Fig. 25.1
The mechanism of (non-jump) serving
Fig. 25.2
The mechanism of setting
Fig. 25.3
The mechanism of spiking
Fig. 25.4
The mechanism of blocking
Because volleyball is considered as a non-contact game (players from the opposing teams are separated by a net), one would assume that the incidence of volleyball-related injuries would be low, especially compared to other sports that involve physical contact. On the other hand, forceful and rapid movements of the whole body occur in many directions when playing volleyball, and different movement patterns are involved in jumping, landing, and hitting (with forceful and rapid overhead movements of the arm and hand when spiking the ball). Because of the relevant biomechanical forces involved in these actions and movements, it is inevitable that injuries will occur. Furthermore, the “non-contact” characteristic is not always true since direct contact may exist during a volleyball game, with contact injuries often resulting from blocking and spiking actions, during either the match or training. The incidence of volleyball-related injuries varied in previous reports, from 1.7 to 3.0 injuries per 1000 h–15. Previous reports support that the majority of injuries sustained in volleyball games occur with players at frontline positions, which is where jumping and landing occur most often, with most of these injuries involving the lower extremity, primarily the ankle (Verhagen et al. 2004; Bahr et al. 1994; Agel et al. 2007). Furthermore, injuries occurring or reported during the match are likely more prevalent than those reported during training (Verhagen et al. 2004; Bahr and Bahr 1997).
Two main categories of injuries appear to be particularly relevant in volleyball in terms of incidence: overuse and acute injuries. Overuse injuries are related to repetitive mechanical stress in some regions or joints of the body and are related to specific movements and actions during matches and training as described above. Acute injuries are often related to direct or indirect acute trauma in a given region or joint of the body and may occur in several ways during the match or training. Because of the broad spectrum of injuries as well as the body parts affected in volleyball, in this chapter we will focus on the most common injuries and their most common sites and discuss the imaging methods available for their detection as well as their imaging features.
25.2 Ankle
Acute ankle sprain is the most commonly reported injury in volleyball players, with a prevalence between 26 and 55 % of all volleyball-related injuries (Watkins and Green 1992; Vanderlei et al. 2013; Augustsson et al. 2006; Verhagen et al. 2004; Bahr and Bahr 1997; Bahr et al. 1994; Agel et al. 2007; Reeser et al. 2006; Solgard et al. 1995). Although the majority of sprains about the ankle in volleyball are mild or moderate, they are relevant in daily practice since, on average, they may result in 4.5 weeks of recovery time and time lost from training or competition (Verhagen et al. 2004). Furthermore, it has been reported that ankle sprains account for approximately 23 % of all volleyball-related injuries leading to at least 10 days away from activity. Contact-related inversion sprains account for the vast majority of volleyball-related ankle injuries, mainly occurring in players at frontline positions (attacker, blocker). Very often, the attacker is taken across the center line when trying to catch a set which is too low and too close to the net. Then, the blocker, who jumps later than the attacker for tactical reasons, may land on the attacker’s foot under the net and is at risk of an ankle sprain (Fig. 25.5). Approximately half of ankle sprains in volleyball occur in such situation (Verhagen et al. 2004; Bahr et al. 1994). Another mechanism described for ankle sprains in volleyball is when a blocker, acting in a multi-player blocking at the net, lands on a teammate’s foot, which accounts for about one quarter of cases (Reeser et al. 2006). Middle blockers and attackers are at greatest risk for ankle sprain, with setters and defensive players at relatively low risk. Other risk factors for ankle sprain in volleyball include a previous sprain involving the same ankle (especially if sustained within the previous 6–12 months (Bahr and Bahr 1997)), neuromuscular control, spiking approach technique, court surface, and taping/bracing (Reeser et al. 2006). Over time, volleyball athletes are likely to develop ankle osteoarthritis mainly because of previous ligament injury and chronic lateral ankle instability. Although compared to age-matched controls, elite volleyball players develop more osteophytes and subchondral sclerosis around the ankle, to date there is no evidence that long term, high-intensity volleyball playing alone represents an independent risk factor for the development of ankle osteoarthritis.
Fig. 25.5
The most common type of ankle inversion sprain in volleyball. The blocker jumps later than the attacker for tactical reasons and may land on the attacker’s foot (or on a teammate’s foot) under the net
Imaging assessment of ankle sprains is mainly achieved with ultrasound and magnetic resonance imaging (MRI). Because of its high soft tissue contrast resolution and multiplanar capability, MRI is a major imaging tool for the assessment of sports-related injuries in the musculoskeletal system, including ankle sprain (Rosenberg et al. 2000). Since inversion ankle sprain is the most common mechanism of injury in volleyball and the anterior talofibular ligament (ATFL) is the weakest ligament around the ankle, the ATFL is the most frequently torn, followed by the calcaneofibular ligament (CFL) and the posterior talofibular ligament (PTFL). The degree of inversion ankle sprain is defined as first degree (partial or complete tear of the ATFL), second degree (both ATFL and CFL are partially or completely torn), and third degree (all 3 lateral ligaments partially or completely torn). Routine axial MRI may depict the morphology and signal of all ligaments at the lateral aspect of the ankle. Partial tears may lead to thickening or thinning of the ligament, with the ligament often displaying irregular margins and increased intrasubstance signal on fluid-sensitive sequences at the acute phase, which is indicative of intrasubstance edema or hemorrhage (Fig. 25.6). Complete tears are depicted when complete discontinuity or detachment of the ligament involved is seen (Figs. 25.7, 25.8, and 25.9). Coronal routine MRI is better suited for the assessment of the CFL (Fig. 25.9). Indirect signs of ligament injury at the lateral aspect of the ankle include obliteration/infiltration of the surrounding adipose tissues, extravasation of joint fluid into the adjacent soft tissues, as well as osseous contusions, with bone marrow edema seen mainly at the medial malleolus and the medial aspect of the talus. Mild insertional bone marrow edema may be depicted at the lateral malleolus or at the lateral aspect of the talus and/or calcaneus. Soft tissue hematomas may also appear in ankle sprain. Finally, reactive fluid within the adjacent tendon sheaths may be seen, especially within the peroneal tendon sheath in CFL injuries. Because eversion ankle sprain is rare in volleyball, injury involving the deltoid ligament is not frequently depicted when imaging is performed. Assessment of ligament integrity in cases of chronic ligament injury may be challenging when applying MRI. A decreased signal intensity of tissues surrounding the ligament affected is often present and indicates local scarring (Figs. 25.9 and 25.10) or chronic synovial proliferation. The ligament itself may present with thickening or thinning, often displaying wavy or irregular contours. Foci of ossifications or bony hypertrophic changes may be present as well.

Fig. 25.6
Acute partial tear of the anterior talofibular ligament. Axial fat-suppressed T2-weighted MRI of the ankle depicts thickening, irregular margins, and increased intrasubstance signal of the ligament (arrows). Note marked bone marrow edema of the talus particularly at its medial aspect, consistent with bone contusion, as well as mild insertional bone marrow edema of the lateral malleolus

Fig. 25.7
Acute complete tear of the anterior talofibular ligament. Axial fat-suppressed T2-weighted MRI of the ankle shows complete discontinuity of the ligament, with no fibers depicted at the usual site (*). Note marked bone marrow edema of the talus particularly at its medial aspect, consistent with bone contusion, as well as insertional bone marrow edema of the lateral malleolus
Fig. 25.8
Acute complete rupture of the anterior talofibular ligament. Axial T2-weighted MRI of the ankle depicts abnormal anterior displacement of ligament fibers (arrows) due to a proximal complete rupture, with thickening and increased intrasubstance signal of the remaining fibers also visible
Fig. 25.9
Acute complete tear of the calcaneofibular ligament. (a) Coronal-oblique T2-weighted MRI of the ankle shows a complete discontinuity with avulsion at the distal insertion of the ligament (arrow), with thickening of the remaining distal ligament fibers. Partial chronic tear of the calcaneofibular ligament. (b) Coronal-oblique T2-weighted MRI of the ankle shows diffuse thickening and low signal intensity of the calcaneofibular ligament (arrows), without discontinuity
Fig. 25.10
Chronic partial tear of the anterior talofibular ligament. Axial fat-suppressed T2-weighed MRI of the ankle depicts moderate thickening and low signal intensity of the ligament (arrow), without discontinuity
In experienced hands, ultrasound is a powerful imaging tool in the assessment of ligaments around the ankle joint and has the advantages of being widely available and inexpensive compared to MRI, and it allows dynamic evaluation of structures including ligaments (Fessell et al. 1998). Acute partial tears of ligaments at the lateral or medial aspect of the ankle are often depicted on ultrasound as a hypoechoic thickening or thinning of the involved ligament, with continuity of the fibers preserved in various degrees depending on the extent of the partial rupture. In acute complete ligamentous tears around the ankle, an anechoic focal complete discontinuity or detachment of the ligament may be depicted, often better assessed using dynamic ultrasound if clinical conditions allow (Fig. 25.11). The greatest advantage of ultrasound over MRI is dynamic assessment of chronic ligament injury, since it is possible to evaluate the continuity and morphology of the chronically torn ligament under tension by stressing it before applying ultrasound (Figs. 25.12, 25.13, and 25.14), even if a fair amount of scar tissue is present.
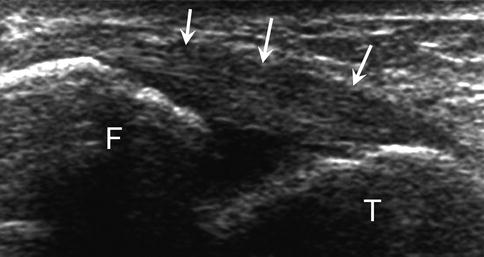
Fig. 25.11
Acute complete tear of the anterior talofibular ligament. (a) High-resolution grayscale longitudinal ultrasound image with ankle inversion stress (with the anterior talofibular ligament under tension) demonstrates a full-thickness anechoic defect of the ligament (arrow), with focal synovial fluid extravasation (*). Hypoechogenicity and thickening of the ligament fibers are also depicted. (b) Normal appearance of the anterior talofibular ligament on grayscale ultrasound image for comparison (arrows). F fibula, T talus
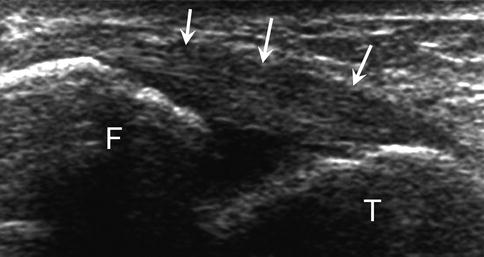
Fig. 25.12
Chronic partial tear of the anterior talofibular ligament. High-resolution grayscale longitudinal ultrasound image with ankle inversion stress (with the anterior talofibular ligament under tension) demonstrates moderate thickening and low signal intensity of the ligament (arrows), without discontinuity
Fig. 25.13
Chronic tear of the anterior talofibular ligament. (a) High-resolution grayscale longitudinal ultrasound image with ankle inversion stress (with the anterior talofibular ligament under tension) shows thinning and redundancy of the ligament (arrows), without discontinuity. Tensioning of the ligament is not adequate on dynamic ultrasound, a feature indicative of ligament insufficiency. F fibula, T talus. (b) Corresponding axial fat-suppressed T2-weighted MRI of the ankle depicts diffuse thinning of the anterior talofibular ligament (arrow)
Fig. 25.14
Chronic tear of the calcaneofibular ligament. (a) High-resolution grayscale longitudinal ultrasound image with ankle inversion stress (with the calcaneofibular ligament under tension) shows thinning and redundancy of the ligament (arrows), without discontinuity. Tensioning of the ligament is not adequate on dynamic ultrasound, a feature indicative of ligament insufficiency. (b) High-resolution grayscale longitudinal ultrasound image with ankle inversion stress (with the calcaneofibular ligament under tension) depicts a normal ligament with adequate tensioning after stress (arrows), a feature indicating ligament sufficiency. F fibula, C calcaneus
25.3 Knee
The knee is commonly affected by injuries in volleyball players. The majority of reports rank the knee as the second most commonly injured body part after the ankle (Augustsson et al. 2006; Verhagen et al. 2004; Bahr and Bahr 1997; Agel et al. 2007). A 10-year study including a large cohort of athletes showed a coefficient of 0.27 knee injuries per active volleyball member of regional sports clubs (Majewski et al. 2006). In volleyball players at good or elite levels, injuries of the knee joint represent 6–30 % of all volleyball-related injuries (Watkins and Green 1992; Vanderlei et al. 2013; Augustsson et al. 2006; Verhagen et al. 2004; Bahr and Bahr 1997; Agel et al. 2007; Solgard et al. 1995; Hell and Schonle 1985). Most knee injuries in volleyball do not involve direct external contact to the injured body part and are likely to represent chronic or overuse injury, with a gradual onset as reported by players (Augustsson et al. 2006). Patellar tendinopathy and internal derangements such as chronic meniscal or cruciate/collateral ligamentous injuries represent the majority of chronic/overuse injuries (Agel et al. 2007; Majewski et al. 2006). Volleyball players executing jumping and landing movements indoors are at a higher risk for chronic/overuse knee injuries. Acute knee injuries may occur in volleyball, such as anterior cruciate ligament injury (Ferretti et al. 1992), leading to much longer recovery times than chronic/overuse injuries. These injuries may be related to a direct contact mechanism in players in frontline positions (blockers and attackers at the net). Although there is lack of support in the literature, some sports medicine physicians involved in volleyball assume that there is an increasing incidence of acute anterior cruciate ligament (ACL) injuries due to the increase in bracing or taping for ankle protection in frontline players, which would transmit the load to the knees when landing, especially on another player’s foot. Fortunately, such conditions are much less frequent in volleyball than in other sports.
Anterior knee pain is a common complaint among volleyball players, and the most common diagnosis is by far patellar tendinopathy, also known as “jumper’s knee” (Blazina et al. 1973). Patellar tendinopathy is reported to affect around 40–50 % of male indoor volleyball athletes (Reeser et al. 2006; Lian et al. 2005; Ferretti 1986). Players with patellar tendon pain and abnormal imaging likely require longer recovery times (away from competition) or may never return to a pre-injury level (Ferretti 1986; Popp et al. 1997). In female volleyball players, however, other internal derangements about the knee such as meniscal and ligamentous injury seem to be more prevalent than patellar tendinopathy (Agel et al. 2007). Patellar tendinopathy represents mainly a chronic overuse injury and typically affects athletes engaged in sports requiring sudden knee extension or repetitive straining of the patellar tendon (excessive loading to the patellar tendon), such as running, kicking, and especially jumping. High-strain mechanical tendon loading may induce tenocyte apoptosis (programmed cell death), an important factor in the development of tendinopathy (Scott et al. 2005). It appears that any factor that increases the dynamic load to the patellar tendon would increase the risk of developing tendinopathy. Such factors include core stability, jumping ability, spike approach, landing technique, court surface, and intensity of training (Reeser et al. 2006). A previous study showed that anthropometric factors in men, especially a greater waist girth, are related to patellar tendinopathy in volleyball players (Malliaras et al. 2007). It has been suggested that there are several biomechanical factors that could be linked to patellar tendinopathy in volleyball players, such as high ankle inversion-eversion moments, high external tibial rotation and plantar flexion moments, large vertical ground reaction forces, and high rate of knee extensor moment development (Richards et al. 2002). Furthermore, a higher incidence of patellar tendinopathy was observed in athletes jumping the highest and landing from a spike (attack) with the deepest knee flexion angle (Lian et al. 2003). Also, valgus forces applied to the knee during the eccentric loading phase of the spike-approach takeoff (Richards et al. 1996), reduced dorsiflexion range of motion of the ankle (Malliaras et al. 2006), as well as diminished quadriceps and hamstrings flexibility (Witvrouw et al. 2001) are probably related to a higher frequency of patellar tendinopathy. Finally, there is some evidence to suggest that patellar tendinopathy is sex dependent, as it is more prevalent among men than women (Lian et al. 2005).
Clinically, symptom onset occurs gradually after a threshold of cumulative loading and ensuing tissue injury has been exceeded. The diagnosis of patellar tendinopathy is based primarily on clinical examination, still considered the reference standard for diagnosis, with athletes presenting with activity-related anterior knee pain associated with well-localized and palpable tendon tenderness (Cook et al. 2001; Peers and Lysens 2005). Imaging assessment is often performed, however, to evaluate the patellar tendon morphology, including the presence of ruptured tendon fibers at its proximal aspect. Imaging assessment of patellar tendinopathy may use both (grayscale and color Doppler) ultrasound and MRI. Routine axial and sagittal MRI is better suited for imaging the patellar tendon. On MRI, there are typically signal changes within the proximal aspect of the patellar tendon, especially at its deepest aspect, with an increase of signal intensity of the patellar tendon at this specific region. Care must be taken when evaluating the presence of signal changes using sequences with short time of echo (TE) such as T1 weighted or proton density weighted, since these are prone to magic angle artifacts which increase the tendon signal without representing pathology. It is of utmost importance to use sequences with longer TEs such as intermediate weighted, T2 weighted, or STIR. The presence of increased signal at the proximal and deep aspects of the patellar tendon in sequences with longer TEs indicates abnormal signal changes (Fig. 25.15). Also, thickening of the proximal aspect of the tendon, often exhibiting a “fusiform” pattern with an increase of the tendon size in the anteroposterior direction, may be present, as well as an ill-defined posterior border of the patellar tendon (Fig. 25.16). The presence of signal changes at the inferior pole of the patella is quite common, although the “edema-like” pattern is even more common. Ill-defined signal changes in the adjacent Hoffa fat pad may also be present. Partial-thickness or complete-thickness rupture at the proximal patellar tendon may be associated with patellar tendinopathy, mostly affecting or starting at the deepest aspect of the tendon, often depicted on MRI as a fluid-equivalent partial or complete defect better seen on fluid-sensitive MRI sequences, with relatively well-defined margins (Fig. 25.17), although this is not a rule. Intrasubstance rupture may be present as well in these cases (Fig. 25.18).
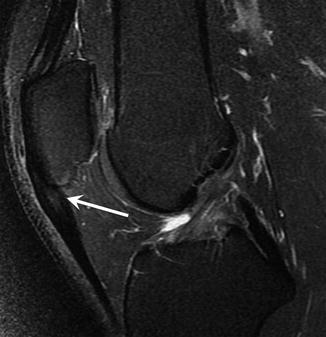
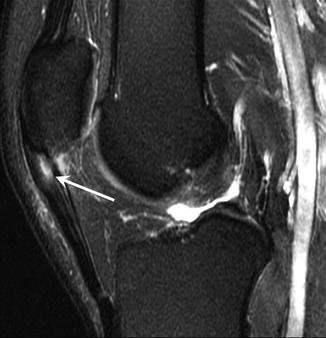
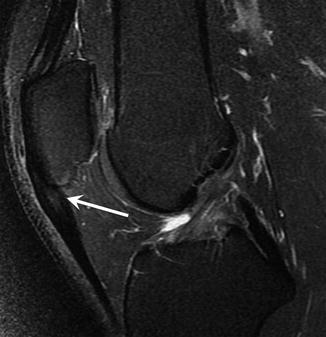
Fig. 25.15
Patellar tendinopathy (jumper’s knee). Sagittal fat-suppressed T2-weighed MRI of the knee shows fusiform thickening of the proximal patellar tendon, with focal increased intrasubstance signal intensity at its deepest aspect (arrow)
Fig. 25.16
Patellar tendinopathy (jumper’s knee). (a) Sagittal fat-suppressed T2-weighed MRI of the knee depicts moderate thickening of the proximal patellar tendon, with focal increased intrasubstance signal intensity mainly at its deepest aspect, as well as ill-defined posterior border of the proximal patellar tendon (arrow). Note mild insertional/reactive bone marrow edema of the inferior patellar pole. (b) Axial fat-suppressed T2-weighed MRI of the knee better depicts the irregular (ill-defined) posterior margin of the proximal patellar tendon (arrowheads)
Fig. 25.17
Patellar tendinopathy (jumper’s knee). (a) Sagittal fat-suppressed T2-weighed MRI of the knee shows fusiform thickening of the proximal patellar tendon, with a relatively well-defined focal partial tear at its deepest aspect (arrow). (b) Axial fat-suppressed T2-weighed MRI of the knee also nicely depicts the focal partial rupture of the proximal patellar tendon (arrow)
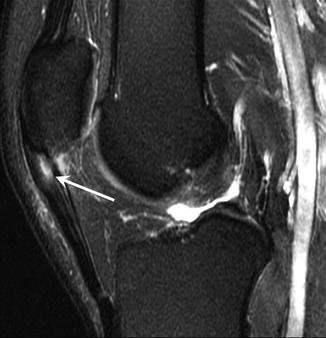
Fig. 25.18
Patellar tendinopathy (jumper’s knee). Sagittal fat-suppressed T2-weighed MRI of the knee demonstrates moderate thickening of the proximal patellar tendon, associated with a focal intrasubstance tear (arrow)
Ultrasound allows high-resolution imaging assessment of the patellar tendon when applying linear transducers with higher frequencies. Structural changes of the patellar tendon commonly depicted on ultrasound when imaging athletes with patellar tendinopathy include the presence of a hypoechoic region often present at the proximal and deep aspect of the patellar tendon (Fig. 25.19). Loss of posterior margin definition may be present as well. Also, a “fusiform” thickening of the proximal aspect of the tendon is easily depicted with ultrasound. Partial- or complete-thickness rupture of the patellar tendon is depicted on ultrasound as a relatively well-defined and anechoic region within the tendon, again mainly at the deep aspect of the proximal patellar tendon. Neovascularization of the patellar tendon may be assessed using color Doppler ultrasound (Fig. 25.19), and such assessment is ideally performed without stretching the patellar tendon (and consequent constriction of the blood vessels), with the knee extended and the quadriceps muscles relaxed.
Fig. 25.19
Patellar tendinopathy (jumper’s knee). (a) High-resolution grayscale longitudinal ultrasound image shows a focal hypoechoic zone at the deepest aspect of the proximal patellar tendon (arrow). (b) Correspondent color Doppler ultrasound image depicts moderate neovascularization adjacent to the proximal and deep hypoechoic zone of the tendon (arrow). P patella, ATT anterior tibial tuberosity
The accuracy of many of these imaging features assessed on MRI, grayscale ultrasound, and color Doppler ultrasound for identifying subjects with clinically diagnosed patellar tendinopathy was assessed in a cohort study, which found that all three methods were accurate, although both grayscale and color Doppler ultrasound were more accurate than MRI (Warden et al. 2007). Grayscale ultrasound, with a sensitivity of 87 %, had the best ability to categorize symptomatic patients over color Doppler ultrasound (70 %) and MRI (57 %). Color Doppler ultrasound had better specificity in categorizing asymptomatic subjects (90 %) than MRI (83 %) and grayscale ultrasound (83 %). Furthermore, a positive color Doppler ultrasound test indicated a strong likelihood an individual was symptomatic, with the authors stating that the combination of grayscale and color Doppler ultrasound probably represents the best combination for the confirmation of a clinically diagnosed patellar tendinopathy (Warden et al. 2007).
MRI is the best imaging method for the assessment of internal derangements of the knee in other cases of gradual onset of knee pain in volleyball players as well as for the assessment of acute ligamentous lesions, such as ACL tears (Figs. 25.20 and 25.21).
Fig. 25.20
Drawing illustrates a potential mechanism of ligamentous sprain of the knee joint, which may occur during landing (after blocking – as illustrated – or spiking the volleyball). A tear of the anterior cruciate and medial collateral ligaments after a valgus force is applied when landing as demonstrated
Fig. 25.21
Acute complete anterior cruciate ligament tear. Sagittal-oblique T2-weighted MRI (a, b, consecutive slices) shows a complete discontinuity of the anterior cruciate ligament at its proximal aspect (arrow). Note the associated joint effusion
25.4 Shoulder
The prevalence of shoulder injuries, pain, and dysfunction in volleyball athletes varies in different reports, accounting for 2–20 % of all volleyball-related injuries (Watkins and Green 1992; Vanderlei et al. 2013; Augustsson et al. 2006; Bahr and Bahr 1997; Agel et al. 2007; Briner and Kacmar 1997). In a recent survey including reports from 422 volleyball players, approximately 60 % reported a history of shoulder problems, with attackers and jump servers more likely to have shoulder problems than setters (Reeser et al. 2010a). Shoulder pain syndromes probably represent the third most common injuries in volleyball players and the second most common overuse-related injuries (Wang and Cochrane 2001; Reeser et al. 2006; Kugler et al. 1996). They are more commonly related to non-contact overuse injuries, with an injury incidence of 0.65 per 1000 athlete exposures reported in a large cohort of women’s collegiate volleyball (Agel et al. 2007). Shoulder overuse injuries were reported to represent 19 ± 11.2 % of volleyball-related injuries in a recent systematic review (Seminati and Minetti 2013). Although shoulder injuries in volleyball are not the most prevalent, these were reported to be responsible for the longest time of recovery (absence from competition) in volleyball players, with an average time loss of 6.5 weeks (Verhagen et al. 2004). Repetitive overhead swinging of the arms during serving and especially during spiking is probably the main mechanism of overuse shoulder injuries in volleyball (Fig. 25.22). Among the overhead volleyball skills, the spike (attack) is probably the most explosive one, being typically high-velocity and high-energy shots (Forthomme et al. 2005). In a single season, an elite volleyball player training between 16 and 20 h per week is expected to perform around 40,000 spikes (Kugler et al. 1996), and the players specialized in the attacking aspect of the game are the ones more likely to develop gradual onset of shoulder pain and dysfunction (Reeser et al. 2010a).
Fig. 25.22
Repetitive overhead swinging of the arm especially during spiking, as demonstrated here, is probably the main mechanism of overuse shoulder injuries in volleyball
The natural history of shoulder overuse pathology in volleyball players is probably similar to that of other “overhead athletes,” such as in baseball, tennis, and some track and field sports. There are some biomechanical similarities when comparing different overhead sports, so it would not be surprising that the developing injuries and structural abnormalities around the shoulder in these sports would be similar as well. Most published studies have focused on baseball (overhead throwing) (Patel et al. 2013; Anderson and Alford 2010), but an analogy with overhead volleyball skills (especially spiking and serving) could be made, and there are few studies that evaluated volleyball-related shoulder biomechanics and their possible consequences in terms of overuse-related injuries (Wang and Cochrane 2001; Kugler et al. 1996; Reeser et al. 2010b; Cools et al. 2005; Wang et al. 2000). However, data from a recent study on shoulder biomechanics during the volleyball serve and spike show some differences from other overhead sports moves such as baseball pitching and tennis serving (Reeser et al. 2010b). It seems that the kinetics of spiking and serving the volleyball may be less than that of tennis or baseball. Further, it was demonstrated that volleyball players usually present less glenohumeral internal rotation deficit on the dominant side than reported for baseball players (Reeser et al. 2010a; Reagan et al. 2002; Sabick et al. 2005; Schwab and Blanch 2009); they generate smaller maximum external rotation torques when compared to baseball and tennis players (Reeser et al. 2010b) and generate slower internal rotation angular velocities when spiking or serving the volleyball compared to pitching a baseball.
The force imparted to the ball during spiking or serving mainly originates from the torso, with the scapula responsible for providing a stable base of support in a way that the upper extremity will be correctly placed during the overhead actions. Since the glenohumeral joint is quite unstable anatomically, the dynamic stabilizers of the scapula and the humeral head will be critical in maintaining the functional integrity of the glenohumeral joint, allowing volleyball players to successfully serve and spike the ball. It has been demonstrated that the forces, torques, and angular velocities at the shoulder during both cross-body and straight-ahead spikes are higher than during roll shots and float serves in volleyball players (Reeser et al. 2010b). The same study concluded that shoulder kinetics similar to those in spiking probably exist during jump serves. Furthermore, the shoulder abduction angles at ball contact or release on volleyball spiking were demonstrated to be greater than previously reported for baseball pitches and tennis serves (Reeser et al. 2010b; Chu et al. 2009; Elliott et al. 2003). This supports that the shoulder girdle is exposed to exceptional cumulative load related to repetitive spiking and serving in volleyball players and may be a risk factor for rotator cuff impingement or labral damage. Chronic overload will directly affect the dominant shoulder girdles with some clinical features reported including depression and lateralization of the dominant scapula (Kugler et al. 1996) and the constellation of findings known as the “SICK” scapula, including scapular malposition, inferior medial border prominence, coracoid mal position and pain, and scapular dyskinesis (Burkhart et al. 2003). It is possible that the SICK scapula contributes to the development of suprascapular neuropathy (Ferretti et al. 1998; Safran 2004), which is a condition that may affect up to 45 % of elite ‑volleyball athletes (Reeser et al. 2006). Entrapment of the suprascapular nerve occurs at the level of the coracoid notch, and repetitive and abrupt movements of the scapula may cause repeated nerve stretching at this location. Denervation of the supraspinatus and infraspinatus muscles will lead to poorly localized pain and loss of strength when abducting and externally rotating the arm (muscle atrophy). It has been demonstrated that the infraspinatus and teres minor muscles act eccentrically to control the movement of the humerus during overhead moves, which provides a stabilizing posterior restraint to anterior subluxation in the acceleration phase of such movements (Rokito et al. 1998). Spiking is a special example, with the arm placed in horizontal abduction and external rotation. Eccentric overload and repetitive stress on rotator cuff tendons and capsule are probably relevant factors for volleyball-related overuse injuries. External/subacromial impingement is one of the most frequently reported overuse injuries in volleyball (Seminati and Minetti 2013). Each time the upper arm is elevated above the shoulder level (e.g., serving, setting, or spiking), there will be a narrowing of the space between the coracoacromial arch and the greater humeral tuberosity, with the supraspinatus tendon acting in a critical zone, where the vasculature may be affected and lead to further tendinopathy. Biceps involvement may also occur in volleyball (Seminati and Minetti 2013). Volleyball players are also at risk for internal impingement of the shoulder, characterized by excessive or repetitive contact of the greater tuberosity of the humeral head with the posterior and superior aspect of the glenoid when the arm is abducted and externally rotated (spiking and serving), which may lead to impingement and injuries of the rotator cuff, mainly articular-side partial-thickness tears of supraspinatus and/or infraspinatus, posterior and/or superior labral lesions, Bennett lesions, humeral head osteochondral lesions or cysts, and posterior glenoid bony lesions (Heyworth and Williams 2009). Finally, acute contact or non-contact injuries around the shoulder such as luxation or muscle strain have also been reported (Seminati and Minetti 2013).
Routine MRI of the shoulder is the best imaging method for the initial assessment of gradual onset of shoulder symptoms in volleyball players, allowing assessment of the whole joint with high soft tissue contrast resolution. Many authors advocate the use of MR arthrography (MRA) with intra-articular injection of a dilute gadolinium solution, which will distend the joint allowing for improved visualization of intra-articular structures and detection of labral tears and undersurface rotator cuff tears (Magee 2009; Magee et al. 2004; Tuite 2003; de Jesus et al. 2009). Further acquisitions with the arm in abduction and external rotation are widely performed in overhead athletes. The position increases the ability of MRA to detect undersurface rotator cuff tears, and it places the anterior stabilizing structures under tension (Tirman et al. 1994a; Cvitanic et al. 1997). On the other hand, applying the appropriate pulse sequences for imaging of the shoulder, non-contrast-enhanced MRI showed equivalent or even superior diagnostic performance in the detection of shoulder pathology including labral tears (Chandnani et al. 1993; Gusmer and Potter 1995; Connell et al. 1999). That being said, the initial assessment of the shoulder in volleyball players should probably be performed with routine non-contrast MRI, and if the diagnosis cannot be made with confidence by the radiologist, MRA would be the next step. In addition to MRI and MRA, rotator cuff tears in external and internal impingement may be also assessed using ultrasound. Ultrasound has been shown to provide similar diagnostic ability in comparison to MRI in a recent meta-analysis (de Jesus et al. 2009). In internal impingement, superficial undersurface fraying or tears of the posterior cuff tendons (mainly the infraspinatus) are depicted as focal partial-thickness defects exhibiting fluid-equivalent signal on MRI and echogenicity on ultrasound (Fig. 25.23). MRA with ABER may improve visualization of these tears (Tuite 2003; Tirman et al. 1994b). Other accompanying features of internal impingement may also be depicted on MRI or MRA, including fraying or tears of the posterior superior glenoid labrum (Figs. 25.23 and 25.24) and fibrocystic changes in the bone marrow at the greater tuberosity or superior glenoid. In cases of external impingement, supraspinatus tendinopathy is often depicted as thickening of the tendon with diffuse changes in signal (MRI) and echogenicity (ultrasound). Fluid-equivalent signal (or contrast) and echogenicity may be detected within the substance of the tendon (intrasubstance tear), at the articular or bursal surface of the tendon in cases of focal partial-thickness tears, or extending across the tendon representing full-thickness tears (Figs. 25.25 and 25.26). Changes in the morphology at the level of the coracoacromial arch may be also depicted in different imaging techniques. Superior labrum anterior to posterior (SLAP) tears may be detected in volleyball players using MRI or MRA, although it is more commonly depicted in throwers (Anderson and Alford 2010). Fluid or contrast extending between the superior labrum and the adjacent glenoid and different types of SLAP may be depicted (Figs. 25.27 and 25.28). It may be difficult to differentiate between a true SLAP tear and a normal sublabral sulcus, and some features on MRI or MRA may help in distinguishing these (Fig. 25.29). Anterior and posterior labral tears may also be depicted in volleyball players. MRI is probably the most useful imaging technique to assess suprascapular neuropathy in volleyball players. Because the mechanism of nerve injury is related to chronic mechanical stretching of the suprascapular nerve, no abnormalities of the suprascapular neurovascular bundle are found in the majority of cases. The MRI features of neuropathy include signs of muscle denervation, with the supraspinatus and/or the infraspinatus displaying denervation edema of the fibers in the acute/subacute phases (Fig. 25.30) or fatty changes and muscle atrophy in chronic cases. MRI and ultrasound may be used in cases of suspected muscle strain around the shoulder in volleyball players. Computed tomography arthrography (CTA) is also a powerful imaging tool for the assessment of rotator cuff and labral pathology, exhibiting diagnostic performance equivalent or superior to MRI and MRA (Lecouvet et al. 2008; Tuite and Rubin 1998). However, CTA has some disadvantages when compared to MRI, such as its poor ability to evaluate soft tissues around the joint. Thus, CTA is probably not the best imaging technique for the initial assessment of shoulders in overhead athletes.