Type I: dysplastic
Congenital deformity of the posterior arch
Type II: isthmic
Lesions of the pars interarticularis with 3 subtypes
Type IIA. Lytic fatigue fracture of the pars
Type IIB. Elongated but intact pars
Type IIC. Acute fracture of the pars
Type III: degenerative
Due to long-standing intersegmental instability
Type IV: traumatic
Due to fractures in other areas of the bony hook than the pars
Type V: pathologic
There is generalized or local bone disease
Because of the high incidence of spondylolysis in child athletes with back pain, early imaging of the lumbar spine is important for diagnosis and treatment. Radiographs of the lumbar spine are useful primary tools in the diagnosis of spondylolysis. Four views of the lumbar spine, including anteroposterior, lateral, and bilateral oblique images, are recommended for the evaluation of suspected spondylolysis. Bilateral oblique images offer the best direct visualization of the pars interarticularis. In the oblique projection the posterior elements of the lumbar vertebrae mimic the profile of a Scottish terrier or “Scotty dog” (Fig. 27.1). Spondylolysis seen on oblique radiographs is likened to a collar or a break in the dog’s neck (Fig. 27.2). Approximately 20 % of pars defects are seen only on oblique radiographs. A coned lateral view centered at the lumbosacral junction can also increase sensitivity (Fig. 27.3). Lateral views of the lumbar spine are also useful to detect and grade associated spondylolisthesis. Radiographs are also sensitive to unilateral pars defects. In addition to direct visualization of the lesion, sclerosis of the contralateral pedicle can be seen as result of stress from a unilateral pars defect. This is often seen on the anterior view, in which the pedicles can be compared for symmetry (Fig. 27.4).

Fig. 27.1
Normal pars interarticularis. (a) Oblique radiograph of the lumbar spine shows normal posterior elements of L5. (b) The silhouette of the “Scotty dog.” The dog’s neck is the pars interarticularis
Fig. 27.2
Spondylolysis: (a) oblique radiograph of the lumbar spine shows spondylolysis of the pars interarticularis of L5 (arrows). (b) The broken neck of the “Scotty dog” silhouette

Fig. 27.3
Spondylolysis. Coned lateral radiograph of the lumbosacral junction shows spondylolysis of the pars interarticularis of L5 (arrow)
Fig. 27.4
A 15-year-old male football player with unilateral spondylolysis, presenting with low back pain. (a) Anteroposterior radiograph of the lumbar spine shows sclerosis of the pedicle of L5 on the right (arrow). (b) Sagittal-reformatted CT images confirm unilateral spondylolysis on the left (b, arrow) and stress reaction with sclerosis of the pars interarticularis and pedicle present on the contralateral side (c, arrow)
Spondylolysis may occur at any vertebral level but it is predominantly encountered in the lower lumbar spine. 85–95 % of pediatric lesions occur at L5. The L4 level accounts for 5–15 % of pediatric spondylolysis. Pars defects above L4 are rare. Spondylolysis can be unilateral or bilateral. Patients with unilateral spondylolysis subsequently may acquire a defect on the contralateral side due to mechanical stress (Fig. 27.5). Spondylolisthesis, forward displacement of the vertebral body on the level below, is more common when pars defects are bilateral (Fig. 27.6). The Meyerding classification is used to grade spondylolisthesis based on the severity of the translation (Table 27.2) (Meyerding 1931). Isthmic spondylolysis is considered to be secondary to mechanical stress on the lumbar posterior elements. In athletes, mechanical stress may occur due to repetitive microtrauma, acute shearing forces, acute loading forces, or a combination. Spondylolysis is found at an increased rate in a wide range of common youth sports including soccer, football, gymnastics, swimming, and diving (Stuart 2005; Caine and Nassar 2005; Giza and Micheli 2005; Nyska et al. 2000). Repetitive loading and repeated flexion and extension are implicated in most sports with higher rates of spondylolysis. The powerful kicking motion in soccer puts the lumbar spine rapidly through the full range of extension to hyperflexion while asymmetrically loading and rotating the lumbar vertebrae (El Rassi et al. 2005). Gymnastic training and competition places significant stress on the lower back. Positional stressors in gymnastics include hyperextension, hyperflexion, and hyperlordosis. Additionally, there is frequent significant axial loading when landing vaults, aerials, and dismounts. The incidence of spondylolysis in football players depends on the position played. The highest rates are seen among linemen, whose powerful blocking results in both extension and axial loading of the lumbar spine on nearly every down.



Fig. 27.5
Progressive spondylolysis. The patient presented in Fig. 27.4 had continued pain despite bracing and physical therapy. Sagittal-reformatted CT image shows new fracture of the left pars interarticularis (arrow)

Fig. 27.6
A 15-year-old male high jumper with spondylolisthesis, presenting with worsening back pain. Sagittal-reformatted CT image of the lumbar spine demonstrates that L5 has slipped anteriorly relative to S1. The slip measures between 50 and 75 % of the vertebral diameter (arrow). This corresponds to a Meyerding grade 3 spondylolisthesis
Table 27.2
The Meyerding classification of spondylolisthesis
Grade 1: 1–25 % anterior translation |
Grade 2: 26–50 % anterior translation |
Grade 3: 51–75 % anterior translation |
Grade 4: 76–100 % anterior translation |
Grade 5a: <100 % anterior translation |
In pediatric athletes with new symptoms suggesting spondylolysis and with normal radiographs, further imaging is indicated. Bone scan with single-photon emission (SPECT) and computed tomography (CT) have historically been the favored secondary imaging modalities. Both CT and bone scan have been shown to be sensitive in the detection of radiographically occult pars defects. CT best demonstrates bony detail and alignment, but does not provide physiologic information. Increased uptake in the pars, lamina, or pedicle on bone scan on SPECT images suggests symptomatic spondylolysis, stress reaction, or stress fracture (Fig. 27.7). SPECT is also used to guide treatment of radiographically diagnosed lesions (Bellah et al. 1991). Spondylolytic lesions with active uptake on nuclear imaging may respond better to conservative treatment such as activity restriction or bracing. Radiographic pars defects without uptake on scintigraphy are often asymptomatic. Any other etiology for the patient’s pain should be excluded in these cases (Fig. 27.8). CT and MRI are useful to exclude alternate pathologies such as infection or osteoid osteoma.
Fig. 27.7
An adolescent male football player with symptomatic spondylosis, presenting with back pain. (a) Posterior projection Tc-99m MDP scintigraphy of the lumbar spine shows abnormal uptake at L5 on the left (arrow). (b) Axial single-photon emission computed tomography (SPECT) slice more precisely shows the uptake in the pedicles and pars interarticularis of L5 on the left and less pronounced uptake on the right (arrows)
Fig. 27.8
A 17-year-old female diver who had sharp posterior low back pain while executing a reverse dive. (a) Lateral radiograph of the lumbar spine shows spondylolysis at L5 (arrow). (b) Posterior projection Tc99m-MDP scintigraphy of the lumbar spine shows no abnormal activity in the region of the pars defects. There is abnormal uptake at the tip of the L4 spinous process (arrow). Subsequently the L4 spinous process was found to be tender to direct palpation and she was diagnosed with “kissing spine” syndrome, impingement of the spinous processes in extreme hyperextension
MRI has developed into a valuable tool in the diagnosis and workup of spondylolysis. MRI, although less sensitive in the detection of pars lesions, is improving in its ability to detect complete pars defects. It is also useful to detect edema early in the course of stress lesions, both in the pars, as well as the adjacent lamina and pedicles (Fig. 27.9). Although increased T2 signal is only an indirect indication of reparative change as compared to increased tracer uptake on bone scan, MRI may be useful in detecting early lesions that respond better to therapy (Sairyo et al. 2006). The lack of ionizing radiation in MRI is another distinct advantage over both CT and bone scan/SPECT.
Fig. 27.9
A 16-year-old male soccer player with spondylolysis, presenting with back pain. (a) Sagittal T1-weighted MRI of the lumbar spine demonstrates spondylolysis of L5 on the right (arrow). (b) Sagittal fat-suppressed T2-weighted MRI shows abnormal high signal in the left pars interarticularis, lamina, and pedicle, consistent with stress reaction (arrows)
27.2.1.2 Disk Herniation
Acute disk herniation is significantly less common in young athletes than in adults. The clinical presentation is often less clear in children. Sciatica, a frequent presenting complaint in adults, is rare in pediatric disk pathology. Unique to the adolescent spine is intervertebral disk herniation associated with avulsion fracture of the apophyseal ring (Fig. 27.10) (Peh et al. 1998). The apophyseal ring begins to ossify around 5 years of age and completely fuses with the vertebral body between 18 and 20 years of age. The apophyseal ring is attached to the adjacent annulus fibrosis by Sharpey’s fibers. This attachment is much stronger than the fibrocartilage junction with the vertebral body ossification center. The ossified portion of the apophyseal ring is also strongly attached to the posterior longitudinal ligament. When acute or chronic stress injures the apophyseal cartilage, the ossified fragment remains attached to the annulus and posterior longitudinal ligament. Unlike the adult athlete population, where degenerative changes to the annulus are usually seen in disk disease, adolescent disk protrusion is more often secondary to destabilization of the annulus by apophyseal injury (Fig. 27.11).
Fig. 27.10
A 17-year-old male football player with apophyseal ring separation, presenting with chronic low back pain. (a) Lateral radiograph of the lumbar spine shows bilateral spondylolysis of L5 with grade 1 spondylolisthesis of L5 on S1. Additionally, there is contour deformity of the posterior aspect of the inferior endplate of L5. (b) Sagittal fat-suppressed T2-weighted MRI shows associated posterior ring apophyseal separation at the lower endplate of L5 (white arrow) with L5–S1 disk herniation (black arrow)
Fig. 27.11
Apophyseal ring injury. (a) Sagittal-reformatted CT image of the cervical spine shows a bulging C5–C6 disk and posterior displacement of a fragment of the posterior apophyseal ring (arrow). (b) Sagittal fat-suppressed T2-weighted MRI shows fluid (arrow) between the vertebral body and the elevated posterior longitudinal ligament
27.2.2 Stress Fractures in Pediatric Athletes
Stress fractures were uncommon in youth athletes before the time when repetitive training for sports became widespread; nowadays they are common (Coady and Micheli 1997; Ecklund 2002). The classic description of how a fatigue stress fracture occurs is outlined above. In addition to this concept of increasing forces overwhelming the remodeling process, muscle fatigue in the face of increasing exercise loads may contribute to the formation of stress fractures by altering movement patterns. This process changes the typical distribution of stress and concentrates it at focal sites that are not prepared to withstand the load (Coady and Micheli 1997). As in adults, about half of stress fractures in pediatric patients occur in the tibia, whereas the fibula (20 %) and pars interarticularis of the lumbar spine (15 %) comprise the majority of the remaining cases in pediatric athletes, with the femur (3 %), metatarsals (2 %), and tarsal navicular (2 %) accounting for relatively few cases (Coady and Micheli 1997).
27.2.2.1 Grading Stress Fractures and Stress Reactions
Radiographs are the first radiologic study undertaken when stress fracture is suspected. When positive, radiographs demonstrate focal periosteal reaction and occasionally endosteal cortical thickening and/or a lucent fracture line in the cortex. However, only about 10 % of radiographs are positive initially, as findings take from 2 to 12 weeks to manifest (Coady and Micheli 1997). MRI has become the imaging method of choice to confirm or exclude stress fractures when radiographs are negative (Heyworth and Green 2008). MRI is more precise than bone scintigraphy and allows discrimination of stress fractures from other bone insults, such as osteoid osteoma, osteomyelitis, neoplasm, and ligamentous injury with secondary osseous reaction (Coady and Micheli 1997). Fredericson and colleagues developed an MRI grading system for tibial stress fractures that has been clinically validated (Fredericson et al. 1995). Grade 1 stress injuries exhibit high T2 signal along the periosteum of the tibia with no signal abnormality present within the bone marrow (Fig. 27.12). Grade 2 injuries add abnormal high T2 marrow signal to the findings, but have no abnormal T1 signal in the marrow (Fig. 27.13). In grade 3 injuries, abnormal low T1 signal is also seen within the marrow (Fig. 27.14). Finally, grade 4 injuries include all these findings but add abnormal signal within the cortex, typically a fracture line but sometimes a broader, less linear area of abnormal signal (Fig. 27.15). In common parlance, injuries of grades 1–3 are referred to as “stress responses” or “stress reactions” and grade 4 injuries are considered “stress fractures.” Increasing grade of stress injury in the tibia reflects increasing severity of injury and often directs the level of restriction of activity recommended to the athlete. Kijowski and colleagues (2007) evaluated the radiographs of 86 patients with MRI scans demonstrating tibial stress injuries. The radiographs with periosteal reaction that corresponded to the patient’s maximal point of pain correlated with high-grade stress injuries, usually grade 4 (stress fracture). This finding may obviate MRI when radiographs of the tibia are positive, as the patient can be treated for stress fracture with confidence, unlike a low-grade stress response.
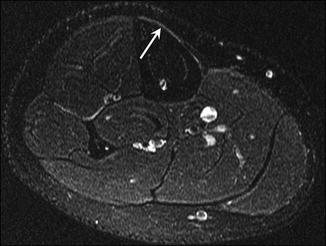
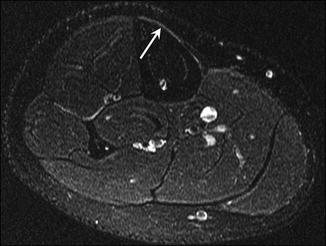
Fig. 27.12
A 15-year-old male runner with grade 1 tibial stress response. Axial fat-suppressed T2-weighted MRI of the right tibia shows mildly increased signal in the periosteum in the area of the patient’s pain (arrow)
Fig. 27.13
A 15-year-old female cross-country runner with grade 2 tibial stress response. (a) Axial fat-suppressed T2-weighted MRI of the right tibia demonstrates increased signal in the periosteum (arrow), as well as increased signal in the marrow space (arrowhead). (b) Axial T1-weighted MRI at the same level shows no abnormal marrow signal
Fig. 27.14
A 14-year-old female cross-country runner with grade 3 tibial stress response. (a) Axial fat-suppressed T2-weighted MRI of the right tibia demonstrates increased signal in the periosteum (arrowhead) and marrow (arrow). (b) Axial T1-weighted MRI at the same level shows abnormal low signal in the marrow (arrow)
Fig. 27.15
A 17-year-old female distance runner with tibial stress fracture (Fredericson grade 4). (a) Axial fat-suppressed T2-weighted MRI of the right tibia demonstrates extensive increased signal in the periosteum (arrowheads) and marrow (arrow). The periosteum is slightly elevated and there is increased signal in the cortex (arrow). (b) Axial T1-weighted MRI at the same level shows abnormal low signal in the marrow and cortex (arrow)
27.2.2.2 Stress Fractures of the Upper Extremity
Stress fractures are rare in the upper extremity of pediatric athletes. Stress fractures occasionally occur in the proximal humerus as overuse injuries in throwing athletes, including baseball pitchers and javelin throwers, and those involved in rugby, swimming, and racquetball (Caviglia et al. 2005). These injuries can be imaged with MRI, bone scan, or CT and usually heal with conservative treatment (Caviglia et al. 2005). Similarly, stress osteolysis of the distal clavicle is rare in adolescents but can occur in adolescent weight lifters. When present, this entity decreases mineralization of the distal clavicle and causes resorption of its distal tip (Fig. 27.16) (Gomez 2002).


Fig. 27.16
A 17-year-old football player with stress osteolysis of the clavicle, complaining of pain with bench presses and push-ups. Anteroposterior radiograph of the shoulder shows irregularity and erosion of the distal clavicle (arrow)
Wrist impaction stress injuries are common in female pediatric gymnasts. “Gymnast wrist” is thought to be caused by chronic compressive impact forces and can reflect several different specific injuries, including overuse injuries of the distal radial physis, tears of the triangular fibrocartilage or rarely the scapholunate or lunotriquetral ligaments, cartilage damage along the articular surfaces of the distal radius and carpal bones, and dorsal ganglion cysts of the wrist (Mandelbaum et al. 1989). Most commonly, gymnast wrist refers to injury of the growth plate of the distal physis (Auringer and Anthony 1999). These injuries often have chronic sequelae into adulthood. The physis of the distal radius suffers marked compressive loading during gymnastics routines, especially with the wrist dorsiflexed, applying compression and shearing forces across the physis. As with the injuries of the proximal humeral and medial epicondyle physes, this injury is understood as a chronic stress injury of the physis, basically a nondisplaced Salter-Harris I stress fracture (Carter et al. 1988). This injury also occurs in weight lifters and roller skaters (Carter et al. 1988). Radiographic changes may include asymmetric widening, haziness, and irregularity of the physis, with variable sclerosis and cystic changes on the metaphyseal side (Fig. 27.17) (Carter et al. 1988; Roy et al. 1985). In some patients with the classic clinical findings of gymnast wrist (namely, wrist pain in the setting of gymnastics), radiographs appear normal. In one study, patients with normal radiographic results were able to return to gymnastics and were pain-free after resting for only a few weeks, whereas those with radiographic findings required an average of 3 months of inactivity to heal (Roy et al. 1985).


Fig. 27.17
A 13-year-old female gymnast with chronic wrist pain. Posteroanterior radiograph of the left wrist demonstrates sclerosis, irregularity, and widening of the physis of the distal radius, representing “gymnast wrist”
Patients who have substantial cumulative injury to the distal radial physis may undergo premature closure of the physis and exhibit a relatively short radius (Fig. 27.18). These patients will have positive ulnar variance and may sustain the various components of ulnar impaction syndrome in their late teenage years and adulthood. This syndrome includes fraying or tearing of the triangular fibrocartilage; damage of the articular cartilage of the lunate, distal radius, and/or triquetrum; and ultimately, tears of the lunotriquetral ligament and degenerative arthrosis of the involved bones in the end stages (Zetaruk 2000). However, full-blown ulnar impaction syndrome with all the components is rare in adolescents. The main component of this syndrome seen in adolescents, other than the positive ulnar variance, is injury to the triangular fibrocartilage (Fig. 27.19) (Zetaruk 2000), which has also been reported in adolescent basketball players with positive ulnar variance (Gaca 2009).

Fig. 27.18
A 13-year-old female gymnast with ulnar impaction syndrome. (a) Posteroanterior radiograph of the left wrist shows premature closure of the distal radial physis and positive ulnar variance. (b) Posteroanterior radiograph of the asymptomatic right wrist for comparison shows a normal radial physis and normal radioulnar relationship. (c) Coronal fat-suppressed T2-weighted MRI of the left wrist shows increased signal in the proximal lunate (arrow)

Fig. 27.19
A 16-year-old weightlifter with triangular fibrocartilage tear, complaining of wrist pain on extension. Coronal T1-weighted MR arthrogram image of the wrist demonstrates a large central tear of the triangular fibrocartilage (arrow). Contrast enters the distal radioulnar joint confirming a tear (arrowhead)
In 1966, Adams reported five cases of Little Leaguer’s shoulder, all in adolescent male baseball pitchers (Adams 1966). Adams referred to this malady as osteochondrosis, but it is now thought of as a stress injury to the proximal humeral physis. This overuse injury is probably best considered a chronic stress form of a nondisplaced Salter-Harris I fracture and occurs in throwers aged 11–16 years, especially baseball pitchers (Lord and Winell 2004; Gomez 2002). This fracture is thought to result from rotational forces placed on the proximal humeral physis by repetitive pitching (specifically too many pitches per week over many weeks), especially curveballs, and other high-volume throwing activities. Patients describe pain particularly in the follow-through stage of the pitching motion (Saperstein and Nicholas 1996). Recent weight gain and out-of season throwing are also risk factors for this injury (Lord and Winell 2004; Latz 2006; Emery 2009). This fracture is an excellent example of the advantages of cross-training (switching sports in different seasons) to pediatric athletes. Switching to a sport that does not place similar stresses on the throwing arm would allow the physis to recover normally and reduce the risk of chronic injury.
Radiographs of patients with Little Leaguer’s shoulder may be normal. When positive for the injury, radiographs demonstrate the physis to be widened (Fig. 27.20), often with accompanying demineralization, fragmentation, cystic change, or sclerosis (Lord and Winell 2004; Emery 2009; Adams 1966). Because the changes may be subtle, the radiographs should be compared with those of the patient’s asymptomatic non-throwing shoulder if there is any uncertainty (Latz 2006). MRI is not typically performed for this injury, but when performed, it shows widening of the physis, in addition to the increased T2 signal intensity within the physis and occasionally edema in the subchondral bone adjacent to the physis. If the patient is treated appropriately with rest to the throwing arm, Little Leaguer’s shoulder is self-limited and resolves rapidly (Adams 1966); appropriate treatment is important, because the proximal humeral physis is responsible for much of the length of the growing humerus (Gomez 2002).
Fig. 27.20
A 12-year-old left-handed baseball pitcher with Little Leaguer’s shoulder. (a) Grashey radiograph of the left shoulder reveals widening and irregularity of the proximal humeral physis. (b) Grashey radiograph of the normal right shoulder is shown for comparison
27.2.2.3 Stress Fractures and Stress Responses in the Lower Extremities
Most tibial stress fractures are focal injuries that occur in the proximal third of the bone, typically along the posterior medial side. The injury clinically referred to as “shin splints” is a longer segment injury, purportedly an enthesopathy that encompasses up to half the length of the bone (Carty 1998). Shin splints only exhibit periosteal signal abnormality on MRI and no abnormal signal within the marrow space (Fig. 27.21). As such, this is a form of Fredericson grade 1 stress response (Fredericson et al. 1995). Although less frequently used due to the rise of MRI, 3 phase bone scan was used previously because it was more sensitive than radiography. Shin splints present as linear increased uptake along the posterior medial tibia (Fig. 27.22).
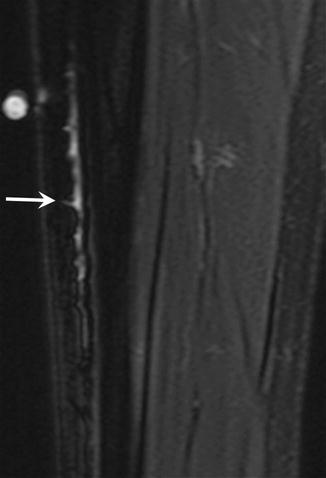
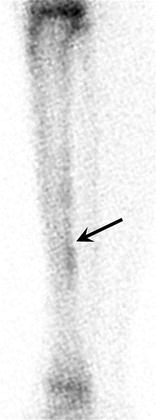
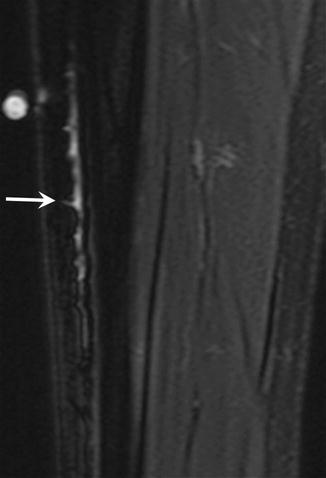
Fig. 27.21
A 16-year-old female track athlete with shin splints. Oblique coronal fat-suppressed T2-weighted MRI of the tibia shows increased signal in the periosteum of the medial tibia (arrow). This is a Fredericson grade 1 tibial stress reaction, also known as shin splints
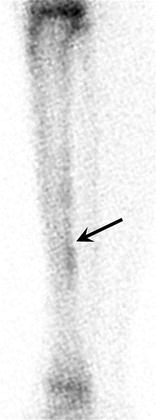
Fig. 27.22
Shin splints. Technetium 99-m MDP scintigraphy of the left tibia demonstrates mild periosteal uptake along the posterior cortex of the tibia (arrow). This corresponds to a Fredericson grade 1 tibial stress reaction on MRI
An important, albeit rare, type of tibial stress fracture occurs in the anterior cortex of the middle third of the bone. This anterior tibial stress fracture occurs in teenagers and young adults involved in sports involving frequent leaping, especially basketball (Beals and Cook 1991; Rettig et al. 1988). On radiographs these injuries are all visible, exhibiting a definite transverse lucent line through the anterior cortex and considerable cortical hypertrophy around the line (Fig. 27.23) (Beals and Cook 1991). The importance of recognizing this type of stress fracture lies in its clinical course. Unlike other stress reactions, these anterior mid-tibial stress fractures are unlikely to heal with short-term immobilization. Longer periods of inactivity are usually required and they often require surgical excision and bone grafting to heal (Beals and Cook 1991; Green et al. 1985). Before the importance of these injuries was understood, it was common for them to progress to complete fractures on resuming practice following a period of immobilization or rest (Beals and Cook 1991; Green et al. 1985). These stress fractures are considered delayed union stress fractures (Rettig et al. 1988) and the resistance to healing despite conservative treatment is thought to relate to the fact that the anterior cortex of the tibia is under tension, whereas the posterior proximal or distal cortex, which is where most tibial stress fractures occur, is under compression (Rettig et al. 1988; Green et al. 1985).
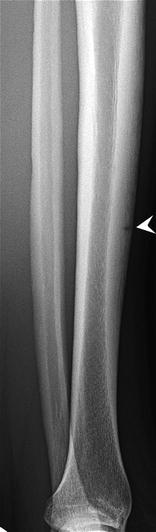
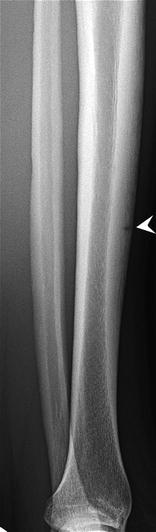
Fig. 27.23
A cheerleader with anterior mid-tibial stress fracture, presenting with shin pain. Lateral radiograph of the left tibia shows a radiolucent fracture line at the point of maximal pain (arrowhead)
Fibular stress fractures are also relatively common in pediatric athletes (Fig. 27.24). Stress injury in the fibula most commonly occurs in the distal third of the bone (Woods et al. 2008). Cortical signal abnormality is present in most cases, either linear or more commonly globular (Woods et al. 2008). Foot and ankle stress fractures usually occur in dancers and distance runners, especially within the metatarsals, and sesamoid stress fractures have been reported in runners, ballet dancers, and soccer and field hockey players (Fig. 27.25) (Coady and Micheli 1997). Freiberg infraction typically occurs in the second or third metatarsal head of 12–15-year-old athletic girls and is related to repetitive stress. Freiberg infraction is considered to be either a stress fracture or stress-induced osteonecrosis and results in flattening and sclerosis of the metatarsal head and occasional fragmentation (Fig. 27.26) (Pommering et al. 2005; Vanhoenacker et al. 2002). Stress fractures of the tarsal navicular are rare in this age group but are ominous as they are prone to nonunion (Fig. 27.27) (Bernhardt and Landry 1995).


Fig. 27.24
A 16-year-old female soccer player with fibular stress fracture, presenting with 3-week history of pain. (a) Axial T1- and (b) coronal fat-suppressed T2-weighted MRI show abnormal signal in the thickened periosteum, cortex, and marrow (arrow)

Fig. 27.25
A 17-year-old female cross-country runner with metatarsal stress fracture. Long-axis fat-suppressed T2-weighted MRI of the left foot reveals abnormal increased signal in the second metatarsal base and shaft (arrow)

Fig. 27.26
A 12-year-old female basketball player with Freiberg infraction, presenting with mid foot pain. Anteroposterior radiograph of the right foot demonstrates sclerosis, fragmentation, and collapse of the distal articular surface of the second metatarsal (arrow)
Fig. 27.27
A 15-year-old male basketball player with navicular stress fracture, presenting with chronic foot pain. (a) Long-axis T1- and (b) fat-suppressed T2-weighted MRI of the left foot show abnormal signal in the navicular (arrow) as well as the lateral cuneiform (arrowhead)
Femoral neck stress fractures, relatively common in adults, are rare in most reports on pediatric stress fractures. However, they do occur (Meaney and Carty 1992) and in one report comprised 5 of 53 stress fractures occurring in pediatric athletes (Fig. 27.28) (Micheli 1983). As described earlier, the Fredericson grading system for stress injuries has been clinically validated for the tibia, for which it was developed. It is frequently used when describing stress changes elsewhere in the skeletal system, but has not been similarly validated in these other settings. One should be cautious when applying this system to other bones, since the pathophysiology in other bones will not necessarily be analogous to the tibia. Because of differences in mechanics and load bearing, the clinical relevance of specific findings in the tibia may not directly translate to treatment regimens for other bones. For this reason, when observing any signs of stress injury to bones other than the tibia, it is recommended that one specifies them as “stress fractures” and delineates the specific findings, allowing the sports medicine physician to tailor the appropriate treatment. One must be especially cautious about labeling a stress injury of the femoral neck anything but a stress fracture, because a femoral neck stress fracture that is not appropriately treated and progresses on to complete fracture is a catastrophe.
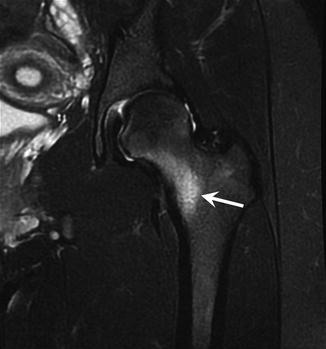
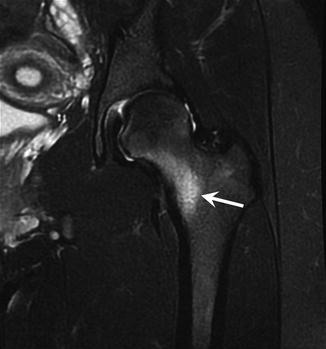
Fig. 27.28
A 16-year-old female runner with femoral neck stress fracture, presenting with 2-month history of groin pain. Coronal fat-suppressed T2-weighted MRI of the left hip reveals abnormal signal in the inferomedial femoral neck (arrow)
27.2.3 Traction Apophysitis
Although significantly less common than tendinitis in the clinical setting (one report of 724 overuse showed an 80 % incidence of tendinitis and only a 19 % incidence of apophysitis) (Micheli and Fehlandt 1992), traction apophysitis is not uncommon in the setting of overuse in adolescents. Apophysitis is a diagnosis that is unique to the growing skeleton. Epiphyses occur at the ends of long and short tubular bones and add to the overall length of the bone as their physes continue to produce new bone until skeletal maturity is reached. On the other hand, apophyses are growth centers that serve as attachment sites for tendons and are often referred to as secondary growth centers (Ryu and Fan 1998). Apophyses also have physes at their interface with the rest of the bone, and just as the epiphyseal physis can be a weak link in a long bone, often suffering a Salter-Harris fracture, the apophyseal physis is a weak link also. When the tendon force exceeds maximal load, the apophyses may separate and become displaced, an avulsion fracture. However, when chronic submaximal repeated forces are placed by a tendon on an apophysis, an overuse injury known as traction apophysitis may result. This injury is especially common during phases of rapid growth, whereas tendinitis is more likely to result from the same forces in a patient who is in a slow growth stage (Micheli and Fehlandt 1992; Saperstein and Nicholas 1996). Pathologically, traction apophysitis represents an accumulation of microscopic avulsions along the apophyseal physis with secondary inflammatory changes attempting to repair the damage but being overwhelmed by the unremitting chronic stresses (Micheli and Fehlandt 1992; Auringer and Anthony 1999). Traction apophysitis essentially is a stress fracture of the apophyseal physis, analogous to a nondisplaced Salter-Harris I injury. These injuries result in tenderness and swelling, with accompanied pain during motion (Ryu and Fan 1998). Specific apophyses that commonly undergo traction apophysitis are addressed in the joint-based discussions that follow.
27.2.3.1 Traction Apophysitis of the Elbow and Little Leaguer’s Elbow
The discussion of elbow injuries in pediatric athletes, especially those who are skeletally immature, centers on a set of maladies grouped under the rubric Little Leaguer’s elbow. About 20 % of pitchers aged 10–14 years have experienced elbow pain (DaSilva et al. 1998). Little Leaguer’s elbow is an overuse phenomenon resulting from chronic repetitive valgus stresses placed on the elbow by the throwing motion, typically seen in pitchers and quarterbacks who throw more than 200 times per week (Do and Herrera-Soto 2003). This valgus stress occurs during the cocking and acceleration phase of the throwing motion and places tension on the medial side of the elbow and compression on its lateral side (Gomez 2002; Ryu and Fan 1998). These forces, when repeated often enough, may result in several specific pathologic entities, including traction apophysitis of the medial epicondyle, osteochondritis dissecans of the capitellum, loose intra-articular fragments, traction apophysitis of the olecranon, premature closure of the radial physis, and/or overgrowth of the radial head (Lord and Winell 2004; Micheli 1983). Traction apophysitis describes a condition of irritation and breakdown of the apophyseal physis (Saperstein and Nicholas 1996). Apophyseal physes are most vulnerable in the growing elbow because they are weaker than the bone and the muscle-tendon unit. Certainly, apophyses that are subjected to abrupt extreme forces may displace from the underlying bone, termed an avulsion fracture; however, if the tendon repeatedly subjects the apophysis to chronic submaximal forces, the physis may develop chronic traction apophysitis.
Traction apophysitis of the medial epicondyle is one of the most frequent components of Little Leaguer’s elbow (Saperstein and Nicholas 1996). The medial epicondyle is the origin of the flexor pronator tendon group, which places tension on the medial epicondyle when strong valgus forces are in effect. This condition afflicts not only preadolescent and adolescent pitchers who engage in heavy throwing regimens but also tennis players and javelin throwers (Gomez 2002; Stanitski 1997). Radiographs demonstrate variable irregularity of ossification, fragmentation, and sclerosis of the apophysis as well as widening and indistinctness of the physis (Fig. 27.29) (Saperstein and Nicholas 1996; Auringer and Anthony 1999; Bernhardt and Landry 1995). MRI demonstrates widening of the physis and increased T2 signal intensity within and possibly adjacent to the physis. The apophysis may be segmented and partially resorbed (Sugimoto and Ohsawa 1994).


Fig. 27.29
A 14-year-old male baseball pitcher and football quarterback with traction apophysitis of the medial epicondyle. Anteroposterior radiograph of the right elbow demonstrates widening and irregularity of the physis of the medial epicondyle (arrow)
Traction apophysitis in the elbow is not limited to the medial epicondyle ossification center. This overuse injury can also affect the olecranon apophysis, though less commonly. Occasionally mentioned as a component of Little Leaguer’s elbow, traction apophysitis of the olecranon more commonly afflicts high-level gymnasts (Maffulli et al. 1992). Football players, competitive divers, and hockey players have also been diagnosed with olecranon apophysitis (Do and Herrera-Soto 2003; Maffulli and Baxter-Jones 1995). Radiographic findings are analogous to those at the medial epicondyle, with variable degrees of physeal widening and apophyseal indistinctness and fragmentation (Maffulli et al. 1992). Caution must be applied in interpreting the lateral radiograph in children because in young children the normal physis may measure up to 5 mm; by the age of 12 years, though, the physis should be narrow, with serpiginous but congruent apposing borders (Chan et al. 1991). Stress fractures are known to occur in the olecranon after physeal closure (Maffulli et al. 1992) but may even occur within the olecranon ossification center before skeletal maturity in baseball pitchers, wrestlers, and gymnasts. When this fracture occurs, radiographs reveal fragmentation and sclerosis of the apophysis and widening of the physis (Maffulli and Baxter-Jones 1995; Chan et al. 1991; DaSilva et al. 1998); undoubtedly, there must be a clinical and radiographic overlap between stress fractures of the apophysis and stress injuries of the physis itself.
27.2.3.2 Traction Apophysitis in Hips and Pelvis
One of the causes of a chronically painful hip in pediatric athletes is traction apophysitis. Pelvic apophysitis results in dull, activity-related pain near the hip. Apophysitis in the hip and pelvis is described in runners, dancers, and in hockey, lacrosse, and football players (Frank et al. 2007). Any of the pelvic apophyses may be involved by traction apophysitis. Acute avulsions are commonly seen in the anterior inferior iliac spine and anterior superior iliac spine but traction apophysitis can also occur at both locations (Fig. 27.30). Traction apophysitis also occurs at the iliac crest, often in runners (Fig. 27.31), and the ischial tuberosity (Fig. 27.32) (Auringer and Anthony 1999; Hotchkiss et al. 2007). On radiographs, the physis may have a normal appearance or appear mildly widened, but not displaced (Frank et al. 2007). At the ischial tuberosity, the apophysis may not be ossified yet, in which case traction apophysitis will cause the margins of the bone to appear irregular and sclerotic, with lucent defects (Kozlowski et al. 1989). MRI of traction apophysitis in the pelvis reveals abnormally increased T2 signal in the bone and sometimes the attached tendon. Ultrasound demonstrates soft tissue thickening about the enthesis and thickening and increased echogenicity of the tendon at the attachment site (Carty 1998).
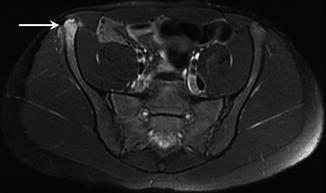

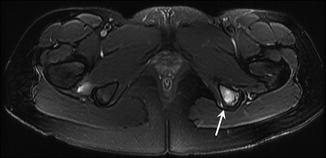
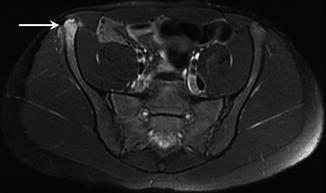
Fig. 27.30
A 14-year-old figure skater with traction apophysitis of the anterior superior iliac spine. Axial fat-suppressed T2-weighted MRI of the pelvis demonstrates abnormal signal in the anterior superior iliac spine and adjacent sartorius and gluteus medius (arrow)

Fig. 27.31
A 14-year-old female cross-country runner with traction apophysitis of the iliac crest. Anteroposterior radiograph of the pelvis shows widening, sclerosis, and irregularity of the right iliac crest apophyseal growth plate (arrow)
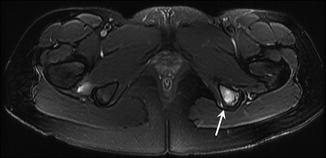
Fig. 27.32
A 15-year-old female distance runner with ischial apophysitis, presenting with left hip pain. Axial fat-suppressed T2-weighted MRI of the pelvis reveals abnormal signal in the left ischium and ischial apophysis (arrow)
Another overuse injury of the pelvis, osteitis pubis, does not occur in young children but is seen in late adolescent runners, fencers, and soccer, hockey, and football players (Hotchkiss et al. 2007; Waite and Krabak 2008). The concepts regarding etiology of osteitis pubis and the broader topic of athletic pubalgia continue to evolve, but osteitis pubis is clearly a chronic overuse injury and likely results from stress related to shear forces from unbalanced traction on the pubic symphysis (Waite and Krabak 2008; Paletta and Andrish 1995). Osteitis pubis results in a gradual onset of pubic pain related to activity. Radiographs reveal sclerosis and rarefaction of the subchondral bone at the pubic symphysis, as well as erosions and cystic changes (Fig. 27.33). However, it can be difficult to discriminate these abnormalities from normal irregularity and fragmentation at the symphysis in the skeletally immature patient (Hotchkiss et al. 2007; Waite and Krabak 2008). MRI demonstrates T2 signal abnormality in the subchondral bone (Fig. 27.34).

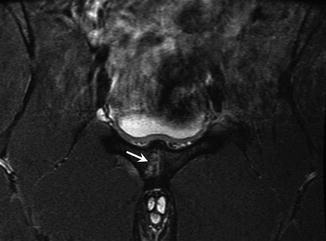

Fig. 27.33
A 17-year-old male football player with osteitis pubis, presenting with week history of groin pain. Anteroposterior radiograph of the pelvis reveals sclerosis, irregularity, and cystic changes along the pubis symphysis (arrow)
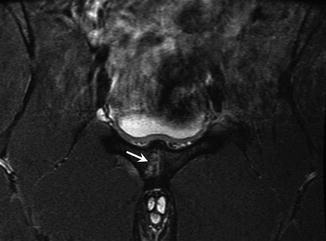
Fig. 27.34
A 17-year-old male basketball player with osteitis pubis, presenting with right groin pain while running. Oblique coronal STIR MRI of the pelvis reveals abnormal signal and cystic changes in the right pubis (arrow)
27.2.3.3 Traction Apophysitis in the Knee
Anterior knee pain is the most common complaint in the adolescent and preadolescent athlete (Ryu and Fan 1998), and many of these complaints stem from the extensor mechanism. Osgood-Schlatter disease is one of the common causes of anterior knee pain in this age group. Most common in 12–15-year-old boys and 8–12-year-old girls, Osgood-Schlatter is a traction apophysitis related to strong forces from the quadriceps mechanism. It occurs at the insertion of the patellar tendon on the tibial tuberosity (Gholve et al. 2007). Repeated jumping, squatting, and/or kneeling leads to Osgood-Schlatter, which produces local pain, swelling, and tenderness at the tuberosity (Gholve et al. 2007). Radiographs reveal irregularity of the apophysis, occasional widening of the physis, and separate bone fragments within the distal tendon near its insertion (Fig. 27.35). Thickening of the tendon will also be present (Gholve et al. 2007; Rosenberg et al. 1992). Bone fragments within the tendon are present in 50 % of cases (Stanitski 1993). On MRI, there is abnormal high signal within and surrounding the tendon on T2-weighted images, and deep infrapatellar bursitis is often present (Auringer and Anthony 1999; Rosenberg et al. 1992). On ultrasound, the tendon will be thickened and heterogeneous and may exhibit echogenic bone fragments and increased vascularity (Fig. 27.36). This malady is considered self-limited, but even with a reduction in athletic activities, symptoms may take months or years to resolve (typically at skeletal maturity), if they ever do (Gholve et al. 2007; Davids 1996).


Fig. 27.35
A 12-year-old male football player with Osgood-Schlatter disease. Lateral radiograph of the right knee shows thickening of the insertion of the patellar tendon, fragmentation of the tibial tubercle apophysis (arrowhead), and edema in the surrounding soft tissues and Hoffa fat pad (arrow)
Fig. 27.36
A 17-year-old male snowboarder with Osgood-Schlatter disease. (a) Longitudinal ultrasound image comparing the insertions of the symptomatic left and normal right patellar tendons shows thickening of the insertion of the left patellar tendon with bony fragments in the distal tendon (arrows in the left image). (b) Doppler ultrasound image of the left knee shows increased vascularity in the distal patellar tendon (arrow)
Sinding-Larsen-Johansson disease is a similar traction apophysitis that affects the origin of the patellar tendon at the inferior pole of the patella in a slightly younger age group (Bernhardt and Landry 1995; Lyon and Street 1998). Technically not an apophysis, the inferior pole of the patella reacts just like the tibial tubercle when subjected to chronic traction forces by the extensor mechanism, so Sinding-Larsen- Johansson is considered a traction apophysitis (Wojtys 1987). The radiographic and MRI findings of Sinding-Larsen-Johansson are identical to those of Osgood-Schlatter, except that they occur at the origin of the patellar tendon (Fig. 27.37) (Auringer and Anthony 1999). For both Osgood-Schlatter and Sinding-Larsen- Johansson, ossicles within the tendon are not enough to make the diagnosis; there must be soft tissue swelling of the tendon, as bone fragments occasionally may occur at the entheses of the tendon as a normal variant (Gaca 2009). The situation changes in skeletally mature adolescents, because similar chronic traction phenomena at the inferior pole of the patella result in jumper’s knee, which is chronic patellar tendinitis (Bernhardt and Landry 1995; Stanitski 1993). MRI findings include thickening and high T2 signal in and around the tendon (Fig. 27.38). Partial tears should be sought, as they may change treatment. On ultrasound, the normal fibrillar echo pattern of the patellar tendon becomes heterogeneous. The tendon will be swollen and may exhibit partial tears (Roberts et al. 2002).
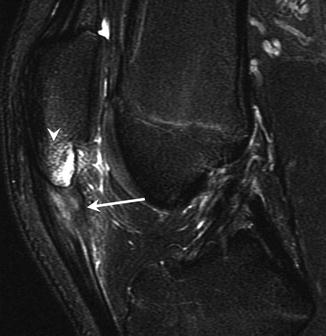
Fig. 27.37
A 10-year-old soccer player with Sinding-Larsen-Johansson disease, 4-week history of pain. (a) Later radiograph of the left knee shows sclerosis and irregularity of the origin of the patellar tendon and inferior pole of the patella (arrow). (b) Sagittal fat-suppressed T2-weighted MRI of the left knee shows abnormal increased signal in the proximal patellar tendon, distal patella, and adjacent fat pads
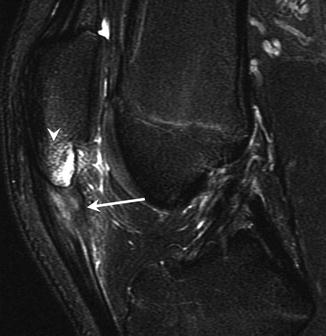
Fig. 27.38
A 16-year-old basketball player with jumper’s knee. Sagittal fat-suppressed T2-weighted MRI of the left knee demonstrates thickening and abnormal increased signal and in the proximal patellar tendon (arrow), as well as increased signal in the distal pole of the patella and adjacent fat pads (arrowhead). Note the difference in skeletal maturity compared to Fig. 27.37
27.2.3.4 Traction Apophysitis in the Ankle and Foot
There is some overlap of true traction apophysitis entities in the foot and ankle with cases of osteochondrosis, which is a term for disordered endochondral ossification that becomes symptomatic. Sever disease is a common overuse traction apophysitis at the calcaneal tuberosity (Pommering et al. 2005) that causes exquisite tenderness at the attachment of the Achilles to the apophysis (Stanitski 1997). This apophysitis usually occurs in 10- to 13-year-olds with tight Achilles tendons and plantar fasciae who have undergone recent growth spurts and concurrent increases in activity (Pontell et al. 2006; Saperstein and Nicholas 1996). Sever disease may lead to fragmentation and sclerosis of the apophysis and widening of the physis (Fig. 27.39), but these findings are often present to a similar degree in asymptomatic preadolescents (Pommering et al. 2005). As such, there are no reliable radiographic signs of Sever disease, and this diagnosis is a purely clinical one. Even MRI often demonstrates moderate high T2 signal in the calcaneal apophysis in asymptomatic youths, so MRI also is not diagnostic (Vallejo and Jaramillo 2001). Iselin disease is a similar traction apophysitis that occurs at the attachment of the peroneus brevis tendon onto the fifth metatarsal base apophysis in runners (Pontell et al. 2006). Radiographs are typically normal (Bernhardt and Landry 1995) but may demonstrate enlargement or fragmentation of the apophysis and widening of the physis (Canale and Williams 1992).


Fig. 27.39
A 10-year-old male soccer player with Sever disease, complaining of heel pain. Lateral radiograph of the right calcaneus shows the calcaneal apophysis is sclerotic and fragmented with thickening of the insertion of the Achilles tendon (arrow)
27.2.4 Articular Cartilage Injuries
Another common overuse condition of the pediatric athlete is osteochondritis dissecans (OCD). OCD is an idiopathic acquired pathologic condition that results in delamination and sequestration of a fragment of subchondral bone at the articular surface with its overlying cartilage (Kocher et al. 2006; Saperstein and Nicholas 1996). OCD most commonly affects the knee, dome of the talus, and capitellum at the elbow. OCD of the capitellum was also discussed previously in the context of Little Leaguer’s elbow (Sect. 27.2.3.1).
27.2.4.1 Osteochondritis Dissecans in the Elbow
OCD of the capitellum is also a frequent component of Little Leaguer’s elbow, causing insidious lateral pain and sometimes locking and catching (Kobayashi et al. 2004). OCD is a condition in which a layer of subchondral bone and sometimes the overlying articular cartilage become damaged and separate from the underlying bone, whether the fragment displaces or not. Some degree of necrosis of the fragment occurs, but the injury may heal. If the injury worsens, the fragment may eventually break down and displace (Ryu and Fan 1998). OCD of the capitellum is thought to be caused by overuse/repetitive trauma, probably shear and compressive forces that accompany the valgus load experienced by overhead throwing pitchers and similar athletes, including gymnasts. This condition is most common between the ages of 12 and 16 years (Ryu and Fan 1998; DaSilva et al. 1998).
Radiography of the elbow is the first step in imaging. Radiography demonstrates a well-defined lucent lesion with sclerotic borders (DaSilva et al. 1998), flattening of the articular surface, or fragmentation of the subchondral bone. Some cases may be radiographically occult (Kijowski and De Smet 2005b). Displaced fragments are most commonly located in the olecranon fossa (Fig. 27.40) (Kijowski and De Smet 2005c). MRI positively identifies these lesions and accurately depicts their size and whether or not there is a displaced fragment (Fig. 27.41) (Bowen et al. 2001). MRI demonstrates that the lesion occurs in the anterolateral aspect of the capitellum and often helps guide surgical intervention (Emery 2009). Surgery may be performed in the setting of unstable lesions, which rarely heal, but is largely directed by clinical findings of persistent symptoms (Kobayashi et al. 2004). On MRI, OCD is well demarcated with a linear interface surrounding a crescentic focus of high T2 signal intensity along the articular surface of the subchondral bone anterolaterally. Occasional early cases may show only the focus of the edema and may not have developed the well-defined sclerotic margin yet. MRI signs of instability include a rim of high T2 signal intensity surrounding the lesion or cysts underlying the interface of the lesion with the adjacent normal bone (Emery 2009; Kijowski and De Smet 2005b). Stable lesions have low T2 signal intensity surrounding the OCD (Kijowski and De Smet 2005b). One must not mistake the pseudo-defect of the capitellum, a common normal variant demonstrating a small focus of cartilage absence in the posterolateral capitellum, with OCD, which occurs anteriorly and laterally (Tuite and Kijowski 2006). OCD of the capitellum more often leads to an inexorable worsening of clinical findings than OCD in the knee, and chronic irregularity of the articular surface and displaced intraarticular fragments are frequent in the elbow (Bowen et al. 2001). Although surgery often improves the condition, both nonsurgically and surgically treated patients may have chronic pain, premature degenerative arthritis, and loss of terminal extension (Tuite and Kijowski 2006).
Fig. 27.40
A 14-year-old female gymnast with osteochondritis dissecans of the capitellum, presenting with elbow pain. (a) Anteroposterior radiograph of the left elbow shows a lucent lesion in the capitellum (black arrow) as well as an intra-articular bone fragment (white arrow). (b) Lateral radiograph demonstrates another intra-articular fragment anteriorly (arrow)
Fig. 27.41
Osteochondritis dissecans of the capitellum in the gymnast from Fig. 27.40. (a) Sagittal fat-suppressed T1-weighted MR arthrogram image of the left elbow demonstrates the osteochondritis dissecans of capitellum (arrow). (b) Coronal fat-suppressed T1-weighted MR arthrogram image reveals an intra-articular fragment medially (arrow)
OCD in the elbow may also affect the trochlea (Fig. 27.42). Marshall and colleagues (2009) reported a series of osteochondral lesions of the trochlea, including three cases of medial trochlear OCDs, ten cases of lateral trochlear OCDs, and five cases of osteonecrosis. The lateral trochlear OCD cases occur in a relative vascular watershed, especially in football players, pitchers, and gymnasts. Lateral trochlear OCD is also seen in longtime skateboarders. Trochlear OCD is seen less frequently than OCD of the capitellum. As with OCD of the capitellum, surgical treatment of trochlear OCD may consist of debridement, stabilization with various hardware, microfracture and drilling, or mosaicplasty (Ansah et al. 2007).
Fig. 27.42
A 15-year-old boy with osteochondritis dissecans of the trochlea. He developed elbow pain after a heavy workout including multiple pull-ups. (a) Anteroposterior radiograph of the right elbow shows a lucent lesion in the trochlea (arrow). (b) Coronal fat-suppressed proton density-weighted MRI demonstrates the osteochondritis dissecans of the trochlea (arrow)
OCD of the capitellum can be confused with Panner disease. Both lesions are best understood as osteochondral lesions of the capitellum. However, Panner disease, classified as true osteochondrosis of the capitellum (Ruch and Poehling 1991), usually occurs in children younger than 10 years and most frequently involves the entire ossification center (Bowen et al. 2001; Kobayashi et al. 2004; Maffulli and Baxter-Jones 1995). OCD develops after the age of 10 years and involves only a portion of the capitellum. Panner disease results in more dramatic findings on radiographs, resembling those of Legg-Calvé-Perthes disease of the proximal femoral epiphysis, with irregularity, fissuring, fragmentation, and collapse of the epiphysis (Fig. 27.43) (Kobayashi et al. 2004). However, Panner disease responds well when the affected extremity is rested. Clinical series report good long-term results in the vast majority of patients treated without surgery (Kobayashi et al. 2004; Bowen et al. 2001). Some think that Panner disease and OCD represent a continuum of disordered endochondral ossification, but it remains unclear if these are distinct entities or not (Kobayashi et al. 2004). Nevertheless, their radiographic findings and age at presentation differ, and the prognosis for Panner disease is much better than that for OCD.


Fig. 27.43
An 8-year-old male baseball player with Panner disease, presenting with increasing elbow pain while throwing. Anteroposterior radiograph of the right elbow reveals diffuse sclerosis of the capitellar ossification center with subchondral lucency (arrow)
27.2.4.2 Osteochondritis Dissecans in the Knee
In the knee, OCD affects the posterior lateral (mesial) portion of the medial femoral condyle in more than 70 % of cases, the central lateral femoral condyle in 15–20 % (Fig. 27.44), and the patella in 5–10 % (Kocher et al. 2006). Patellar lesions occur almost exclusively in the lower pole (Fig. 27.45), which distinguishes OCD from the upper pole location of dorsal defects of the patella (Edwards and Bentley 1977). These lesions present in children, adolescents, and young adults and are separated into two groups: juvenile OCD occurs in patients with completely open physes; adult OCD occurs in patients with closing or closed physes (De Smet et al. 1997). This distinction is important, as juvenile OCD lesions usually heal without consequence using conservative measures but adult OCD is more likely to become unstable, worsen clinically, require surgical intervention, and lead to premature degenerative arthrosis (Kocher et al. 2006; Sales de Gauzy et al. 1999). As with many other overuse injuries, the incidence of OCD of the knee is increasing in pediatric athletes, thought likely to be due to increasing participation in competitive sports (Kocher et al. 2006). There is not enough evidence to conclusively prove the cause of OCD of the knee, but most investigators believe the root cause is repetitive trauma or shear forces leading to a stress reaction that progresses to a stress fracture in the subchondral bone with components of ischemia. With cessation of impact loading, the lesion may revascularize and heal over time, but continued stresses cause further progression (Kocher et al. 2006; Micheli et al. 2006; Hefti et al. 1999). End-stage lesions delaminate on a macroscopic level and fragments displace from the bed into the joint (Micheli et al. 2006). Of the different sites in the knee, OCD occurring in the medial femoral condyle and trochlea (rare) are most likely to heal (Micheli et al. 2006). Surgical techniques for OCD include fixation with several devices such as variably threaded screws, K wires, and tacks, picking/microfracture, autologous cartilage implants, and mosaicplasty (Micheli et al. 2006).
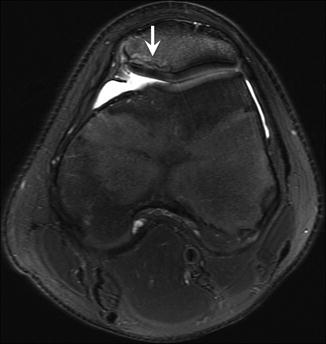
Fig. 27.44
A 17-year-old female multisport athlete with osteochondritis dissecans of the lateral femoral condyle. (a) Sagittal proton density-weighted MRI of the left knee demonstrates a large osteochondritis dissecans of the lateral femoral condyle (arrows). (b) Sagittal fat-suppressed T2-weighted MRI shows underlying cystic change (arrow)
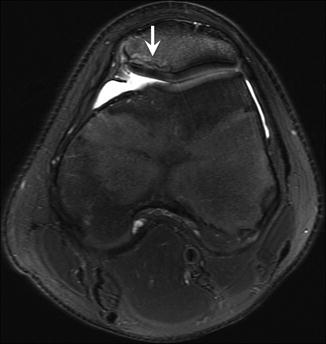
Fig. 27.45




A 15-year-old boy with osteochondritis dissecans of the patella, complaining of pain following a basketball rebound attempt. Axial fat-suppressed T2-weighted MRI of the left knee shows a patellar osteochondritis dissecans (arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree