CHAPTER 5 ![]() MUSCULOSKELETAL SYSTEM
MUSCULOSKELETAL SYSTEM
WILLIAM E. ERKONEN AND CAROL A. BOLES
Congenital and Developmental Anomalies
Gout, Pseudogout, and Hemophilic Arthritis
Approach to Common Clinical Problems
When you think about it, bones are visible on nearly all radiographs. Therefore, radiologic anatomy of the musculoskeletal system is extremely important, but it is time-consuming to learn. Entire textbooks are dedicated to isolated joints, and there are just no shortcuts to mastering this detailed material. As always, a solid knowledge of normal image anatomy is a prerequisite for intelligent image evaluation. Remember that the anatomic structures are all the same—we are merely viewing them differently. Let us begin with normal image anatomy of the hand and move systematically cephalad to the shoulder girdle. This will be followed by normal image anatomy of the lower extremity from the foot to the hip.
The bones develop in a rather systematic fashion. Bone formation is by either intramembranous (transformation of mesenchymal tissue) or endochondral (conversion of an intermediate cartilage form) formation, or by both methods.
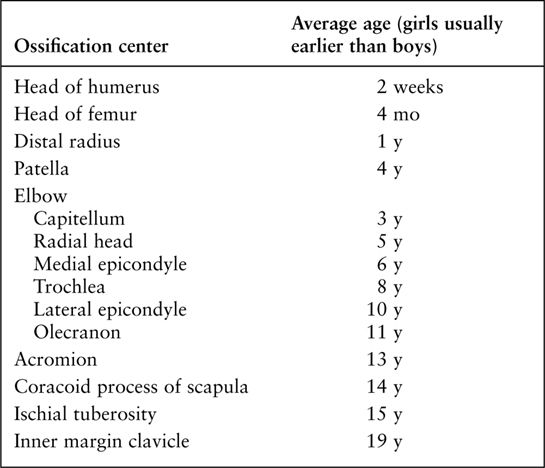
Many flat bones, such as the skull and mandible, form by intramembranous bone formation. Both methods are found in the extremities, spine, and pelvis. With endochondral ossification, cartilage is replaced by bone initiated at specific sites called centers of ossification. These centers of ossification appear in such a predictable order that they may be used for estimation of age. (Table 5.1) Understanding this aids in evaluation of fractures in the pediatric population as a small bone adjacent to a joint may be assumed to be an ossification center when it is, in fact, a fracture. The area of cartilage between the centers of ossification is often called the growth plate, or physis. Eventually, the centers of ossification fuse across the physis.
Joints develop between the developing ends of bone. There are three types of joints: synchondrosis, symphysis, and synovial joints. A synchondrosis has hyaline cartilage between the ends of bone and not movable while symphysis joints have fibrocartilage and a small amount of motion. Synovial joints have mesenchymal tissue converted into synovium, which will eventually produce fluid to lubricate these movable joints.
People commonly injure their extremities because they actively encounter the environment with their arms and legs. Consequently, you will probably order many radiographs of the extremities in your clinical practice. Thus, we need a system to evaluate upper and lower extremity images (Table 5.2). Each bone in an image must be carefully evaluated for density, variations of normal, and fracture. Also, each joint must be evaluated for width, smoothness of the articular surfaces, dislocation, arthritis, fracture, and foreign body. The soft tissues should be evaluated for edema, hemorrhage, masses, calcifications, and foreign bodies.
The hand is so complex that it is a subspecialty in both orthopedics and plastic surgery, so don’t expect to conquer the anatomy overnight. When you request radiographs of the hand, the standard study usually consists of posteroanterior (PA), oblique, and lateral views (Fig. 5.1). Remember that one of the most difficult aspects of medicine is to learn the jargon and routines, so we need to get the hand terminology correct from the beginning. Each digit of the hand must be properly named to communicate and document information accurately. The proper terminology for each digit and the numbering system for the metacarpals are displayed in Fig. 5.1A. Simply numbering the digits does not suffice, especially in situations in which digits are missing. Would you refer to the index finger as the first or second finger when the thumb is missing? So, beginning on the radial side of the hand, the thumb is always the thumb and not the first finger. Next is the index finger (not the second finger and not the first finger as some say there are four fingers and a thumb). Then the long finger (not the third or middle finger), the ring finger (not the fourth), and the small or little finger (not the fifth).
AVERAGE AGE OF APPEARANCE OF SOME MAJOR OSSIFICATION CENTERS
OBSERVATION CHECKLIST FOR BONE RADIOGRAPHS
Each bone should be evaluated for
Density
Anomaly
Fracture
Tumor
Foreign body
Infection
Each joint should be evaluated for
Articular surface smoothness
Symmetry
Fracture
Dislocation
Arthritis
Foreign body
Soft tissues should be evaluated for
Edema
Hemorrhage
Calcifications
Masses
Foreign bodies
Metacarpals (Fig. 5.1A) are numbered logically with the thumb articulating with the first metacarpal, the index finger with the second metacarpal, and so on. As a general rule, each hand digit has three phalanges except the thumb, which has only two. The phalanges are named proximal, middle, and distal. The joint between the proximal phalanx and the metacarpal is called the metacarpophalangeal (MCP) joint (Fig. 5.1A). The joint between the proximal and middle phalanges is the proximal interphalangeal (PIP) joint. The joint between the distal and middle phalanges is called the distal interphalangeal (DIP) joint. The thumb, with only two phalanges, has an interphalangeal joint. The distal-most aspect of the metacarpals and phalanges is the head, whereas the proximal portions are the bases. The central aspects of these bones are the shafts.

FIGURE 5.1 A: Right-hand oblique and posteroanterior (PA) radiographs. Normal. B: Right-hand lateral radiograph. Normal. C: Left-hand PA radiograph. Normal physis, epiphysis, metaphysis, and diaphysis. The cartilaginous physis is a lucent area on a radiograph.
Commonly used bone terms such as physis, epiphysis, metaphysis, and diaphysis can be confusing to the novice, but actually they are very simple. The locations of these entities are demonstrated in Fig. 5.1C. The physis (physeal or epiphyseal plate) is the growth plate as bone formation occurs on both sides (epiphysis and metaphysis) of the physis. The physis is the weakest part of a growing bone. The epiphysis is a secondary ossification center at the end of the bone, the metaphysis is just proximal to the physis, and the diaphysis (bone shaft) is between the proximal and distal metaphyses. Eventually, the epiphysis and the metaphysis fuse as the physis closes. The term apophysis is confusing and merely refers to an epiphysis that does not articulate with another bone and does not contribute to bone length growth but rather to bone contour. A typical example is the greater trochanter as seen in Fig. 5.23.
The wrist and forearm are common fracture sites, especially in children. If we are to intelligently understand and treat fractures in these areas, a thorough knowledge of wrist and forearm anatomy is very important. The appearance, location, and names of each carpal bone must be learned as well as their relationship to the distal radius and ulna. These relationships are well visualized on standard PA, lateral, and oblique radiographic views of the wrist (Fig. 5.2).
We generally obtain anteroposterior (AP) and lateral views of the forearm in children and adults (Fig. 5.3). Routine elbow radiographs consist of AP and lateral views (Fig. 5.4), but external rotation oblique views of the elbow may be requested on occasion (Fig. 5.5A). Radiographs of the humerus usually consist of AP (see Fig. 5.5A) and lateral views. Generally, an AP radiograph is obtained to evaluate the shoulder (Fig. 5.5B), and this is supplemented by either an axillary or lateral view of the shoulder depending on local practice. Musculoskeletal anatomy and disease can be nicely demonstrated by computed tomography (CT) and magnetic resonance imaging (MRI) (Table 5.3). CT imaging is especially good for bone detail, whereas MRI is good for soft tissue and bone marrow imaging, which can reveal edema caused by bone contusions or subtle fractures not seen on the radiographs. MRI is especially helpful in displaying the soft tissue structures around joints such as shoulder rotator cuff anatomy (Fig. 5.6).
FIGURE 5.2 Right wrist PA (A), oblique (B), and lateral (C) radiographs. Normal. Notice that the tip of the radial styloid is distal to the tip of the ulnar styloid and the radius articulates distally with the scaphoid and lunate carpals and laterally with the ulna (ulnar or sigmoid notch). The distal radial articular surface slopes toward the ulna and anteriorly (palmar). The distal ulna articulates with the radius laterally and wrist fibrocartilage distally. The ulna does not articulate directly with a carpal.

FIGURE 5.3 Right forearm AP (A) and lateral (B) radiographs. Normal. Note that in the correct lateral of the forearm, both the elbow and the wrist are in the lateral position. The distal radius is large and the proximal radius is small, whereas the distal ulna is small and the proximal ulna is large. The radius is far more important than the ulna in the wrist joint, whereas the ulna is more important in the elbow joint than the radius.
FIGURE 5.4 Left elbow AP (A) and lateral (B) radiographs. Normal. The elbow is usually flexed 90 degrees to minimize the appearance of the anterior and posterior fat pads. The dotted line on B indicates the ulna coronoid process.
FIGURE 5.5 A: Right humerus AP radiograph with external rotation of the humerus. Normal. The right elbow is in an oblique position. B: Right shoulder AP radiograph with external rotation of the humerus. Normal. Note the prominence of the greater tuberosity.
MUSCULOSKELETAL CT AND MRI INDICATIONS
Computed tomography
Bone detail
Fracture fragment evaluation
Bone tumor workup
Magnetic resonance imaging
Bone marrow imaging for occult fracture or metastasis
Soft tissue evaluation: ligaments, tendons, cartilages, and vessels
Bone tumor workup

FIGURE 5.6 Right shoulder coronal T1 MR image. Normal.

FIGURE 5.7 Right foot AP (A), oblique (B), and lateral (C) radiographs. Normal.
Now we approach lower extremity radiologic imaging by beginning with the foot and moving toward the hip. The standard views of the foot are AP, lateral, and oblique (Fig. 5.7). Naming of the toes is far easier than that of the fingers. The big toe or great toe may be referred to as the first toe, and the remaining toes are numbered sequentially ending with the little or fifth toe. Similarly, the metatarsals are numbered sequentially with the great toe articulating with the first metatarsal, the second toe articulating with the second metatarsal, and so forth. The ankle is usually imaged by AP, lateral, and either oblique or mortise-view (an internally rotated view) radiographs (Fig. 5.8). MRI may be used to image the ankle to detect soft tissue injury (Fig. 5.9). Radiographs of the tibia and fibula usually consist of AP and lateral views (Fig. 5.10).
Routine knee radiographs consist of AP and lateral views, and they may be supplemented by AP standing radiographs (Fig. 5.11A–C) and/or oblique views. Axial, coronal, and sagittal magnetic resonance (MR) images of the knee (Fig. 5.12) are commonly requested to evaluate injuries of the knee, particularly the nonosseous structures, including the medial and lateral menisci, articular cartilage, ligaments, tendons, and muscles. Remember that ligaments, tendons, and vessels have a low-intensity signal or appear black on MR images.
The femur and the hip joint are radiographed in the AP and lateral views (Fig. 5.13). A cross-table lateral view of the hip is frequently obtained in a trauma setting as seen in Fig. 5.68B.
FIGURE 5.8 Left ankle AP (A), oblique/mortise (B), and lateral (C) radiographs. Normal. Note how the mortise view (B) allows improved visualization of the distal tibiofibular articulation.
FIGURE 5.9 Right ankle sagittal T1 MR image. Normal. Note that the calcaneal (Achilles) tendon has a homogeneous low-intensity (black) signal.

FIGURE 5.10 Right tibiofibular AP (A) and lateral (B) radiographs. Normal.

FIGURE 5.11 Right knee AP (A), AP standing (B), and lateral (C) radiographs. Normal.

FIGURE 5.12 A: Right knee proton-dense sagittal MR image. Normal anterior cruciate ligament in a 36-year-old man. B: Right knee proton-dense sagittal MR image in the same patient. Normal posterior cruciate ligament. The posterior cruciate ligament (arrow) is more homogeneous and has a lower intensity signal (blacker) than the anterior cruciate ligament. C: Right knee proton-dense medial-sagittal MR image in a 32-year-old man. Normal posterior horn (straight arrow) and anterior horn (curved arrow) of the medial meniscus.

FIGURE 5.13 A: Right hip and proximal femur AP radiograph. Normal. Left hip AP (B) and frog-leg lateral (C) radiographs. Normal. See Fig. 5.68B for a true lateral of the hip.
There are several osseous variations of normal that can cause confusion for the novice (Table 5.4). One such variation of normal is the sesamoid bone, which is merely a normal extra bone, usually within a tendon. Sesamoids occur at numerous sites and are commonly found in the plantar aspect of the foot near the head of the first metatarsal (see Fig. 5.7) and in the palmar aspect of the hand near the head of the first metacarpal (see Figs. 5.1A and 5.14A–C), where they are actually located in the volar plate rather than in a tendon. When you think about it, the patella is actually a sesamoid bone or a bone within a tendon. Sesamoids function to decrease the moment arm and thus the work of a muscle. The quadriceps group of muscles becomes hypertrophied to compensate for increased work following removal of the patella.
NORMAL OSSEOUS VARIATIONS
Sesamoid bones (located within a tendon like the patella)
Ossicles (extra small bones)
Supernumerary epiphyses
Coalitions/fusions
Bone islands
FIGURE 5.14 Left wrist PA (A), left-hand oblique (B), and lateral (C) radiographs. Multiple sesamoids (arrows). Bone islands (curved arrows) are present in the head of the fifth metacarpal and the capitate, and they have no clinical significance. D: Left foot AP radiograph. Os tibiale externum (straight arrow) and os peroneum (curved arrow). Right knee anterior radiograph (E), tangential radiograph of right patella (F), and axial fat-suppressed MR image (G). Bipartite patella. Note that the patella has two sections and the accessory bone (curved arrows) usually lies superior and lateral to the main body of the patella. The axial image (G) shows the continuous cartilage over the ossification center (straight arrows) differentiating it from a fracture, which is rare in this superolateral position. H: Right wrist PA radiograph. Normal distal right radial epiphysis spur. This 21-year-old woman fell and had a painful wrist. This spur (arrow) is a variant of normal and must not be confused with a fracture. I: Right ankle AP radiograph. Accessory epiphysis near the tip of the distal tibia epiphysis in the region of the medial malleolus (arrow). This is a variant of normal.
FIGURE 5.15 Left wrist PA and oblique radiographs. Congenital fusion. There is coalition of the lunate and triquetrum (arrow) and a prominent scaphoid tubercle (curved arrow). This tubercle should not be confused with a fracture. Compare with the normal carpals in Fig. 5.2.
Ossicles are another variant of normal. They are small supernumerary or extra bones found in a variety of places in juxtaposition to the skeletal system and usually named after the neighboring bone (Figs. 5.14D and 6.16). The bipartite or multipartite patella (Fig. 5.14E–G) is another example of an accessory bone that should not be mistaken for a fracture. The condition results when one or more of the patellar ossification centers fail to fuse with the main patellar body. The result is that the patella has two or more sections, and this variant occurs superolaterally approximately 75% of the time. There is a strong male predominance.
Epiphyses can vary in appearance and in their number of ossification centers and still be normal (Fig. 5.14H, I). A sometimes confusing variant is a prominent scaphoid tubercle. This prominence can be mistaken for a fracture by even experienced clinicians (Fig. 5.15).
CONGENITAL AND DEVELOPMENTAL ANOMALIES
Osseous congenital anomalies are not uncommon, and a few of the many variations are illustrated in Figs. 5.16 to 5.19 and listed in Table 5.5.
Coalition refers to the failure of segmentation of bones during development, resulting in a congenital fusion. This fusion may be bony or fibrous. Common locations involve the lunate and triquetrum in the wrist (Fig. 5.15) and the calcaneus and navicular or calcaneus and talus in the foot (Fig. 5.16).
Osteogenesis imperfecta is a congenital, non–sex-linked, hereditary abnormality with the primary defect in collagen synthesis with deficient bone matrix. These patients have abnormal bones (Fig. 5.20) that are fragile, fracture easily, and are often deformed. Achondroplasia is a hereditary, often sporadic, autosomal-dominant anomaly manifested by shortened long bones that results in this most common form of dwarfism (Fig. 5.21).
The hip joint is the most common site of congenital dislocation and has a strong female predominance. Developmental dysplasia of the hip (DDH) was formerly known as congenital dislocation of the hip or congenital hip dysplasia. This dysplasia, shown in Fig. 5.22, is usually diagnosed in infancy. DDH is an abnormal development of the hip joint resulting in an abnormal acetabulum and femoral head. There is displacement of the femoral head referable to the acetabular cartilage. The femoral head usually displaces superiorly but can displace posteriorly. The acetabulum becomes shallow and the angle between the femoral head and shaft is widened.
SOME BONE ANOMALIES
Upper extremity
Supernumerary digits or polydactylism
Missing bones (fingers, radius)
Coalition (carpals)
Large digits or macrodactyly
Supracondylar process
Lower extremity
Polydactylism
Coalition (calcaneus with talus or navicular)
Developmental dysplasia hip
Slipped capital femoral epiphysis
Legg-Calvé-Perthes disease (avascular necrosis)
Talipes equinovarus (club foot)
Pes planus (flat foot)
Generalized
Osteogenesis imperfecta
Achondroplasia
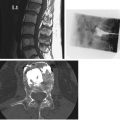
FIGURE 5.16 Lateral radiograph of the left ankle (A) and coronal CT image of the same patient (B). There is a prominent C on the radiograph (arrows). Compare with the normal lateral in Fig. 5.8. The coronal CT clearly shows continuous bone bridging (curved arrow) between the talus (T) and calcaneus (C).
FIGURE 5.17 Left-hand PA radiograph (child). Polydactylism. There are two thumbs and one first metacarpal. One thumb has three phalanges (straight arrows), and the other thumb has two phalanges (curved arrows).

FIGURE 5.18 Left forearm pronated, oblique radiograph. Absence of the radius, 1st metacarpal, and thumb. This 6-year-old had left hand and arm deformity at birth.

FIGURE 5.19 Right humerus lateral radiograph. Supracondylar process or spur (arrow). It is usually located in the anteromedial aspect of the distal humerus.
FIGURE 5.20 Left tibia and fibula lateral radiograph. Osteogenesis imperfecta. There is a healing, apex posterior, left tibia fracture (arrow). Note the thin serpentine appearance of the fibula and generalized osteoporosis.
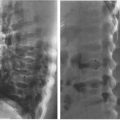
Two hip problems that can cause confusion are slipped capital femoral epiphysis (SCFE) and Legg-Calvé-Perthes disease (Table 5.6). SCFE (Fig. 5.23) is a hip problem that occurs during adolescence and is often associated with hip pain. The etiology is not understood, but there may be a history of trauma. Apparently, the physis becomes weakened during the rapid growth around puberty. The radiographic findings show the femoral head slipping or displacing posteriorly, medially, and inferiorly relative to the femoral neck. The proximal epiphysis becomes widened. Mild cases may go undetected and present with an earlier-than-expected onset of osteoarthritis.
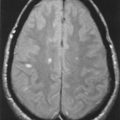
Legg-Calvé-Perthes disease (Fig. 5.24A) is a form of avascular necrosis, and the etiology is unknown. It may be referred to as osteochondrosis or coxa plana. It typically occurs in a boy between 5 and 10 years of age who complains of hip pain and walks with a limp. It occurs less frequently in females. The pain may be referred to the ipsilateral knee or the knee on the same side. Radiographic findings vary but may include increased density of the femoral capital epiphysis, femoral head flattening, rarefaction (bone demineralization) of the metaphysis, and medial joint space narrowing. In general, avascular necrosis or aseptic necrosis can occur in any joint (Fig. 5.24B, C) and can result from multiple other etiologies. Some of the other causes of avascular necrosis are listed in Table 5.7. The typical findings are sclerotic bone changes on one side of a joint that may go on to fragmentation and eventually to collapse or fracture. MRI (Fig. 5.24C) has proved particularly useful for the diagnosis of avascular necrosis prior to radiographic changes.
Extremity fractures are very common, so now is the time to discuss fractures in general. The initial imaging modality to evaluate for fracture should be a radiograph. Because a fracture or other osseous abnormality may be visible on only one of the radiographs, we obtain at least two views of a bone or joint that are 90 degrees to each other. Give yourself every opportunity to detect a fracture or other abnormality by obtaining as many views of an area as is practical. Never accept just one radiographic view of a bone or joint. When there is persistent concern for a fracture and the radiographs are normal, a clinical assessment is then needed. In many circumstances, the area of concern can be immobilized for a week and repeat radiographs obtained to see whether an occult fracture has now become visible. Other fractures are of such clinical importance that it is important to find out right away. The classic example is a hip fracture in an elderly patient for which an MRI should be obtained if the initial radiographs do not demonstrate a fracture. CT scans are the screening method of choice for cervical spine fractures are often used to better define a fracture prior to treatment.

FIGURE 5.21 Pelvis and lower extremities AP radiograph. Achondroplasia. The proximal long bones are shorter and wider than normal, especially the proximal tibias (straight arrows). The iliac bones are rounded (double arrows), and the acetabula are flat (curved arrow).
COMPARISON OF SLIPPED CAPITAL FEMORAL EPIPHYSIS (SCFE) AND LEGG-CALVÉ-PERTHES DISEASE (LCP)


FIGURE 5.22 Pelvis AP radiograph. Developmental dysplasia (DDH) of the right hip in a 14-year-old. The right hip is abnormal with a flattened femoral head (single arrow) and a poorly formed acetabulum (curved arrow). Compare the right hip to the normal left hip and note how the femoral heads remodel to conform to the shape of their corresponding acetabulum.

FIGURE 5.23 Pelvis AP radiograph. Bilateral slipped capital femoral epiphyses (SCFE) in a 15-year-old with chronic renal failure and on dialysis. The capital (proximal) femoral epiphyses (straight arrows) are displaced from their normal anatomic position. Usually, they are displaced inferiorly and posteromedially. There are monitoring electrodes projecting over the pelvis (curved arrows).
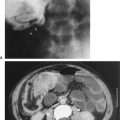
FIGURE 5.24 A: Pelvis AP radiograph. Legg-Calvé-Perthes disease. The right femoral head is normal. Note the irregular contour, flattened articular surface, and increased density of the left femoral head (straight arrow). The left hip joint space is widened (curved arrow). The left proximal femoral epiphysis is widened (double arrows), and the metaphysis is irregular. Note that the acetabulum is normal. B: Pelvis AP radiograph. Bilateral femoral head avascular necrosis of unknown etiology in a 42-year-old man. Both femoral heads (straight arrows) are sclerotic in appearance, and the right femoral head is deformed because of mild collapse or fracture. The right hip joint is narrowed laterally (curved arrow). C: Coronal T1-weighted MRI. Femoral head osteonecrosis in a patient on chronic steroids. The crescentic area formed by low-signal lines (straight arrows) represents the infracted regions. The left hip has a large amount of low-signal edema (curved arrows), suggesting a more acute infarction.
A PARTIAL LIST OF AVASCULAR NECROSIS ETIOLOGIES
Steroids and anti-inflammatory drugs
Trauma including fractures and dislocations
Sickle cell anemia
Hemophilia
Alcohol
Systemic lupus erythematosus
Renal transplant
Infection
Diabetes
In general, fractures can be conveniently divided into two major clinical categories:
- Simple or closed fracture means that there are bone fragments and the skin is intact.
- Compound or open fracture means the skin is not intact near the fracture. The skin has been penetrated by one or more of the bone fragments or by a penetrating foreign body.
Many terms applied to fractures are very descriptive and quite specific (Fig. 5.25A, B). Examples of straightforward common terms for describing fractures include the following:
- Spiral, transverse, oblique
- Nondisplaced
- Overriding
- Distracted
- Angulated
- Offset, or displacement, usually described by the percentage of the fracture fragments abutting or touching each other
Some fracture terms (Fig. 5.25C) that are not quite so obvious include the following:
- Torus fracture of the distal radius looks like the bump at the base of a Greek column and has nothing to do with a bull. This is an incomplete fracture that occurs in children. The bump is created by a buckling of the cortex without an obvious fracture line.
- Greenstick fracture describes a bone that fractures by bending like a green twig and is also incomplete.
- Comminuted or complex fracture indicates more than two bone fragments.
- Pathologic fracture is one that passes through abnormal bone such as a metastasis, a primary bone tumor, or a bone cyst.
- Stress fractures are secondary to unusual or excess stress, for example, tibial fractures in runners who overdo it.
- Insufficiency fractures describe fractures in bone with decreased strength, for example, caused by osteoporosis. Such a fracture may result from a normal stress such as merely walking across a room.
- An avulsion fracture is usually a fracture that occurs at the site of a tendon attachment. This fracture results when the tendon and muscle remain intact while the bone gives way (avulses) at the site of the tendon attachment to the bone.
The Salter-Harris classification of fractures (Fig. 5.25D) is helpful in describing and understanding fractures around a physis. Remember that the physis represents the weakest point in a bone.
Type I: The fracture involves only the physis.
Type II: The fracture involves the physis and metaphysis.
Type III: The fracture involves the physis and epiphysis.
Type IV: The fracture involves the physis, metaphysis, and epiphysis.
Type V: The fracture involves only the physis, but there is compression of the physis. This type is more serious than Type 1 because there is a high risk of the physis fusing as the fracture heals. As a result, the bone stops growing and is shorter than the opposite side.
When describing the position of displaced fracture fragments, we use another set of terms. Unfortunately, much confusion can be created by the nomenclature. Traditionally, the distal fragment is described relative to the proximal fragment. An alternative nomenclature uses the apex of the angle created by the fracture fragments as the key. If the apex of the fracture fragments points lateral, the fracture is described as apex lateral. (This same fracture is described as medially angulated by the other nomenclature. You can see where confusion may arise.) I prefer using the word apex in the description so that everyone understands which system is used. If the apex of the fracture fragments points medial, then it is apex medial angulation (Fig. 5.25E). One may substitute medial with volar, dorsal, radial, ulnar, or any other appropriate direction of angulation. Varus and valgus angulation are other common terms to describe angulation and are also illustrated in Fig. 5.25E. Another useful rule for describing fracture alignment describes the direction in which the distal fracture fragment is displaced (Fig. 5.25F).
The rate at which a fracture heals depends on the fracture site, type of fracture, patient age, adequacy of immobilization, nutrition, and presence or absence of infection. When a fracture occurs, there usually is an associated hemorrhage into the fracture site with subsequent hematoma formation around and between the fracture fragments. The fibrin in a hematoma serves as a framework for fibroblasts, osteoblasts, and a general inflammatory reaction. Bone matrix or osteoid appears in the repair process after a few days, and this is called soft callus or provisional callus. The soft callus is not visible on a radiograph. As calcium salts precipitate in the soft callus and new bone grows, this is called callus. As the callus gradually becomes more dense, it becomes visible on a radiograph. Eventually the callus becomes solid, and bone union is established between the fracture fragments.
FIGURE 5.25 A, B: Some common fractures (arrows) and the terms used to describe them and their alignment. C: Other common terms used to describe fractures (arrows). D: The Salter-Harris classification of physis fractures. The solid black line indicates the fracture (arrows), whereas the physis is indicated by the vertical black and white lines. E: Illustrations of the nomenclature used to describe fracture angulation. F: Nomenclature used to describe the direction of displacement of the distal fracture fragments.
FIGURE 5.26 Left-hand AP radiograph. Obvious severe hand injuries secondary to a corn-picking accident. The phalanges are essentially missing, and there are fractures of the metacarpals and carpals.
In a few days following a fracture, some absorption or removal of bone occurs as a part of the repair process near the ends of the fracture fragments. Because of this bone absorption, the fracture line becomes more visible on subsequent radiographs. This explains why some subtle fractures may not be visible on radiographs obtained immediately following injury but become visible approximately 7 to 10 days postinjury.
Self-explanatory terms used to describe problems in the fracture healing process include the following:
- Nonunion or nonhealing
- Delayed union
- Malunion
Fractures of the hands result from a wide variety of activities (Table 5.7). Some fractures and injuries are so obvious that the average citizen could spot them on a radiograph (Fig. 5.26). Subtle fractures can involve any bone and are common in the phalanges of the hand (Figs. 5.27 and 5.28). Joint dislocations occur in almost all joints, and the hand phalangeal joints are common dislocation sites, notably related to sports (Fig. 5.29). Metacarpal fractures are also common, and fractures of the fifth metacarpal often result from punching a solid object. These fractures are appropriately called boxer fractures although they clearly demonstrate an amateur status because professionals would strike using the second and third metacarpals (Fig. 5.30).
The most commonly fractured carpal is the scaphoid (Fig. 5.31). The carpal scaphoid is occasionally referred to as the navicular (an archaic term) by clinicians, but anatomists correctly call it the scaphoid. To add to the confusion, there is a tarsal navicular. Scaphoid fractures result from the injury lines of force being transmitted along the long axis of the thumb, and the majority of these fractures are located in the scaphoid waist. Because of the location of their blood supply and variable arterial branches, scaphoid fractures may develop complications such as nonunion and avascular necrosis, which may result in secondary development of arthritis. These complications are more apt to occur when there is delayed diagnosis and delayed or inadequate treatment. If a scaphoid fracture is suspected but the initial radiographs are negative, additional radiography, CT, or MR is indicated (Fig. 5.32).

FIGURE 5.27 Left thumb PA (A) and lateral (B) radiographs. Comminuted fracture (straight arrows) that extends to the articular surface of the interphalangeal joint (curved arrow). There is mild apex palmar angulation at the fracture site (double arrows).
FIGURE 5.28 Right index finger lateral radiograph. Mallet finger. The distal phalanx demonstrates a slightly flexed attitude due to fracture (arrow) at site of the insertion of the extensor digitorum mechanism. The loss of the extensor mechanism continuity with the distal phalanx allows the distal phalanx to assume a flexed position or a mallet finger.

FIGURE 5.29 Left-hand PA radiograph. Dislocation at the proximal interphalangeal (PIP) joint of the left long finger. The middle and distal phalanges are completely dislocated relative to the proximal phalanx. There are no fractures.

FIGURE 5.30 Right-hand PA oblique radiograph. Boxer or Saturday night fracture. The apex dorsal angulated fracture (arrow) is through the neck of the right fifth metacarpal.
FIGURE 5.31 Right wrist PA radiograph. Essentially nondisplaced fracture (arrows) of the scaphoid waist.

FIGURE 5.32 STIR (short tau inversion recovery) MR image of the right wrist. The initial radiograph was normal, but suspicion for fracture led to the MR scan. In this sequence fat is suppressed, so the bone marrow appears dark. Cartilage is gray and fluid is white. There is fluid signal within the scaphoid centered at the scaphoid waist (arrow) with adjacent cortical disruption confirming the suspected scaphoid fracture.
Using arms and outstretched hands to cushion falls often results in fractures about the wrist. Whereas young adults typically fracture the scaphoid, children and older adults are more likely to fracture the distal radius and ulna. One such common fracture is called the Colles fracture (Fig. 5.33). It is imperative to reduce these fractured bones as close to their normal anatomic alignment as possible. Anything less than anatomic realignment may result in a painful and/or poorly functioning wrist. Therefore, it is important to know that the radial styloid tip is 1 to 1.5 cm distal to the ulnar styloid tip, and the distal radial articular surface slopes 15 to 25 degrees toward the ulna and 10 to 25 degrees volar or anteriorly. These important relationships are summarized in Table 5.8. Children, however, have a remarkable ability to remodel and anatomic realignment is not usually needed, depending on the age of the child. In fact, to avoid future limb length discrepancy, anatomic realignment may be purposely avoided.
COMMON CAUSES OF UPPER EXTREMITY FRACTURES
Work injuries
Home falls
Recreational activities
Sports
Motor vehicle accidents
Fisticuffs
FIGURE 5.33 Right wrist PA, oblique, and lateral radiographs. Colles fracture. There are fractures of the distal radius (straight arrows) and the ulna styloid (curved arrows) with dorsal tilting of the distal radius fracture fragment. The pronator fat stripe is obliterated when compared with Fig. 5.1B. The ulna styloid is minimally displaced radially. Note that the radial length is maintained and the distal radius articular surface slopes toward the ulna on the PA view. However, the distal radius articular surface now slopes posteriorly on the lateral view; reduction will try to bring this to neutral or restore the volar (anterior) tilt.
A subtle fracture in the distal forearm of children is the torus fracture (Fig. 5.34). Torus does not refer to a bull but rather the convex molding/projection (torus) located at the base of a classical column. The torus fracture on a radiograph usually appears as a minimal bump on the bone without a visible fracture line. It represents a buckling of the bone cortex. However, most fractures of the radius and ulna that are encountered in practice are much more obvious (Fig. 5.35).
Elbow fractures (Figs. 5.36 to 5.38) and dislocations (Fig. 5.39A–D) can occur when children and adults fall directly on their elbow or on an extended arm or hand. In children, supracondylar fractures of the distal humerus are more common, but in adults, radial head or neck fracture predominates. In general, children are more likely to have a supracondylar fracture of the distal humerus and adults a radial head fracture. Dislocations of the elbow are named for the direction the radius and ulna dislocate relative to the humerus. When the radius and ulna dislocate anterior to the humerus, it is an anterior dislocation.
The radiographic anatomy of the elbow is complicated. This is especially true in children because of the presence or absence of multiple ossification centers. When in doubt about an elbow fracture or dislocation, the noninvolved elbow may be useful for comparative purposes as seen in Fig. 5.38A and B. This principle of comparative views applies to all areas of difficult anatomy. However, knowledge of the anatomy and ordered development of the ossification and fusion of the physes is fundamentally more important. Note that fractures and dislocations of the elbow can be a threat to the brachial artery because of its proximity to the distal humerus (Fig. 5.39E).
A very common injury to the shoulder occurs when a senior citizen trips on the rug or stairs. If they land on their extended hand and do not fracture their wrist, they may sustain a fracture of the surgical neck of the humerus (Fig. 5.40). Generally, this is very easily treated with a sling or a light hanging cast but may require an extended time for healing due to the patient’s age and the fewer stresses compared to a weight-bearing bone. A similar fracture can occur through the physis of the proximal humerus in children (Fig. 5.41).
Dislocation of the shoulder is another common injury that can occur in all age groups. In anterior dislocation of the shoulder, the humeral head becomes caudad or inferior to the glenoid cavity on an AP radiograph and an impaction fracture of the greater tuberosity, a Hillsach’s deformity, may result (Fig. 5.42A–C). Alternatively, the greater tuberosity may fracture during dislocation (Fig. 5.42D). In a posterior dislocation, the humeral head is often slightly cephalad to the glenoid cavity. However, a dislocation is often very difficult to diagnose on a single anterior view, and an axillary or scapular Y view should be obtained (Fig 5.42E). Anterior dislocation of the shoulder is much more common than a posterior dislocation. Associated fractures of the humerus or scapula and rotator cuff tears may occur. Neural and vascular injuries are much less frequent.
FIGURE 5.34 A: Left wrist PA, oblique, and lateral radiographs. Torus fracture (arrows) or a nondisplaced fracture of the distal left radius. Left wrist PA (B) and lateral (C) radiographs. Healing left radius torus fracture 6 weeks following the radiograph shown in A. The dense white zone (arrows) is the typical appearance of a healing fracture.

FIGURE 5.35 Right forearm AP (A) and lateral (B) radiographs. Greenstick fractures (straight arrows) of the distal radius and ulna. The fractures simulate a broken green twig or branch wherein the twig bends or breaks but does not separate. On the lateral radiograph, the fracture lines appear to involve only the anterior cortex of both bones. There is mild apex dorsal angulation. This will probably not be reduced because of the great bone remodeling capability in a child. Right forearm AP (C) and lateral (D) radiographs. Complete transverse fractures (arrows) of the distal shafts of the radius and ulna in a 15-year-old. There is mild apex volar, or apex anterior, angulation at the radius fracture site. The fracture fragments in the ulna are mildly offset. E: Right forearm AP radiograph. Healing fractures (straight arrows) of the radius and ulna in a young child. The fractures are remodeling to near-anatomic alignment, and the curved arrows indicate periosteal reaction and new bone formation. The fracture lines are not visible, suggesting early bone union.
FIGURE 5.36 Left elbow AP (A) and lateral (B) radiographs. Radial neck fracture. The straight arrows indicate the site of the fracture, and the radial head is tilted laterally on the AP view. The fracture is very difficult to see on the lateral view (straight arrows). A positive fat pad sign is faintly visible posterior to the distal humerus (curved arrow) on the lateral view, and this always means that one should carefully evaluate for a fracture. A visible fat pad anterior to the distal humerus is normal so long as it is not overly prominent (see Fig. 5.4).

FIGURE 5.37 Left elbow AP (A), lateral (B), and oblique (C) radiographs. Fracture of the radius neck. The patient fell from a bicycle and complained of a painful elbow. A fracture is not definitely visible on the AP and lateral radiographs; however, it should be strongly suspected because the anterior fat pad (single arrows) is more prominent than normal and a posterior fat pad (curved arrow) is present. The fracture (straight arrow) can be clearly visualized on the oblique radiograph. This demonstrates the importance of obtaining multiple views of a suspected fracture site and reiterates the significance of a positive posterior fat pad sign and a prominent anterior fat pad.
Occasionally, a severe fracture or other disease process of the proximal humerus necessitates a shoulder prosthesis (Fig. 5.43). Fractures of the scapula are not common and usually result from a high-force injury as in motor vehicle accidents (MVAs; Fig. 5.44). These are frequently evaluated by CT to determine whether the fracture involves the glenoid or the suprascapular notch where the nerve to the supraspinatus and infraspinatus muscle travels (Fig. 5.45). Fractures of the clavicle are very common, especially in children who fall (Fig. 5.46). The most common site for clavicle fractures is at the junction of the middle and distal thirds.
MRI is a powerful tool for evaluating shoulder rotator cuff integrity, and a complete interruption of the rotator cuff is shown in Fig. 5.47. An arthrogram is performed by distending a joint, usually with fluid that will provide contrast to the structures of interest. MR arthrograms are especially helpful for evaluating tears of the glenoid labrum (Fig. 5.48). Remember that MRI is excellent for demonstrating the bone marrow and soft tissue detail, whereas CT imaging is better for trabecular and cortical detail.
Sudeck’s atrophy, or reflex sympathetic dystrophy or chronic regional pain syndrome (Fig. 5.49), is a poorly understood phenomenon that can be the result of a fracture or almost any type of mild or severe injury. It is frequently associated with pain, swelling, and stiffness.
FIGURE 5.38 A: Left elbow AP radiograph. Avulsion fracture of the medial epicondyle epiphysis (straight arrow) in a 13-year-old. There is considerable soft tissue prominence (curved arrows), probably due to edema and hemorrhage secondary to the avulsion fracture. Remember that the pronators and flexors of the forearm attach to the medial epicondyle and the extensors and supinators to the lateral epicondyle. B: Right elbow AP radiograph for comparison. Normal. The medial epicondyle epiphysis (straight arrows) is normal. C: Right elbow oblique radiograph. Bucket-handle fracture of the distal humerus (curved arrow) in a 14-month-old child. Bucket-handle-type fractures can be found in child abuse situations. The straight arrows indicate periosteal reaction that occurs as a part of the healing process.

FIGURE 5.39 Left elbow (A) and right elbow (B) lateral radiographs. Anterior dislocation of the left (arrow). The right elbow lateral radiograph is normal and was obtained for comparative purposes as elbow anatomy may be especially difficult in children. Note the significant difference in position of the proximal left radius relative to the left humerus compared to the normal right proximal radius relative to the right humerus. Right elbow AP (C) and lateral (D) radiographs. Posterior dislocation of the elbow in a 23-year-old. The proximal ulna and the radial head are posterior to their normal articulations with the distal humerus, and this is best appreciated on the lateral view. There are no fractures. E: Left elbow lateral angiogram. Fracture-anterior dislocation of the left elbow in a different patient. The radius and ulna are dislocated anteriorly relative to the humerus, and there is a comminuted fracture of the ulna olecranon (straight arrows). The brachial artery is displaced anteriorly by the dislocation and the associated soft tissue edema and hemorrhage.
The etiologies of lower extremity injuries are similar to those in upper extremity injuries (see Table 5.9). Injuries to the feet are very common, as this is where our body meets the ground (see Figs. 5.50 to 5.55 for a gallery of common foot injuries). CT is often used to evaluate complex ankle and calcaneal fractures (Fig. 5.55). Remember that a lateral radiolucent line near the base of the fifth metatarsal that runs parallel to the long axis of the metatarsal in a growing person represents a normal apophysis (Fig. 5.51C), whereas a transverse lucent line at the base of the fifth metatarsal always represents a fracture (Fig. 5.51D). An apophysis is a growth center (like the epiphysis) that does not contribute to bone length. It alters bone contour and usually is not located in a joint but typically has tendons attached to it.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree