 2005).
On MRI, tendinopathy of the long head of biceps tendon is represented by abnormal signal intensity and caliber changes. The biceps tendon may appear thickened or flattened within the rotator interval or bicipital groove. One should note, however, signal changes within the obliquely oriented intra-articular biceps tendon are less specific, due to partial volume averaging and the magic angle effect, and they need to be correlated with changes in the caliber of the tendon in all three imaging planes. An excess of fluid and synovitis around the biceps tendon in the bicipital groove, in the absence of a large glenohumeral joint effusion, is indicative of tenosynovitis, which may lead to an altered gliding motion of the biceps tendon within the groove and consequent tendon degeneration and wear. Focal fluid within the biceps tendon or abrupt caliber changes indicates partial tears which may result in eventual rupture (Eakin et al. 1999). Complete tears of the biceps tendon are characterized by the absence of the biceps tendon in the bicipital groove proximally on axial imaging, with a thickened and retracted tendon end often visualized distally. Disruption of the intra-articular biceps or biceps anchor can usually be appreciated on coronal oblique and sagittal images, with redundancy of the torn proximal tendon end increasing diagnostic certainty (Stevens et al. 2012).
9.3.1.3 Injuries of the Glenoid Labrum
Labral injuries may be due to normal overuse of the shoulder or instability of the shoulder which may be primary or secondary to acute trauma. The glenoid labrum infrequently tears without underlying shoulder instability. The humeral head mildly translates back and forth during late cocking and deceleration phases of throwing under compressive forces to grind the labrum. This microinstability and “grinding factor” can cause injuries of the anterosuperior labrum (Meister 2000). Table 9.1 summarizes the known types of SLAP lesions (Mohana-Borges et al. 2003; Stevens et al. 2012). Overuse syndrome of the superior glenoid labrum, i.e., SLAP type 2 lesions, are also commonly secondary to traction forces from the long head of the biceps which occur in the deceleration phase of the throwing cycle (Meister 2000). Of the ten known types, types 2, 4, 5, 6, 7, 8, and 10 involve the biceps tendon (Figs. 9.5 and 9.6), while types 1, 3, and 8 do not (Fig. 9.7). The appearance of SLAP tears on MRI includes intermediate hyperintense labral degeneration and linear fluid or gadolinium undercutting the superior labrum, extending posterior to the biceps origin (Beltran et al. 2003).
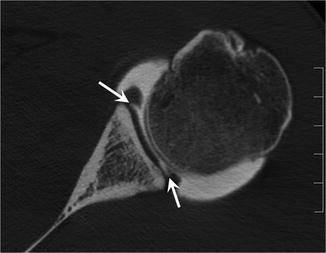

Table 9.1
Types of SLAP tears and their findings and causative mechanisms
Type | Findings | Mechanism |
|---|---|---|
1 | Superior labral fraying with intact biceps | Repetitive overhead throwing |
2 | Superior labral tear with stripping of the biceps 2A: with anterior extension of labral tear 2B: with posterior extension of labral tear 2C: with anterior and posterior extension of labral tear | Repetitive overhead throwing |
3 | Bucket-handle tear of the superior labrum with intact biceps | Fall on outstretched hand |
4 | Bucket-handle tear of the superior labrum and extension of the tear into the biceps tendon | Fall on outstretched hand |
5 | Bankart lesion extending to the superior labrum, biceps tendon stripping | Anterior shoulder dislocation |
6 | SLAP type 2 with anterior or posterior flap tear | Fall on outstretched hand |
7 | Superior labral tear, biceps stripping, and middle glenohumeral ligament tear | Anterior shoulder dislocation |
8 | Similar to type 2B but with more extensive abnormalities | Acute trauma with posterior shoulder dislocation |
9 | SLAP type 2 with circumferential labral detachment | Trauma |
10 | Superior labral tear with extension to the structures that cross the rotator interval | Trauma |
Fig. 9.5
A 29-year-old male handball player with pain during arm elevation and clinical microinstability. Coronal reformatted CT arthrography image (a) shows a bucket handle tear of the superior labrum (black arrow, SLAP 4) and extension to the biceps tendon (white arrow). Sagittal reformatted CT arthrography image (b) confirms the long biceps tendon tear (arrow). Another coronal reformatted CT arthrography image (c) shows superior labrum avulsion
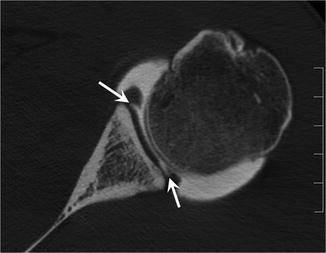
Fig. 9.6
A 28-year-old male handball player with multidirectional shoulder instability. SLAP type 9 lesion. Axial CT arthrography image shows both posterior and anterior labrum avulsions (arrows)

Fig. 9.7
A 27-year-old male handball player with pain during throwing motion. SLAP type 3 lesion. Coronal reformatted CT arthrography image demonstrates a bucket handle tear of the superior labrum (arrow)
Bennett Lesion
A Bennett lesion is a bony spur at the posterior inferior aspect of the glenoid (Ferrari et al. 1994). This lesion is most commonly seen in baseball pitchers, probably caused by traction of the posterior band of the inferior glenohumeral ligament that occurs during the deceleration and follow-through phases of throwing. Further growth of the lesion is likely due to posterior humeral impingement in the late cocking phase of overhead throwing. Bennett lesions are frequently associated with tears of the posterior labrum, teres minor, and infraspinatus tendons in symptomatic shoulders (Ferrari et al. 1994). Bennett lesions are usually asymptomatic, but large lesions may cause posterior shoulder pain (Nakagawa et al. 2006).
Glenohumeral Joint Instability
In the late cocking and early acceleration phases of overhead throwing, there is significant shear force across the shoulder. Over time, there is an increased load at the anterior capsule, often secondary to poor technique and fatigue of the external stabilizing musculature of the shoulder. The anterior capsule eventually fails with stress and accumulation of repetitive microtrauma, leading to anterior glenohumeral joint laxity (Dillman et al. 1993). Laxity of the anterior shoulder joint allows increased anterior translation of the humeral head during throwing, which in turn increases the risk of anterior labral lesions and SLAP tears.
Some players have generalized ligamentous laxity bilaterally, which may be accompanied by a hypoplastic labrum. These players also exhibit hyperextension of other joints such as elbows and knees and are capable of the highest-velocity throws and ball movements. They do, however, have a high level of risk for microtrauma and long-term injury secondary to throwing (Meister 2000).
Acute traumatic instability is uncommon in handball players. An acute traumatic event typically leads to a unidirectional pattern of instability of the glenohumeral joint (Matsen 2002) (Fig. 9.8).
Fig. 9.8
A 33-year-old male handball player with glenohumeral instability following trauma. Axial (a) and sagittal (b) fat-suppressed proton density-weighted MRIs show anteroinferior glenoid fracture and labral avulsion (arrow) in keeping with an osseous and fibrous Bankart lesion
9.3.2 Elbow
Overhead throwing in handball generates large valgus and extension forces at the elbow in the late cocking and early acceleration phases of the throwing cycle. This leads to high tensile stress at the medial compartment, significant compressive forces at the lateral compartment, and high shear forces at the posteromedial olecranon. Medial compartment tensile loads in handball players lead to injuries of the medial stabilizing structures including medial joint laxity, ulnar collateral ligament tears, ulnar neuritis, flexor–pronator muscle origin injury, and medial epicondyle apophysitis or avulsion. Lateral compressive forces can lead to osteochondral injuries of the capitellum, which may result in loose bodies. Shear stress results in injuries of the posteromedial tip of the olecranon and trochlea/olecranon fossa, which may cause osteophytosis, loose bodies, and fractures (Ouellette et al. 2005). Radiography and MRI have important diagnostic roles, particularly when the clinical presentation is unclear and to evaluate for other important potential associated injuries such as myotendinous injuries, fractures, dislocations, and osteochondral lesions (Beltran et al. 2013).
9.3.2.1 Technical Consideration Regarding MRI of the Elbow Joint
Using a Whole-Body MR Scanner
The patient is positioned either in the “superman” position or in the supine position. For the superman position, the patient lies prone with the arms raised over the head and the elbows in full extension. The forearm is placed in supination (i.e., thumb up). The superman position has two distinct advantages, i.e., improved signal-to-noise ratio from more central positioning in the bore and a wider selection of usable coils. In general, the best available knee coil (e.g., eight or more receiver channels) provides the best technical performance in elbow MRI when scanning in the superman position (Wenzke 2013). Unfortunately, many patients cannot tolerate the position long enough to complete the study, particularly those with shoulder pain or injury. Patient comfort is critical to reducing motion artifacts. Pillows under the axilla can reduce strain on the shoulder. The arm and hand should be padded for comfort and immobilization (Wenzke 2013).
Patients can tolerate supine positioning much more easily. The arm is adducted with the elbow in full extension. The thumb is pointed up (i.e., neutral or mild supination at the elbow). The elbow should be as far from the edge of the bore as possible. Disadvantages of the supine positioning are reduced signal-to-noise ratio, compromise of frequency-selective fat suppression techniques when the elbow is near the edge of the bore, and limitations on coil selection (Wenzke 2013).
A third specialized position, the flexion, abduction, and supination (FABS) position, enhances visualization of the distal biceps tendon and is used when injury to that structure is the primary clinical concern (Giuffre and Moss 2004). The patient lies prone in the scanner with the arm over the head. The elbow is flexed 90° and the thumb is pointed up. Some patients find this position uncomfortable. Although the elbow is near the isocenter of the magnet, flexion at the joint limits coil selection (Wenzke 2013).
Using an Extremity MRI Scanner
Extremity MRI systems cost significantly less than whole-body systems, and the open design is more comfortable for patients. Older systems with low-field strength magnets suffered from poor signal-to-noise ratio, long scan times, poor spatial resolution, and an inability to obtain thin slices. Frequency-selective fat saturation could not be performed at low-field strength, and STIR had to be used as a substitute (Wenzke 2013). The latest generation of extremity MR imaging systems, however, includes superconducting magnets with field strengths to 1.5 T and the ability to use traditional fat suppression techniques. Extremity MRI systems are designed so that the patient’s elbow (or any other joints in the upper and lower extremities) is always centrally positioned in the magnetic field. Disadvantages compared to traditional whole-body scanners include a reduced longitudinal field of view and longer scan times. Although these dedicated extremity systems may not outperform the best whole-body systems in terms of image quality, the major technical improvements combined with the lower price point and patient comfort make these scanners viable options for some practices and institutions (Wenzke 2013).
9.3.2.2 Ulnar Collateral Ligament Injuries
The ulnar collateral ligament comprises three bands: the anterior, posterior, and transverse. The anterior band is the largest and is the major valgus stabilizing structure at the degree of flexion seen in throwing athletes (Hotchkiss and Weiland 1987; Morrey et al. 1991; Regan et al. 1991). The anterior band of the ulnar collateral ligament originates from the inferior aspect of the medial epicondyle and inserts on the sublime tubercle at the medial aspect of the coronoid process of the ulna. Repetitive tension on the medial ligaments during the acceleration phase of the throwing cycle may lead to ligamentous weakening, inflammation, and progressive laxity (Popovic and Lemaire 2002). Following repetitive stress, the anterior band of the ulnar collateral ligament may eventually tear, usually at its ulnar insertion at the sublime tubercle of the coronoid process. Less commonly, a small avulsion fracture of the sublime tubercle may occur (Glajchen et al. 1998).
Imaging diagnosis of ulnar collateral anterior band injuries is important because this structure is not well assessed arthroscopically (Field et al. 1995). There are indirect signs on radiography that may indicate ligamentous injury, i.e., heterotopic ossification of the ulnar collateral ligament and a variation of more than 0.5 mm at the medial joint on stress views, compared with nonstress images (Mulligan et al. 2000; Rijke et al. 1994). Contrast extending beyond the medial capsule on CT arthrography is sensitive and specific for partial and complete ligamentous tears (Timmerman et al. 1994). On MRI, the anterior band of the ulnar collateral ligament appears as a line of low signal intensity extending from the inferior medial epicondyle to the sublime tubercle of the coronoid. MRI features of acute injury include discontinuity of some or all fibers of the ligament and intraligamentous T2 hyperintensity. The ligament may be retracted if completely torn. MRI features of chronic injury include diffuse ligamentous T2 hyperintensity and thickening. MRI arthrography is the study of choice for ulnar collateral ligament injury (Wenzke 2013). It has been demonstrated that MR arthrographic sensitivity for partial tears is 86 % with a specificity of 100 % (Schwartz et al. 1995). In addition to the features of ligamentous tear seen on conventional MRI, extracapsular leakage of contrast indicates complete medial collateral ligamentous disruption or avulsion on MR arthrography (Cohen and Bruno 2001). Partial-thickness undersurface tears of the distal anterior band of the ulnar collateral ligament near the sublime tubercle insertion have been described as having the appearance of a “T,” hence the T sign (Schwartz et al. 1995) (Figs. 9.9 and 9.10).
Fig. 9.9
A 19-year-old male handball player with acute-onset pain on a blocked attack and ulnar collateral ligament strain. Coronal fat-suppressed proton density-weighted MRIs of the right elbow show increased signal intensity of the ulnar collateral ligament (a, arrow) and tension loss (b)
Fig. 9.10
A 20-year-old female handball player with ulnar collateral strain. Coronal reformatted CT arthrography image of the right elbow (a) shows a distal tear of the ulnar collateral ligament with the typical T sign (red arrow). Coronal fat-suppressed proton density-weighted MRI (b, c) confirms the distal ulnar collateral ligament tear. Normal appearance of the common flexor tendon
9.3.2.3 Medial Epicondyle Lesions
Medial Epicondylitis
The medial epicondyle serves as a common origin for the wrist flexor and pronator muscles. These muscles provide important dynamic support during valgus stress in the early acceleration phase of the throwing cycle (Sisto et al. 1987). The flexors are also important for wrist flexion during ball release. Because of these stresses, tendinopathy and myotendinous tears of the common flexor tendon are common in throwing athletes (Chung et al. 2004).
Patients with medial epicondylitis complain of pain over the medial epicondyle on palpation, forearm pronation, or resisted wrist flexion. Handball players with medial epicondylitis typically experience pain at the medial elbow during late cocking and early acceleration phases of the throwing cycle. Although the term “epicondylitis” is used, osseous inflammatory changes are not commonly seen. Abnormalities predominantly affect the common wrist flexor tendon origin (Chung et al. 2004).
On radiography, patients with medial epicondylitis may demonstrate calcification at the flexor/pronator muscular origin. On MRI, the common flexor/pronator tendon is optimally assessed on coronal images. MRI findings of medial epicondylitis include increased tendon thickness of the flexor/pronator tendons, with T2 high signal intensity if mucoid degeneration is present (Miller and Savoie 1994). Partial-thickness tendon tears on T2-weighted images are seen as partial tendon disruption with high signal intensity. Complete tears appear as fiber discontinuity of the flexor/pronator tendon on both T1- and T2-weighted sequences (Chung et al. 2004).
Medial Epicondyle Avulsion and Apophysitis
The elbow is a frequently injured joint in skeletally immature athletes, and medial epicondyle avulsion and apophysitis are commonly encountered lesions in young throwing athletes, although they can also occur in older athletes (Fig. 9.11). The medial apophyseal plate is biomechanically weaker than the anterior band of the ulnar collateral ligament and is thus more commonly injured secondary to valgus stresses generated at the elbow during throwing, although concomitant injuries to both the ulnar collateral ligament and the medial epicondyle can occur (Fig. 9.11). In addition, the flexor-pronator group of muscles exerts traction on the relatively weak growth plate during throwing. The combination of radiocapitellar compression injury and change relative to medial tensile stress is referred to as Little Leaguer’s elbow since it is commonly seen in young baseball pitchers (Bennett 1959), although this lesion also occurs in non-baseball athletes. Radiography may demonstrate fragmented medial epicondylar apophysis. There may be avulsion and displacement of the medial epicondyle ossification center. The fragment may become entrapped in the elbow joint or cause ulnar nerve damage. On MRI, variable signal may be seen in the fragmented medial apophysis and adjacent parent bone. Hyperintensity on T2-weighted images reflects bone marrow edema, and hypointensity represents sclerosis (Klingele and Kocher 2002; Ouellette et al. 2005).
Fig. 9.11
A 37-year-old male handball player with ulnar collateral ligament strain. Coronal fat-suppressed proton density-weighted MRI of the right elbow shows ulnar collateral ligament strain with common flexor tendon partial avulsion
9.3.2.4 Osteochondral Lesions and Loose Bodies
Lateral elbow pain may result from osteochondral injuries and osteochondritis dissecans of the capitellum, probably caused by compressive forces at the radiocapitellar joint during late cocking and early acceleration of the throwing cycle. A subchondral lucency with variable marginal sclerosis and fragment attachment at the capitellum represents osteochondral injury on radiography and CT. CT and CT arthrography are useful for the detection of subtle osteochondral abnormalities or for the assessment of detached fragments (Ouellette et al. 2005) (Fig. 9.12).
Fig. 9.12
A 30-year-old male handball player with chronic elbow pain. Axial CT arthrography image (a) demonstrates olecranon chondropathy (black arrow) and a loose body (white arrow). Sagittal reformatted CT arthrography images show posterior loose body (b, arrow) and capitellum chondropathy (c, arrow)
MRI is also helpful in the assessment of subtle osteochondral injuries of the capitellum which may be radiographically occult (Wenzke 2013). MRI may demonstrate capitellar articular cartilage irregularity and fissuring. Osteochondral lesions show decreased signal intensity on T1-weighted and increased signal intensity on T2-weighted images within the capitellum. On contrast-enhanced T1-weighted images, complete enhancement of the fragment or incomplete craterlike fragment enhancement is associated with favorable clinical outcomes with conservative treatment. Fragment displacement or circumferential fluid surrounding the osteochondral fragment on MRI is indicative of fragment instability (Mesgarzadeh et al. 1987). MR arthrography is useful for visualization of intra-articular loose bodies and fragment stability determination.
One should be aware of a common diagnostic pitfall, so-called pseudodefect of the capitellum, which is seen at the junction between the anterolateral capitellum and posterolateral aspect of the lateral epicondyle (Ouellette et al. 2005). This should not be mistaken for an osteochondral injury. Pseudodefect of the capitellum can be easily recognized by its typical location. An apparent defect should be cross correlated with the sagittal view to distinguish between a true defect and a pseudodefect (Ouellette et al. 2005).
9.3.2.5 Posterior Olecranon Impingement
Because of valgus overload syndrome, handball players may develop posterior and posteromedial olecranon osteophytes, which are frequently symptomatic. Olecranon osteophytes may fracture and become intra-articular loose bodies (Ouellette et al. 2005). Symptomatic posterior olecranon impingement may require surgical therapy.
9.3.3 Wrist
Athletic injuries to the wrist can occur as a result of a single traumatic event or following overuse and repetitive microtrauma. Conventional posteroanterior and lateral radiographs are the first-line modality in the diagnosis of suspected wrist injuries. Standard measurements of the wrist including radial inclination, palmer tilt, and ulnar variance can be performed on a properly positioned posteroanterior and lateral view (Rosner et al. 2004).
9.3.3.1 Carpal Fractures
Fractures of the carpal bones are common in athletes, with the scaphoid the most commonly fractured (Rettig 2003). Triquetral fractures represent the second most common form of carpal bone fractures, far behind those of the scaphoid (Bonnin and Greening 1944; Hey et al. 2011). Most triquetral fractures result from falls from standing height onto the outstretched hand (Hey et al. 2011). Three types have been described in the literature: cortical dorsal (the most common), body, and cortical palmar (Hey et al. 2011; Smith and Murray 1996). Although triquetral fractures were first described in the literature more than 80 years ago (Thompson 1933), the exact mechanism of injury remains controversial. Two major theories have been suggested: ligament avulsion fracture (Bonnin and Greening 1944; Smith and Murray 1996) and ulnocarpal impaction (Levy et al. 1979; Garcia-Elias 1987). Other less common theories include direct trauma to the dorsum of the hand or sudden resistance against a twisting motion of the wrist (Bartone and Grieco 1956).
The prevalence of carpal bone fractures may be underestimated because they may be occult or overlooked on radiographs and consequently undiagnosed or misdiagnosed as wrist sprain (Becce et al. 2013). It has been shown that radiography has low sensitivity (30 %, for all carpal bones) for the detection of carpal bone fractures compared to CT (Welling et al. 2008), and thus, CT should be considered after a negative radiographic finding if clinically warranted. MRI is also an option for cross-sectional imaging (Mack et al. 2003; Fotiadou et al. 2011), but its relatively high cost may preclude routine use of MRI in clinical practice (Fig. 9.13).
Fig. 9.13
A 55-year-old male recreational handball player with wrist trauma. Axial fat-suppressed T2-weighted MRI of the wrist (a) shows bone marrow edema of the triquetrum (arrow). Axial CT images (b, c) show bone avulsion of the dorsal aspect of the triquetrum (arrow)
9.3.3.2 Scapholunate Ligament Tear
The scapholunate ligament comprises volar, central, and dorsal components. Each of these has different histologic properties and biomechanical functions. The location of the injury and size of the lesion may have clinical implications regarding therapy and prognosis (Pappou et al. 2013). Injuries to the scapholunate (SL) interosseous are the most common ligamentous injuries in the wrist (Rettig 2003). The SL ligament is a key stabilizer of the proximal carpal row of the wrist, and its dorsal component is the most important (Kuo and Wolfe 2008). Scapholunate ligament injury typically occurs following a dorsiflexion injury, e.g., a fall on a pronated outstretched hand. In handball, this injury usually occurs as a result of excessive force applied to a hyperextended wrist in a player who sustains a fall (Lewis and Osterman 2001). The patient complains of dorsal wrist pain and swelling and may report a discernable popping sound with wrist motion. Patients may also experience a weakness of grip (Rosner et al. 2004). On clinical examination, there is tenderness to palpation 1 cm distal to the dorsoradial tubercle (Fufa and Goldfarb 2013).
A static increase in the scapholunate interval (scapholunate dissociation) and dorsiflexion of the lunate occur as a consequence of a complete tear of the scapholunate ligament associated with a tear of one or more extrinsic ligaments (Meade et al. 1990). In addition, rotatory subluxation (volar flexion) of the scaphoid occurs, and further dorsal and proximal translation of the capitate along with the distal carpal row will lead to a dorsal intercalated segment instability (DISI) deformity (Linscheid et al. 1972). DISI causes abnormal articular loading that leads to the degenerative changes known as scapholunate advanced collapse (SLAC) wrist (Crema et al. 2012).
Scapholunate ligament injury may be suspected with a widening of the SL interval of greater than 2 mm on AP radiograph. This widening can be exaggerated with an AP clenched fist view (Rosner et al. 2004). A common radiographic finding of scapholunate dissociation is the “cortical ring sign” which occurs due to abnormal orientation of the scaphoid with the scaphoid rotated and appearing foreshortened on the AP radiograph (Ritchie and Munter 1999).
MRI can depict partial or complete intrinsic ligament tears. The intrinsic ligaments are optimally visualized on coronal images. Complete tears appear as distinct areas of discontinuity of the ligament with fluid signal on T2/T2* contrast or STIR sequences (Fig. 9.14). Complete absence of the ligament is also indicative of a tear. In more advanced cases, there may be associated widening of the SL ligament interval similar to that seen on radiographs, particularly if two or more portions of the ligament are involved. Fluid pooling around the ligament, concomitant bone injury, and adjacent ganglia are other clues to underlying injury (Rosner et al. 2004). Depiction of disruption of the dorsal portion of the ligament is also important, as injury to the dorsal component means the loss of the most important stabilizer of the SL ligament (Timins et al. 1995; Rosner et al. 2004). MRI or MR arthrography can also demonstrate partial ligament disruptions. Partial disruptions frequently involve the volar portion of the ligament. MRI may depict a dysfunctional ligament that has healed with scarring (Rosner et al. 2004). A recent study showed, however, that conventional MRI is outperformed by CT or MR arthrography for imaging diagnosis of scapholunate ligament tears, with CT arthrography having the highest sensitivity, specificity, and accuracy for identifying which component of the scapholunate ligament was torn (Lee et al. 2013).
Fig. 9.14
A 33-year-old male handball player who fell on his right wrist. Coronal fat-suppressed T2-weighted MRI shows scapholunate ligament tear (arrow)
Multidetector CT (MDCT) arthrography accurately depicts partial or complete tears of the scapholunate ligament. Axial images are useful to evaluate partial or complete tears of the dorsal and volar components. Coronal images are useful to evaluate tears of the membranous (proximal) component. DISI can be evaluated on MDCT using sagittal images, from which the axis of the scaphoid, lunate, and capitate may be determined. For exact angle measurement, neutral positioning of the wrist is critical. As a result of scaphoid volar flexion and lunate dorsiflexion, the scapholunate angle is increased (normal angle, 30–60°). The capitolunate angle is also increased (normal angle, 0–30°) because of the lunate dorsiflexion (Crema et al. 2012).
9.3.3.3 TFCC Lesion
The triangular fibrocartilage complex (TFCC) is a major stabilizer of the distal radioulnar and ulnocarpal joints. The TFCC consists of the following structures: (1) a triangularly shaped fibrocartilaginous articular disk, (2) a meniscal homologue, (3) the ulnar collateral ligament, (4) dorsal and volar radioulnar ligaments, and (5) the extensor carpi ulnaris tendon sheath. The TFCC also coalesces to form extrinsic ligaments that extend distally to insert on the triquetrum, hamate, and fifth metacarpal. The articular disk extends from the sigmoid notch of the radius to insert on the fovea and ulnar styloid. Lesions of the TFCC may be confined to the articular disk or involve one or more components of the TFCC (Rosner et al. 2004).
Patients present with ulnar wrist pain and tenderness exacerbated by wrist and forearm motion. Traumatic TFCC tears are more common in younger patients including athletes and in those with ulnar-negative variance. The most common mechanism of injury in the athlete involves rapid twisting of the wrist with ulnar-sided loading, which often occurs in racquet sports, golf, and gymnastics, as well as handball (Ko and Wiedrich 2012). Traumatic TFCC tears frequently occur close to the radial insertion. Fluid accumulation within the distal radial ulnar joint is an important secondary sign for a radial-sided TFCC tear (Rosner et al. 2004). Ulnar-sided TFCC injuries are more difficult to diagnose. Positive MRI findings include altered morphology of the ulnar attachments, linear fluid extending to the surface of the peripheral TFCC, and excessive fluid localizing to this region particularly if the fluid extends below the expected location of the prestyloid recess (Sofka and Potter 2001). Ulnar-sided TFCC injuries heal spontaneously or can be repaired (Rosner et al. 2004).
TFCC injuries can be classified according to the Palmer classification (Palmer 1989). Type 1 injuries are traumatic and further subclassified into 1A (central perforation), 1B (ulnar avulsion with or without distal ulnar fracture), 1C (distal avulsion of the TFCC attachments to the lunate or triquetrum), and 1D (radial avulsion with or without sigmoid notch fractures). Type 2 injuries are degenerative and represent progressive stages of ulnocarpal impaction syndrome. Type 2 injuries are also further subclassified: stage 2A is characterized by thinning and degeneration of the undersurface of the articular disk. Stage 2B indicates further TFCC degeneration with the addition of ulnolunate chondromalacia. Stage 2C represents TFCC perforation with ulnolunate chondromalacia. In stage 2D, TFCC perforation and ulnolunate chondromalacia are accompanied by lunotriquetral perforation. Stage 2E is characterized by each of the findings seen in stage D with the addition of ulnolunate arthritis (Rosner et al. 2004) (Figs. 9.15 and 9.16).
Fig. 9.15




A 21-year-old male handball player with chronic ulnar-sided pain of the wrist. Coronal fat-suppressed proton density-weighted MRI demonstrates high signal of the triangular fibrocartilage complex ulnar attachment (Palmer lesion type 1B, arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree