Introduction
The interpretation of the pediatric cervical spine can be difficult for those unfamiliar with the normal pattern of development and ossification of the spine. There is a real risk of both false-negative and false positive interpretative errors.1 An understanding of this helps to avoid pitfalls in interpretation. There are a number of predictable epiphyses, apophyses, and synchondroses that may be misinterpreted radiographically as fractures. There is also a wide range of normal variants with specific morphological and radiological characteristics. In addition spinal movement patterns also differ from those expected in the adult.
The appearance of the secondary ossification centers in the growing spine can be associated with radiographically subtle but significant physeal injuries. Although the pediatric spine assumes many of the adult radiographic features by the age of 8 years, as in the peripheral skeleton, potential injuries related to these relatively vulnerable physes should be given due diagnostic consideration.
The incidence of spinal injury in childhood and adolescence is variably reported between 1 % and 9 % of the total reported spinal injuries. This implies that accident and emergency staff and radiologists are unlikely to see this injury on a regular basis in the same hospital. This lack of experience and teaching material increases the risks of missed diagnosis. Cervical spine injuries in particular may be more common than is currently recognized as they are easily overlooked on plain radiographs. Aufdermaur identified injuries through endplates of vertebral bodies in an autopsy study, but only 1 in 12 was suspected to have sustained a spinal injury before autopsy.2 Road traffic accidents and falls are the most frequent mechanism of injury in the childhood group as a whole. However, in the older child and adolescent, sports-related injuries including diving, surfing, and cycling account for a number of cases.
The pattern of cervical spine injury affecting the child differs from that in the adult. In the younger child (< 8 years), there is a predominance of upper cervical spine injury over the lower cervical region, which is the opposite of that seen in adults. The upper cervical spine is more vulnerable to injury due to a number of anatomical and physiological features. These include the unique pattern of ossification of C1 and C2, the poorly developed neck musculature, the relatively large size of the head compared to the cervical spine in the child, the fulcrum of movement being located in the upper cervical spine in the young child as opposed to the mid to lower cervical region seen in the older child and adult, ligamentous laxity, and underdeveloped skeleton of the spinal motion segments. Adult type of injuries (over 8 years of age) occuring in the pediatric age group will not therefore be the emphasis of this chapter as they are covered in previous chapters.
There are a number of subsets of spinal injury that are predominant or even unique to children. Trauma to the spine occurring at birth is rare, and although uncommon, trauma to the spine in nonaccidental injury has become increasingly recognized, while SCIWORA (spinal cord injury without radiographic abnormality) is more commonly seen in children than in adults.
In order to understand the different patterns of injury and avoid errors of interpretation it is important to be familiar with the development of the spine, its radiological appearances and the range of normal variants before embarking on the imaging of the various pathological conditions.
Development of the Vertebral Column
The term centrum describes the central part of a developing vertebra. It encloses the notochord and gives rise to most of the vertebral body. A “neural process” extends dorsally on each side of the neural tube and later in the fetal period the right and left processes unite to complete the neural arch, which forms the vertebral arch and a small portion of the vertebral body. In the centrum, endochondral ossification commences at approximately 9 weeks of fetal life. Bipartite centers (anterior and posterior) associated with the arrangement of the blood vessels may be encountered. Coronally cleft vertebrae may occur up to the age of 4 years and are considered to be a normal variation of endochondral ossification3 that depends on varying patterns of vascular distribution.4 The junctional area between the centrum and the neural arch is termed the neurocentral synchondrosis.
At birth most vertebrae have three ossific areas—one for the centrum and one for each half of the neural arch. The ossific center of a centrum in the newborn is ovoid on a lateral radiograph. The ossific center of each vertebral centrum is separated from that of the neural arch by the broad radiolucent synchondrosis that contains uncalcified cartilage. Bony union takes place here between 3 and 6 years. Anteriorly and posteriorly there are small indentations or clefts that represent vascular channels running through the ossific center. As normal growth occurs, the vertebral bodies as seen on a lateral radiograph become more rectangular, while the height of the vertebral body compared with the disk space increases.
In early childhood the vertebral endplate has a thick hyaline cartilage component. Growth forces at the diskovertebral interfaces, which are both elliptical in their enlargement contours, have an effect on the distribution of the cartilage components (physes) superiorly and inferiorly. There are no separate epiphyseal ossification centers in the growing human vertebrae, but due to the mechanics in operation the growth cartilage becomes increasingly thin centrally, with a thicker periphery laterally and anteriorly which becomes the ring apophysis. First visible at approximately 5 years they represent an annular recess that surrounds the vertebral body and will form the secondary ossification center of the vertebral endplate. The recess is filled with cartilage. Initially on lateral radiographs the ring apophysis appears set in a superior and inferior groove anteriorly at the borders of the developing vertebra. This is an area of active growth and remodeling carrying significant biomechanical shearing, compressive forces and not just traction stresses. Small calcific foci begin to appear in this cartilaginous rim at 6-8 years in girls and 7-9 years in boys.5 Ossification of this ring apophysis may not occur simultaneously in the superior and inferior components and must not be mistaken for a fracture. These foci slowly ossify and gradually unite to form a bony vertebral ring—the vertebral ring apophysis. The vertebral ring apophysis/growth plate parallels the superior and inferior vertebral margins and in infants and young children it extends substantially over the superior and inferior aspects of the anterior vertebral margin.5 The fusion of individual foci to form a unified rim is complete at 12 years. Prior to that, the child’s spine assumes adult characteristics by ages 8-10 years.
The neural arches of C1 and C2 show well-developed ossific areas bilaterally at birth, but perichondral ossification of the neural arches here and elsewhere is not complete at birth. The spinous processes do not yet possess their own ossific centers and are formed during the first year by amalgamation of the neural arches. This begins in the lumbar area and spreads to be complete in the cervical spine in the second year. Union may not occur in the atlas until the fourth to sixth year and in the sacrum until the seventh to tenth year. Fusion between the base and apex of the dens usually occurs by 12 years.
Secondary centers of ossification (apophyses) form along the tips of the spinous processes during the years of adolescent growth (11-14 years), formed as small ossific centers that eventually cap the entire tips of the spinous processes. These unite with the spinous processes when vertebral growth is complete. The tips of the transverse processes in the lumbar region show occasional development of secondary ossific centers. The first two cervical vertebrae are atypical. The central pillar of the axis develops as three segments: (i) the tip of the dens; (ii) the base of the dens; (iii) the centrum. Ossification occurs in the order of the centrum, the base of the dens (appearing at birth) and finally the tip of the dens, the latter occurring before 2 years but not constantly present. The base of the dens has two centers of ossification.
Normal Variants
Visualization of the spine in its developmental stage reveals different stages of ossification. On the radiograph areas of lucency may be representative of cartilaginous development, so knowledge of the expected appearance and approximate age of appearance of different ossification centers will help in interpretation. Synchondroses have smooth well-corticated margins and occur at characteristic sites and awareness of this will avoid misinterpretation of these as fractures. The atlas and the axis have a different developmental and hence morphological appearance to the other vertebrae.
The ossification center for the anterior arch of the atlas is present in 20 % at birth but usually appears during the first year.It may, however, be absent resulting infailure of anterior fusion leaving a cleft. The body of C1 joins the neural arches by synchondroses that close by the seventh year, but the ring of C1 reaches its normal adult size by the fourth year (Fig. 8.1). The pattern and sequence of ossification of the axis, including the centrum, the odontoid process, and the apex of the odontoid process have been referred to above. The basilar odontoid synchondrosis usually fuses between 3 and 6 years of age but closure may be delayed. This should not be mistaken for a fracture. The vestigial form may still be visible up to the age of 11 years, represented by a fine sclerotic line, but should be clearly differentiated from a fracture line that will appear clearly lucent. This vestigial remnant can remain discernible on CT and MRI images into adult life. Fractures of the peg typically occur above the level of the synchondrosis and may ultimately give rise to an os odontoideum (see later). The ossification center at the apex of the odontoid process appears at approximately 2 years of age and fuses to the larger odontoidprocessatapproximately12 years. Sometimes the appearance of the apical ossification center may be delayed, or it may even not appear at all.
Disturbances in alignment of the vertebral bodies in the cervical spine may arouse concern about underlying occult injury. Hypermobility, ligamentous laxity, and incomplete ossification may be responsible for these appearances. A number of normal variants occur in a child, which would give rise to alarm if seen in the adult patient. These include:
Pseudo Jefferson fracture (pseudospreading of C1). In young children the ossification of the lateral mass of C1 often exceeds that of the ossification of C2 giving rise to what has been called the pseudospread of C1 on C2 (Fig. 8.1).
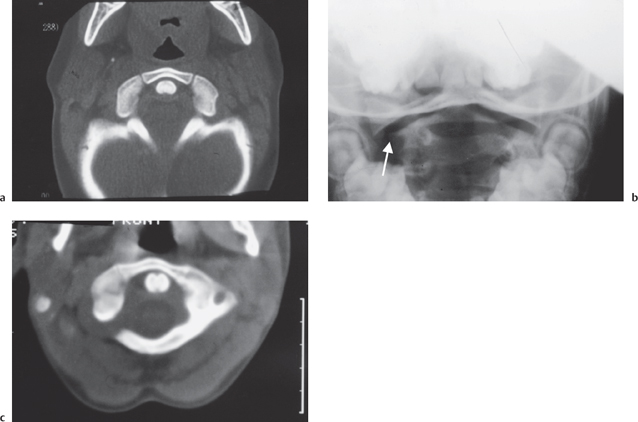
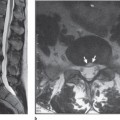
Fig. 8.1 a Axial CT of the normal development of the C1 vertebra with the odontoid peg equidistant from the synchondroses of the anterior body of C1. Pseudo Jefferson fracture of C1 with lateral offset on the radiograph on the right (arrow) (b) due to unequal growth at the synchondroses of C1 producing elongation on the right as judged by the odontoid peg (c).
Pseudosubluxation of the body of C2 on C3 is a well-recognized phenomenon. Forward movement of the second cervical vertebra on the third during flexion and extension of the spine is noted. The phenomenon is a combination of forward shift and flexion of the second cervical vertebra on the third. Pseudosubluxation of up to 4 mm is acceptable in a child. Bailey indicated that attention to both symmetry of the curve and the relative positions of adjacent cervical vertebrae is necessary to identify this phenomenon.6 Cattel and Filtzer described a method for measuring the degree of anteroposterior movement of C2 on C3.7 They noted marked to moderate anterior displacement in 39 of 160 children aged 1-16 years and a definite tendency towards anterior displacement in 28 out of 160. Hypermobility with ligamentous laxity were thought to be a contributory factor but also the relative horizontal plane of the articular processes in the upper cervical region as described by Sullivan and colleagues may allow greater forward gliding of C2 on C3.8 Anterior wedging, a further normal variant (see below) may also contribute to the appearance. Swischuk described a line to help differentiate physiological from pathological C2 anterior displacement.9 If a line is drawn between the anterior margin of the spinous processes of C1 and C3, in physiological subluxation the anterior aspect of the spinous process of C2 should lie within 2 mm of this line (Fig. 8.2). If it lies more than 2 mm either anterior or posterior to this line then pathological subluxation is present.10 Cattel and Filtzer also observed posterior displacement in extension at the C2/C3 level.7 Anterior displacement of C3 on C4 was also observed in 14% of cases. The radiographic depiction of pseudosubluxation, however, must always be correlated with the clinical status. In instances of persistent cervical symptoms further imaging and follow-up will still be required despite the radiographic demonstration of pseudosubluxation to exclude a hidden injury (Fig. 8.2).11 The underlying anatomic and physiological factors promoting C2/C3 pseudosubluxation are also in play in a traumatic event, rendering this level susceptible to trauma. Indeed 7 out of 11 patients with presumed pseudosubluxation were shown to have a true injury.12
Vertebral pseudowedging. Anterior wedging is merely a radiographic appearance of the vertebrae due to the pattern of vertebral ossification and is not morphological. The apparent wedging of vertebral bodies has been observed by a number of authors on lateral views of the cervical spine. Immature vertebral bodies are oval in shape with smooth rounded corners and gradually become more rectangular in shape with age. A study by Swishuk et al13 demonstrated that in infants and young children some developed a wedging deformity of the vertebral body ossification center involving the anterosuperior corner of the vertebral body (Fig. 8.4). Swischuk studied the lateral cervical spine radiographs of 481 children ranging in age from birth to 19 years and confirmed that cervical vertebral bodies generally mature from an ovoid shape to a rec-
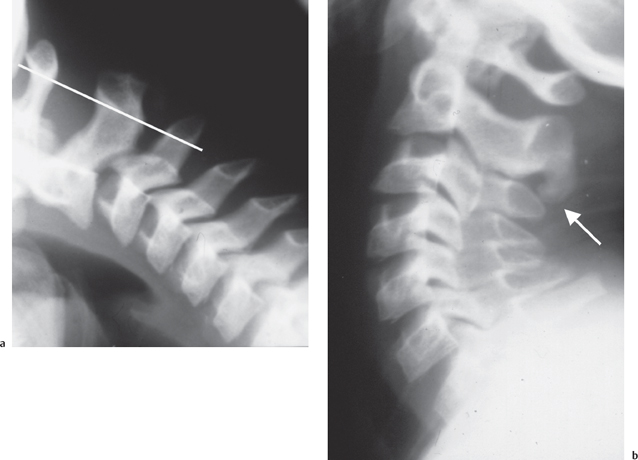
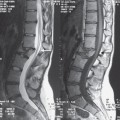
Fig. 8.2 Pseudosubluxation of the body of C2 on C3 confirmed by the continuous spinolaminal line drawn between C1 and C3 (a). Despite the radiographic appearance, due to ongoing symptoms appropriate treatment and follow-up was required which revealed a hidden injury of the osteo-ligamentous attachment at C2/C3 highlighted by new bone formation (arrow) (b).
tangular adult shape, but that at the level of C3 some infants and children develop a wedging deformity of the vertebral body ossification center. This appearance was occasionally seen at C4 but was not seen at other levels. The incidence of this anterior wedging decreased with increasing age, being present in 14/481 patients between birth and 3 years, and seen only in 2/481 patients between 13 and 19 years.13 It was postulated that chronic exaggerated hypermobility caused chronic repetitive impaction of the vertebral body of C3 by C2. Thus hypermobility of the upper cervical spine in infants and children is most pronounced at the C2/C3 level, which is also the fulcrum of movement in this age group, and can be associated with a number of normal variants. These include anterior wedging, actual anterior displacement of the vertebral body, or marked angulation at the C2C3 level.
Congenital spondylolysis. Farndon and Fielding in 1981 used the term “pedicle defect” to encompass a congenitally absent pedicle, congenital spondylolysis, and persistent synchondrosis.14 In the cervical region C6 is most commonly involved. The lytic defect may be uni-orbilateral. There may be dysplasia of the posterior elements and a compensatory change in levels above and below the vertebra involved (Fig. 8.3).15,16 Patients may give a history of neck or shoulder pain precipitating the radiographic examination or it may be detected incidentally during imaging following a history of trauma. The abnormality is usually suspected or clearly diagnosed from features on the radiograph. These include the well-corticated margins of the spondylolytic defect, hypoplastic facets, and spina bifida occulta. CT can readily confirm these findings (Fig. 8.3). The lesion can be difficult to detect on MRI but absence of the spinous process on sagittal sequences should alert one to the possibility of the diagnosis.15
The space between the posterior aspect of the anterior arch of the atlas and the front of the odontoid peg (atlanto-axial or atlanto-odontoid distance) normally measures approximately 4 mm in children (the equivalent adult distance is 2-3 mm). This wider distance in the child is due radiographically to the lucent unossified atlanto-dens cartilage with a degree of ligamentous laxity. The atlanto-odontoid space can widen in flexion up to 5 mm.
There may be overriding of the anterior arch of the atlas on the odontoid process in extension. In Cattel and Filtzer’s study7 overriding was said to be present when more than two thirds of the visible anterior arch of the atlas lay above the superior margin of the odontoid process.
Absence of the normal lordotic curvature in the neutral position in adults can be considered to represent spasm and be indicative of underlying bone or soft tissue injury. Absent lordosis has, however, been observed by Juhl et al17 and Fineman et al18 as occurring in normal subjects and, therefore, not necessarily indicative of injury.
Marked angulation at a single intervertebral level was observed by Cattel and Filtzer7 and was felt to probably be the result of the relative laxity of the interspinous, interlaminar, and posterior longitudinal ligaments.
In Cattel and Filtzer’s study absent flexion curvature of the spine between the second and seventh cervical vertebrae with the neck in flexion was described.7
There is a wide range of normal variants occurring in the pediatric spine.19 Many of these variants relate to hypermobility related to ligamentous laxity and to incomplete ossification, which renders a very different appearance than that seen with the adult spine.
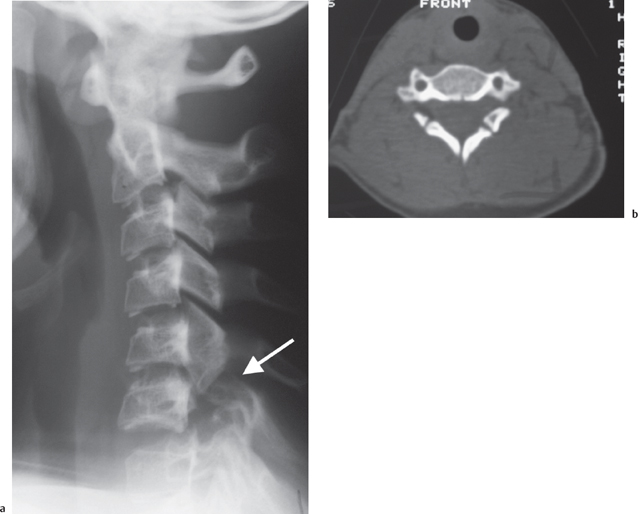
Fig. 8.3 Congenital spondylolysis of C6 seen on the lateral cervical radiograph (arrow) (a), with evidence of failed fusion at all synchondrotic sites at C6 on the CT (b).
Birth Injury
Injury to the spinal cord is a tragic event that can occasionally occur as a complication of traumatic birth delivery. When it occurs it is usually in association with a breech presentation involving the lower cervical and upper thoracic spine. Although the vertebral column with its intact ligaments is flexible and can stretch, there is a very limited degree of elasticity afforded to the spinal cord and “over stretch” may result in cord injury. When cord injury occurs in association with a breech presentation this is usually at the cervicothoracic junction probably as a result of traction. This contrasts with the high cervical cord injury, which is the usual injury that occurs with a cephalic presentation, and is thought to be due to rotation.20 There is usually little to find on spinal radiography. The diagnosis is often suspected on the basis of the history of a difficult delivery, neurological signs, and respiratory symptomatology, including pneumonia occurring secondary to weak respiratory muscles. MRI is valuable in demonstrating cord signal abnormality.
Nonaccidental Injury (NAI)
The true incidence of NAI induced spinal injury is unknown. In part this is due to the previous lack of routine acquisition of AP and lateral views of the spine in suspected NAI cases. It is unusual to see obvious vertebral fractures in cases of nonaccidental injury. In this setting the presentation is more likely to be that of neurological disturbance in the presence of normal radiographs. This is because of the elasticity of the spine. Severe shaking or other trauma may induce cord hemorrhage or edema in the absence of actual fracture. In Brown’s review of 103 cervical spine injuries in children, the three cases of child abuse were all associated with SCIWORA.21 Studies,22 however, have demonstrated that most changes are anteriorly located with subtle compression fractures of vertebrae, some of which may extend into the growth plate. Posterior neural arch fractures are unusual. These have been identified at postmortem. “Typical” fracture patterns have been described as in the paper by Kleinman and Marks.22 They reported on the postmortem radiological and histopathological findings in 10 cases of vertebral body fractures occurring in infants and young children. Three patterns were noted: (1) Compression only—mild compression deformity (<25%) of the anterior half of the vertebral bodies without disruption of the endplate. (2) Fracture with superior endplate extension. These fractures involved the anterosuperior aspect of the vertebral body with extension into the anterior aspect of the endplate. This tended to undermine a variably sized bone fragment. Histologically the fractures entered the cartilaginous growth plate of the superior endplate. (3) Combined lesions. With increasing compression deformity of the vertebral bodies, extension of the fracture into the proliferative zone of the superior cartilaginous growth plate was more extensive. In cases of nonaccidental injury there is usually evidence of injury elsewhere in the skeleton particularly in relation to long bones and/or rib fractures.
Cervical Spine Injuries
Atlanto-Occipital Dissociation (AOD)
The higher incidence of upper cervical injuries in children compared with adults is also reflected in this injury, which is twice as frequent in the pediatric age group. This rare injury is usually fatal, but in survivors the diagnosis can be clinically difficult to make. In the first instance these victims are usually suffering from severe polytrauma, especially head injuries. In addition the clinical picture is variable with a spectrum of neurological (cranial nerve, quadriplegia, sub-brain stem complete loss), respiratory, and cardiovascular (hypotension, tachycardia, cardiac arrest) dysfunction. The mainstay of diagnosis is based on radiological appearances which are readily appreciated if there is residual atlanto-occipital dissociation at the time of examination. In some instances it is not an easy diagnosis to make when spontaneous anatomical reduction and alignment is restored, but this can become apparent on the lateral radiograph taken immediately after skull traction. The Powers ratio is helpful in identifying the presence of AOD being based on two simple measurements. The distance between the anterior rim of the foramen magnum and the posterior arch of the atlas is divided by the distance between the posterior rim of the foramen magnum and the anterior arch of the atlas. Values greater than 1.0 are abnormal while less than that are definitely normal. This measurement however has been shown to be unreliable when anterior injuries reduce spontaneously, in posterior atlanto-occipital injury, in the presence of an atlas fracture or congenital cranio-vertebral junction osseous abnormalities. To overcome this problem the dens-basion distance can be measured as well as the interspinous C1/C2 and C2/C3 distances. A dens-basion distance over 14 mm was the mainstay of diagnosis in 11 patients with atlanto-occipital dissociation.23 A C1/C2:C2/C3 ratio greater than 2.5 indicates ligamentous injury. In instances of equivocal radiological measurements, CT and MRI can be employed to identify malalignment and cranio-cervical hemorrhage, respectively. MRI may also be useful if the neurological status deteriorates to exclude hydrocephalus and retropharyngeal pseudomeningocele complications.
Fractures of C1
The Jefferson fracture is a comminuted fracture of the atlas involving both the anterior and the posterior arches of the ring. Most Jefferson fractures occur as a result of a significant impact on the head, such as a fall, or a blow to the vertex. The force is transmitted through the occipital condyles and into the atlas. Although a rare injury in the young child, it needs to be differentiated from both a normal variant appearance and developmental defects. The fracture may also occur through the neuro-central synchondroses, which may remain unfused until the age of 7, and this is best diagnosed by CT.24, 25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree