Pierre E. Bize • Yann Lachenal • Alban Denys
Pelvic hemorrhage is usually related to unstable pelvic fractures, which are observed in up to 25% of all polytrauma patients.1 Because pelvic fractures are usually caused by high-energy trauma and often associated with injuries in other parts of the body, their management requires a multidisciplinary approach and triage decision between all bleeding sites. Despite the advances made in all disciplines of resuscitative medicine and surgery, the mortality rate following pelvic ring injuries ranges from 20% to 40%.2–5
Pelvic trauma represents a particular physiologic condition in the trauma spectrum. Usually, the pelvic compartment represents a closed space in which tamponade occurs rapidly, limiting the extension of bleeding. But in case of pelvic ring disruption, this tamponade effect does not occur, and it has been demonstrated that a gap of only 3 cm in the pelvic symphysis increases the volume of the pelvic compartment of as much as 1.5 L.6
Then, in case of pelvic fracture, patients can bleed up to 4 L of blood in a closed, difficult-to-reach compartment. According to the Advanced Trauma Life Support (ATLS) recommendation, the external stabilization of the pelvis should be performed in any case where there is suspicion or clinical evidence of pelvic fracture.7 This can be achieved at the patient’s arrival in the hospital or before using dedicated pelvic belts. A chest and pelvic x-ray should be obtained in the emergency room in all trauma patients to rule out hemothorax or pneumothorax and assess the presence or absence of evident pelvic fractures. Hemodynamically stable patient should then undergo computed tomography (CT) scan for a throughout workup. Hemodynamically unstable patients should benefit from a focused assessment by sonography for trauma (FAST) to look for free peritoneal fluid. Unstable patients with free abdominal fluid should be rushed to the operating room for exploratory laparotomy. However, note that if the peritoneum is not breached, the bleeding can be completely occult at FAST. In case of hemodynamically unstable patients without any other seriously bleeding injury and with no, or not enough, free intraperitoneal fluid to explain instability, retroperitoneal bleeding from the pelvis should be suspected.5
Bleeding in the pelvis can occur from arteries, veins, or directly from the broken bones. The immobilization of the pelvic ring with a strap or an external fixator helps restore the tamponade effect and has been shown to restore hemodynamic stability in polytrauma patients suffering from pelvic fractures.8 However, tamponade is efficient only in case of bleeding from broken bones or lacerated veins. In patients with persistent hemodynamic instability despite pelvic ring immobilization, an arterial bleeding should be suspected. In this case, four treatment options are usually described: immediate external surgical fixation, direct surgical vessel ligation, retroperitoneal packing, and transcatheter arterial embolization (TAE).9 There is no consensus on which of these treatment options is the most efficient in restoring hemodynamic stability, but there is a growing evidence in the literature suggesting that external fixation should be performed first and does not preclude any other subsequent adjuvant treatment.9 However, this can be ponderated when arterial lesions are evidenced on the CT scanner and when surgical procedure is complex and would delay arterial bleeding control by TAE.
Figure 23.1 describes the decision-making algorithm proposed by Geeraerts et al.5

There are many classifications of pelvic fractures based on the underlying traumatic mechanism or on the presence or absence of posterior ring elements instability.10 The classification of Pennal et al.11 describes three types of underlying mechanism: type 1 (anteroposterior compression), resulting in transverse opening of the pelvic ring (open book fracture) and risk of lesion of the internal iliac artery (IIA); type 2 (lateral compression), with risk of lesion of the iliac vessels and retropubic venous plexus; and type 3 (vertical shearing), with structural instability of the posterior ring elements. The classification of Burgess et al.12 adds a fourth category for mixed fractures with high risk of vascular lesions. The anteroposterior compression type and the vertical shear type of pelvic fracture are more often associated with vascular lesions.13 However, there seems to be no correlation between the type of fracture and vascular injury. The probability of vascular injury rather seems to be related to the amount of energy that caused the trauma.4 The anatomy of the IIA and its branching pattern is highly variable and needs to be well known. Figure 23.2 displays the classical anatomy of the IIA and its branches. The most commonly affected vessels are, in descending order of frequency, the superior gluteal, the lateral sacral, the iliolumbar, the obturator, and the vesical and inferior gluteal arteries.5

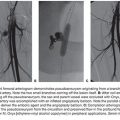
The aberrant obturator artery from the external iliac artery is a frequently overlooked source of bleeding in patients with pelvic fracture. This anatomical variant is thought to be present in 14% to 36% of cases.14 Figure 23.3 displays the angiographic aspect of the aberrant obturator artery.

The success rate of transcatheter embolization ranges from 59% to 100% and is best assessed by the rapid improvement of the hemodynamic status in the angiography suite.15 Care should be taken to recontrol the efficacy of the embolization once the hemodynamic stability has been restored as arterial spasm might mask adequate management of vascular injury or bleeding and the embolized vessels might reopen when the vasoconstriction diminishes.
DEVICE AND MATERIAL DESCRIPTION
Gelatin sponge pledgets is used as the preferred embolic agent, but N-butyl cyanoacrylate (NBCA) glue can be an efficient alternative in extremely unstable patients. Particulate agents should not be used in this setting because of the potential important ischemia that they may induce. Ischemia of the large muscular territories of the buttocks and thighs have been described. Coils should be used only in case of superselective occlusion of a single peripheral vessel. In case of a disrupted vessel, the “front door/back door” technique should be used to avoid continuous bleeding from collateral reperfusion. Coils should not be used in the proximal IIA as they will not be efficient because of the important collateralization in this anatomical region.
TECHNIQUE
Vascular access in patients with pelvic fracture can be challenging in the presence of soft tissue lesions at or near the usual site of puncture and because of compression or external fixation devices. Choice of the side of arterial puncture is usually the opposite of the bone lesions. In case of nonpalpable femoral pulse, ultrasound guidance should be used promptly. In these cases, vascular access can also be obtained from the brachial or radial arteries. The Seldinger technique is used to gain vascular access with a 5-Fr or 6-Fr introducer sheath. In case of selecting radial or brachial arterial access, use of introducer sheaths larger than 5-Fr should be avoided. The contralateral side is embolized first as the contralateral catheterization of the IIA is usually easier and the rapid control of bleeding will help stabilize the hemodynamic status of the patient. The contralateral IIA can be easily catheterized with a Cobra 2 catheter Terumo Europe, Leuven Belgium. Digital subtraction angiography (DSA) images will allow appreciation of the vascular anatomy of the IIA. Vascular lesions and active bleeding may be identified at this point. If the patient’s hemodynamic status allows, superselective catheterization of the main target vessel should always be attempted with a microcatheter. It will allow selective embolization with 0.018-in coils. Once the contralateral side is embolized, a Waltman loop may be formed in the aorta and the catheterization of the ipsilateral IIA is performed. When the patient is hemodynamically stable, multiple DSAs from different angles can be obtained to identify the site of active bleeding or vascular injury (e.g., pseudoaneurysm/sudden cutoff of any branch close to the bone fracture), which will be then catheterized and embolized superselectively. But when the patient is hemodynamically unstable, we recommend to perform just a single DSA in the posteroanterior view to confirm proper localization of the catheter in the IIA before proximal embolization is performed. In this setting, both IIAs should be occluded as rapidly as possible with Gelfoam pledgets (Ethicon, Somerville, New Jersey).
In case of hemodynamically unstable patients with multiple bleeding sites, the use of an aortic occlusion balloon catheter (e.g., Equalizer; Boston Scientific Corporation, Natick, Massachusetts) can be a lifesaver. This type of balloon can be placed even without any kind of imaging guidance in the aorta after obtaining common femoral access using Seldinger technique in the emergency department (ED). The balloon catheter is advanced 30 cm upward using the umbilicus of the patient as the target level then inflated and pulled backward until resistance is felt when the balloon reaches the aortic bifurcation. This will immediately control most bleeding in the lower body while other procedures can take place.
TAE of upper abdominal organs can be performed while an occlusion balloon is inflated by inserting a 5-Fr catheter between the balloon and the aortic wall (Fig. 23.4). Once the other bleeding sources are controlled, the balloon can be deflated and the IIA embolized.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree