Knee
Thomas H. Berquist
Protocols
Radiographs or computed radiography images
Routine images
Anteroposterior (AP) and lateral (minimum two views)
Trauma
AP, lateral (cross-table preferred to detect lipohemarthrosis), both obliques
Patella
Lateral and tangential (sunrise) views
Orthopedic series
AP standing, AP standing with flexion, lateral, and patellar views
Additional techniques
Notch views
Stress views (varus, valgus, AP)
Computed tomography (CT)
Helical CT images at 1-mm thick sections at 0.5-mm intervals (can be reformatted in the coronal and sagittal planes)
Bone and soft tissue window settings
Magnetic resonance imaging (MRI) (Table 5-1)
Extremity coil, knee slightly flexed (5 to 10 degrees)
TABLE 5-1 MAGNETIC RESONANCE SCREENING EXAMINATION OF THE KNEE | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Skeletal Trauma: Osteochondral Fractures
Key Facts
Fractures involving the joint surface result from direct blows or shearing forces.
Fractures may be subtle, requiring CT or MRI for detection.
Osteochondral patellar fractures are commonly associated with dislocation.
Associated soft tissue injury is common.
 FIGURE 5-1 Patellar view demonstrating subluxation after reduction of a patellar dislocation. There is a displaced osteochondral fragment (arrow) laterally. |
Suggested Reading
Capps GW, Hayes CW. Easily missed injuries about the knee. Radiographics 1994;14:1191–1210.
Dezell PB, Schils JP, Recht MP. Subtle fractures about the knee: Innocuous appearing yet indicative of internal derangement. AJR Am J Roentgenol 1996;167:699–703.
Skeletal Trauma: Patellar Fractures
Key Facts
Patellar fractures account for 1% of all skeletal fractures.
The mechanism of injury is direct trauma (motor vehicle accidents 28%, falls 68%) or indirect trauma (4%), such as quadriceps contraction.
Types of patellar fracture: transverse or oblique 34%; comminuted 16%; longitudinal 28%; apical or basal 28%.
A bipartite patella involves the upper outer quadrant. It usually is bilateral and should not be confused with a fracture.
Routine radiographs (AP, lateral, patellar views) usually are diagnostic.
Treatment includes reduction with internal fixation for displaced fractures. Fractures with less than 2 to 3 mm of displacement and articular surface congruency can be treated conservatively (casting). Badly comminuted fractures may require partial or complete patellectomy.
Complications
Osteoarthritis
Nonunion
 FIGURE 5-4 Lateral (A) and patellar (B) views after reduction with K-wires and tension band. The articular surface is reduced. |
Suggested Reading
Bostrom A. Fracture of the patella. Acta Orthop Scand Suppl 1972;143:1–80.
Skeletal Trauma: Supracondylar Fractures
Key Facts
Supracondylar fractures involve the distal 9 cm of the femur. Fractures of the distal femur account for 7% of all femoral fractures. Open injuries account for 5% to 10%.
Intra-articular extension is common. These complex fractures are difficult to manage.
Associated tibial plateau fractures are common.
Mechanisms of injury include minor trauma to the flexed knee in elderly patients and high-velocity forces applied to the anterolateral, lateral, or medial aspect of the knee.
Routine radiographs (AP and lateral) are diagnostic.
Treatment may be conservative (casting or traction) or operative to reduce and achieve restoration of the joint and leg length.
Complications:
| Early | Late |
|---|---|
| Vascular injury | Infection |
| Infection | Nonunion |
| 1% of closed | Malunion |
| 20% of open | Osteoarthritis |
| Failed reduction |
 FIGURE 5-6 AP (A) and lateral (B) radiographs of a severely comminuted complete articular fracture. Note the loss of length and posterior rotation (arrow) of the distal fragment in (B). |
Suggested Reading
Fraser RD, Hunter GA, Waddle JP. Ipsilateral fractures of the femur and tibia. J Bone Joint Surg 1978;60B:510–515.
O’Brien P, Meek RN, Blachut PA, et al. Fractures of the distal femur. In: Bucholz RW, Heckman JD, eds. Rockwood and Green’s fractures in adults. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2001:1731–1773.
Orthopedic Trauma Association Committee on Coding and Classifications. Fractures and dislocations compendium. J Orthop Trauma 1996;10(suppl):41–45.
Skeletal Trauma: Proximal Tibial Fractures
Key Facts
Proximal tibial fractures may be extra-articular or articular (tibial plateau or condylar fractures).
Tibial plateau (condyle) fractures account for 1% of all fractures and 8% of fractures in the elderly. The majority (55%–70%) of plateau fractures involve the lateral plateau. Isolated medial plateau factures occur in 10% to 23% of cases, and medial and lateral fractures occur in 10% to 30% of cases.
Mechanism of injury is motor vehicle accidents (54%) or falls (46%) leading to vertical compression (T and Y fractures) varus and valgus forces (medial and lateral plateau fractures, respectively).
Ligament and meniscal injuries are common with varus, valgus, or twisting forces.
AP and lateral radiographs usually are diagnostic for displaced fractures.
CT and MRI frequently are indicated to evaluate fragment position and soft tissue injury.
Management is based on four key factors: degree of articular depression, degree of fragment separation, degree of comminution, and extent of soft tissue injury.
Depression of 4 to 8 mm and separation of fragments 4 mm or more generally indicate a need for internal fixation.
Complications include infection, nonunion, and arthropathy.
Ipsilateral, femoral, and tibial condylar fractures are not uncommon and have the following significant associated injuries:
Abdominal and chest injuries 20%
Open injury to leg 60%
Neurovascular injury 7%
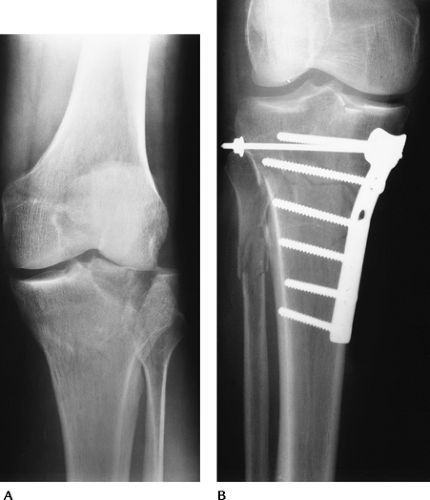 FIGURE 5-9 (A) Tibial plateau fracture with splitting and separation laterally. (B) Tibial plateau fracture reduced with buttress plate and screws to restore joint congruency. |
 FIGURE 5-10 CT images in the axial (A), sagittal (B), and coronal (C) planes demonstrating a minimally depressed fracture (arrows) with minimal articular displacement (open arrow). |
Suggested Reading
Hohl M. Tibial condylar fractures. J Bone Joint Surg 1967;49A:1455–1467.
Skeletal Trauma: Miscellaneous Fractures
Key Facts
Other tibial and femoral fractures include avulsion fractures, tibial spine fractures, tuberosity fractures, physeal fractures, stress fractures, and bone bruises.
Subtle osseous injury may be initially detected by the presence of a lipohemarthrosis on cross-table lateral radiographs.
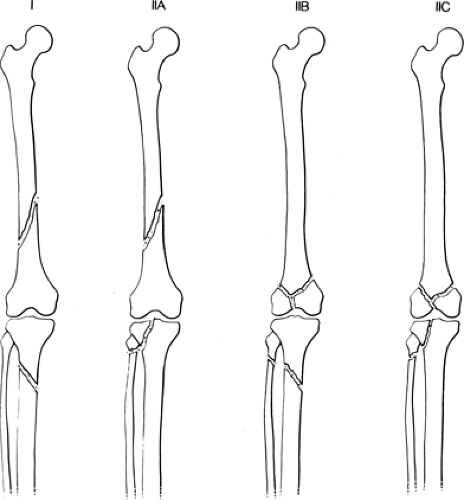
Physeal fractures about the knee account for only 0.5% to 3% of physeal injuries. Femoral physeal fractures are more common because of the ligament support of the knee. Most injuries are Salter-Harris Types I and IV.
The second fracture is an avulsion injury at the insertion of the middle third of the capsular ligament on the upper lateral tibia. Anterior cruciate ligament (ACL) tears are associated in 75% to 100% of cases.
Stress fractures of the tibia and femur are subtle early radiographically. MRI has replaced radionuclide scans for more effective and specific early diagnosis.
Bone bruises usually are not evident on radiographs but easily detected with MRI. Associated meniscal and/or ligament injuries are common and also easily appreciated on magnetic resonance (MR) images.
 FIGURE 5-11 Ligament support about the knee. (A) The tibial physis is within the ligament support, and the femoral physis is proximal resulting in greater risk for fracture (B,C). |
 FIGURE 5-16 Cross-table lateral radiograph demonstrating a lipohemarthrosis (arrows) indicating an intra-articular fracture. |
 FIGURE 5-17 (A) AP radiograph is normal. (B) Coronal T1-weighted image clearly demonstrates the stress fracture (arrow). |
Suggested Reading
Dezell PB, Schils JP, Recht MP. Subtle fractures about the knee: Innocuous-appearing yet indicative of internal derangement. AJR Am J Roentgenol 1996;167:699–703.
Meniscal Lesions: Meniscal Tears
Key Facts
Meniscal tears are the most common cause of knee pain and instability.
Patients present with pain, locking, or “giving way.”
Tears may be the result of acute trauma or repetitive trauma with progressive degeneration.
The lateral meniscus is C-shaped and less firmly attached to the capsule (separated posteriorly by popliteus tendon sheath). The medial meniscus is more firmly attached, and the posterior horn is larger (Fig. 5-19).
MRI has replaced other imaging techniques for diagnosis of meniscal tears. Tears are most easily identified on spin-echo proton density images. Conventional spin-echo sequences are 93% sensitive compared with 80% for fast spin-echo sequences. Sagittal, coronal, and axial image planes should all be evaluated to properly characterize the type of tear.
Meniscal tears are described by configuration and location. The posterior horn is most commonly involved.
MR criteria for classifying meniscal tears have been clearly defined (Fig. 5-21).
Treatment depends on the location (peripheral vs. central) and type of tear. Peripheral tears may heal or be repaired as in the vascular zone. Displaced fragments may be removed arthroscopically. Allograft replacement is an evolving technique.
 FIGURE 5-20 (A) Types and appearances of meniscal tears. (B) Meniscal tears seen in the axial and coronal planes. |
 FIGURE 5-23 Gradient-echo sagittal image of a linear tear (arrowheads) in the posterior medial meniscus. |
Suggested Reading
Blackman GB, Majors NM, Helms CA. Comparison of fast spin-echo versus conventional spin-echo MRI for evaluation of meniscal tears. AJR Am J Roentgenol 2005;184:1740–1743.
Crues JV III, Murk J, Levy TL, et al. Meniscal tears of the knee: Accuracy of MR imaging. Radiology 1987;164:445–448.
Harper KW, Helms CA, Lambert HS III, et al. Radial meniscal tears: Significance, incidence, and MR appearance. AJR Am J Roentgenol 2005;185:1429–1434.
Wright DH, Desmet AA, Norres M. Bucket-handle tears of the medial and lateral menisci of the knee: Value of MR imaging in detecting displaced fragments. AJR Am J Roentgenol 1995;165:621–625.
Meniscal Lesions: Postoperative Meniscus
Key Facts
Menisci may be partially or completely resected or repaired.
Image features applied to diagnosis of meniscal tears (increased signal intensity extending to the articular surface and displaced fragments) can be applied after repair.
Intra-articular gadolinium may improve accuracy for evaluating the postoperative meniscus. Intra-articular gadolinium is 92% accurate for detection of retear.
Arthroscopy is most useful in complex or equivocal cases.
Suggested Reading
Lum PS, Schweitzer ME, Bhatea M, et al. Repeat tear of postoperative meniscus: Potential MR imaging signs. Radiology 1999;210:183–188.
Magee TH, Shapiro M, Rodriguez J, et al. MR arthrography of the postoperative knee: For which patients is it useful? Radiology 2003;229:159–163.
Meniscal Lesions: Meniscal Cysts
Key Facts
Meniscal cysts are reported in 1% of patients undergoing meniscectomy.
They are most common anterolaterally but can occur medially.
Meniscal tears usually are present and may be the basis for cyst formation.
Patients present with tenderness and joint-line swelling.
Meniscal cysts can be diagnosed with arthrography, but MRI is preferred.
Treatment requires decompression of the cyst and meniscal repair.
MR features include
Well-defined high-signal intensity lesion adjacent to or partially including the meniscus on T2-weighted sequences.
Cysts may be septated (47%) and up to 5 cm in size.
Ganglion cysts and cruciate ligament cysts may be confused with meniscal cysts.
Suggested Reading
Burk DL, Dalinka MK, Kanal E, et al. Meniscal and ganglion cysts of the knee. MR evaluation. AJR Am J Roentgenol 1988;150:331–336.
Campbell SE, Sanders TG, Morrison WB. MR imaging of meniscal cysts: Incidence, location, and clinical significance. AJR Am J Roentgenol 2001;177:409–413.
Meniscal Lesions: Discoid Menisci
Key Facts
Discoid menisci are reported in 1.5% to 15.5% of lateral and 0.1% to 0.3% of medial menisci.
Discoid menisci are broad and disk shaped and more prone to meniscal tears. Meniscal tears are more difficult to evaluate with discoid menisci because of degeneration and the high incidence of multiple tears.
The transverse diameter of a normal meniscus is 10 to 11 mm. A discoid meniscus projects farther into the joint and therefore appears larger on coronal and sagittal MR images (visible on three or more 4-mm-thick sagittal images).
Suggested Reading
Ryu KN, Kim IS, Kun EJ, et al. MR imaging of tears of discoid menisci. AJR Am J Roentgenol 1998;171:963–967.
Ligament and Tendon Injuries: Basic Concepts
Key Facts
Complete evaluation of the ligaments, tendons, and capsule is difficult with conventional techniques, including CT and arthrography.
MRI offers the ability to evaluate all supporting structures of the knee.
Key anatomic structures for image evaluation include
Anterior cruciate ligament (ACL): oblique course with anteromedial and posterolateral bands. Extends from the lateral femoral condyle to the tibial plateau.
Posterior cruciate ligament (PCL): thicker than ACL. Extends from medial femoral condyle to posterior intercondylar region of the tibia.
Medial collateral ligament (MCL): three layers. The first layer is composed of fascia covering the quadriceps, the second layer includes the MCL, and the third layer is the capsular ligament. The MCL extends from the medial femoral condyle to attach on the tibia approximately 5 cm below the joint line.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree