and Jurgen J. Fütterer2, 3
(1)
Department of Radiological Sciences, Oncology and Pathology, Sapienza University of Rome, Rome, Italy
(2)
Department of Radiology and Nuclear Medicine, Radboudumc, Nijmegen, The Netherlands
(3)
MIRA Institute for Biomedical Technology and Technical Medicine, University of Twente, Enschede, The Netherlands
Renal Adenoma
A renal adenoma is a benign renal neoplasm. It is traditionally classified into three distinct types (renal papillary adenoma, renal tubular adenoma, and alveolar renal adenoma). The papillary type is the commonest variant with an estimated prevalence of 40 % in patients older than 70 years of age.
Such lesions are histologically indistinguishable from larger carcinomas more commonly encountered in the kidneys, and they often have histologic grades indicating a definite potential for malignant behavior. Accordingly, most investigators believe that these lesions should be regarded as carcinomas in an early stage of evolution and should not be classified as adenomas.
On CT, these small renal tumors are usually well defined and homogeneous in appearance. Less commonly, they show marginal irregularity, heterogeneity, or central calcification, findings that may suggest pathologically high-grade tumors. These lesions are best managed with partial nephrectomy, provided that the other kidney is normal.
Renal Angiomyolipoma
Renal angiomyolipoma (AML) is a type of benign mesenchymal neoplasm composed of adipose tissue, thick-walled vessels and smooth muscle elements in varying proportions. 80 % of angiomyolipomas are sporadic and have a female predilection (F:M of 4:1). 20 % can be seen in association with phakomatoses, e.g., tuberous sclerosis, and in these cases they present earlier, are larger and far more numerous.
When they are symptomatic, they present with spontaneous retroperitoneal hemorrhage. The bleeding risk is proportional to the size of the lesion, being greater if it measures more than 4 cm. Other common signs and symptoms are palpable mass, flank pain, urinary tract infections, hematuria, renal failure, and hypertension.
When the triad of adipose tissue, thick-walled vessels, and smooth muscle elements is present, the radiologic diagnosis is uncomplicated. However, “monophasic” variants exist, i.e., consisting of only one of these three components, such as the form composed exclusively of spindle-shaped smooth muscle cells, or the epithelioid variant, which is particularly problematic because it can be interpreted as a carcinoma.
On CT, most lesions involve the cortex and demonstrate macroscopic fat (<20 HU). Sometimes, especially in the context of a syndrome, they can be fat-poor.
MRI is a valuable tool at evaluating fat-containing lesions, and two main set of sequences are employed, that is fat saturated techniques (which demonstrate high signal on nonfat saturated sequences, and loss of signal following fat saturation) and in and out of phase imaging which generates India ink artifact at the interface between fat and nonfat components. It is important to remember that rarely renal cell carcinomas may have macroscopic fat components; therefore, the presence of fat is suggestive of an angiomyolipoma, but it is not pathognomonic.
Renal Bacterial Infection (Acute Pyelonephritis)
Pyelonephritis is an infectious process affecting the kidney, which is caused mainly by Gram-negative bacteria (E. coli, Proteus, Pseudomonas, Klebsiella, and Enterococcus species), whereas less than 20 % of cases are caused by Gram- positive bacteria. Ascending infections caused by bacteria of the fecal flora are the most common, especially in patients with concomitant urinary tract diseases such as lithiasis or vesicoureteric.
Acute pyelonephritis can be defined as a clinical syndrome characterized by lumbar pain and hyperpyrexia, associated with laboratory findings of renal bacterial infection including leukocytosis, pyuria, bacteriuria, and positive urine culture. In anatomopathologic terms, pyelonephritis is a bacterial infection of the kidney, with consequent acute inflammation often involving the pelvis and renal parenchyma of both kidneys. This causes suppurative interstitial inflammation with tubular necrosis.
Imaging is needed to determine if there are complications requiring prolonged antibiotic therapy or surgical intervention (e.g., renal and perinephric abscess or pyonephrosis). Imaging is also useful for excluding abnormalities that predispose to refractory infections such as nephrolithiasis or ureteral obstruction.
In patients with acute bacterial renal infection, CT scans are acquired with contrast enhancement during the corticomedullary phase (30 s after initiation of injection) and during either the nephrographic phase (70–90 s after injection) or the excretory phase (5 min after injection). A nephrogram on contrast-enhanced CT that consists of discrete rays of alternating attenuation extending to the cortex is characteristic of pyelonephritis and is better demonstrated on CT than on excretory urography. Striations result from stasis of contrast material within edematous tubules that demonstrates increasing attenuation over time. Severe tubulointerstitial inflammation may progress to form a hypodense mass or masses with rounded or irregular contours and bulging of the renal surface. If treated too late or inadequately, such lesions may develop single or multiple small areas of liquefaction (i.e., small abscesses). These areas are often irregular and of near water attenuation (20–30 HU); they do not enhance after intravenous administration of contrast medium.
Renal Cell Carcinoma
The most common renal cancer is the carcinoma (renal cell carcinoma, RCC), which accounts for 3 % of all adult cancers and 80–85 % of malignant renal tumors.
Patients with RCC can present with a range of symptoms; unfortunately, many patients are asymptomatic until the disease is advanced. At presentation, approximately 25 % of individuals either have distant metastases or advanced locoregional disease. The classic triad of RCC (flank pain, hematuria, and a palpable abdominal renal mass) occurs in most 9 % of patients. Many patients with RCC present with or subsequently develop systemic symptoms or paraneoplastic syndromes.
Of all the available prognostic factors, tumor extension at diagnosis is the most important element for predicting disease progression; as a result, CT plays a key role and still today can be considered the best imaging modality for staging RCC.
CT is currently recognized as the best imaging technique for identifying renal parenchymal neoplasms. CT can identify more and smaller lesions than US, although it is unable to improve on their characterization; Fig. 8. There are two fundamental aims to the characterization of solid renal lesions to distinguish a renal tumor from normal anatomic variants or pseudotumoral lesions which can mimic a neoplasm (e.g. lobar dysmorphism or fetal lobulations) and to differentiate benign from malignant forms. CT can suggest a growth pattern is infiltrative rather that expansive (in the latter the tumor is bounded by a pseudocapsule). Involvement of the inferior vena cava is demonstrated by extension of the renal vein thrombus into the vena cava itself, where it becomes evident as an intraluminal defect. CT remains the most immediately used imaging modality for the evaluation of distant metastases (lungs, liver, and skeletal system). The most specific CT parameter for classifying a solid mass as T3a is provided by the identification of a solid enhancing nodule in the perirenal fat, which possibly behaves in a similar manner to the primary lesion. Stranding and increased thickness of perirenal fat are not necessarily signs of tumor spread, since they are identifiable in 50 % of patients with lesions confined to the capsule.

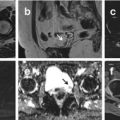
Fig. 8
CT images showing a capsulated renal mass with inhomogeneous contrast enhancement on arterial and venous phase which was found to be a Renal Cell Carcinoma. MR images depicting a round-shaped, well-capsulated renal mass with inhomogeneous high signal intensity on T2-weighted images and contrast enhancement, without any signs of infiltration of renal vein. After surgery this mass was found to be a Renal Cell Carcinoma
MRI has an important role to play in the characterization of renal lesions. Thanks to the efficacy of the dynamic study, the increase in signal intensity can be measured over time and the vasculature of small lesions can be evaluated. In T1-weighted images medium to large lesions can appear hypo-isointense or even weakly (but never clearly) hyperintense. In T2-weighted sequences, the appearance is hypo- and hyperintense. MR is able to resolve the problems CT has with complex cysts, i.e., small lesions with calcified walls, in which the absence of enhancement can help make the diagnosis of benign lesions.
Renal Cysts (Simple Renal Cyst)
The most common causes of radiologically evident renal cysts in adults are simple renal cysts, which will be discussed here, autosomal dominant polycystic kidney disease, and, acquired cystic disease in patients with end-stage renal disease after several years of dialysis, particularly hemodialysis. Unusual causes of renal cysts in adults are Von Hippel–Lindau disease, tuberous sclerosis complex, and nephronophthisis. Postmortem studies have shown that more than 50 % of people under the age of 50 have one or more cysts.
To help diagnose and manage these lesions, the Bosniak renal cyst classification system was created. Based upon morphologic and enhancement characteristics with CT scanning, cystic renal masses are placed into one of five different categories. The presence of true contrast enhancement of the lesion (a minimum increased attenuation of 10–15 Hounsfield units) is the most important characteristic separating categories III and IV, which are associated with malignancy in 40–90 %, from the categories I, II, and IIF, which are typically benign processes.
MRI is typically used to evaluate patients with indeterminate lesions. In addition to signal characteristics, MRI evaluates the same morphologic findings as described above for CT scanning: wall thickening, nodularity, septa, and enhancement. One difference is that MRI does not detect calcification. MRI is especially useful for characterizing internal contents of cysts, such as hemorrhage or mucin, and is more sensitive than both ultrasonography and CT in showing enhancement of internal septations. The combination of mural irregularity and intense mural enhancement had the highest correlation with malignancy.
Serial MRI examinations at 3, 6, and 12 months are warranted in patients with indeterminate lesions on gadolinium-enhanced MRI.
Renal Lipomatosis
Renal sinus lipomatosis refers to a condition where there is excessive renal sinus fat replacement, which can be due to inflammation, renal parenchymal atrophy, renal stones, ageing or steroids.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree