Introduction
Anatomy
The vertebral endplate consists of a layer of cartilage that covers the surface of the disk, separating the disk from the adjacent vertebral body. It is debatable whether the endplates are strictly components of the disk or whether they actually belong to the vertebral body, but they are often described as being part of the intervertebral disk.1 The intervertebral disk is composed of a central nucleus pulposus with a surrounding annulus fibrosus. The nucleus pulposus is a semi-fluid mass of mucoid material, rather like toothpaste. The annulus fibrosus consists of collagen fibers that surround the nucleus pulposus in concentric rings. The endplate lies on the superior and inferior surfaces of the intervertebral disk, so the nucleus pulposus is in direct contact with the endplate (Fig. 9.2.1). The endplates are attached to the subchondral bone of the vertebral body. In small pockets over the surface of the subchondral bone, the bone is deficient allowing the marrow cavity to abut the surface of the endplate. The intervertebral disk has no direct blood supply, and indeed is the largest avascular structure in the body. The pockets of deficient subchondral bone facilitate the diffusion of nutrients from blood vessels in the marrow space and are important for the nutrition of the endplate and intervertebral disk. They do, however, represent relative areas of weakness, which can allow the nucleus pulposus to herniate directly into the vertebral body, forming a Schmorl’s node.
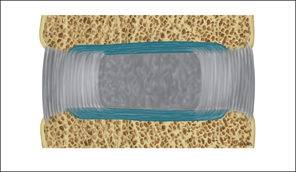
Fig. 9.2.1 Diagrammatic representation of a sagittal slice through the intervertebral disk. The nucleus pulposus is in direct contact with the cartilage of the vertebral endplate.
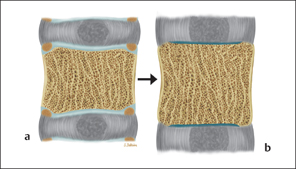
Fig. 9.2.2 a Sagittal slice through the vertebral body and disk in adolescence. The ring apophysis is separated from the vertebral body by a thin layer of hyaline cartilage and is an area of relative weakness. b The ring apophysis fuses with the vertebral body. The peripheral fibres of the adult annulus have a bony attachment, while the more central fibres insert into the vertebral endplate.
In the immature spine, a cartilaginous growth plate on the superior and inferior surfaces of the vertebral body achieves growth in vertical height. At maturity the subchondral bone plate develops on the vertebral body side of the growth plate, with the cartilaginous endplate on the other. Until the endplate ossifies, the cartilaginous growth plate of the immature spine is relatively weak and prone to injury, resulting in endplate abnormalities.
The ring apophysis develops between the ages of 7 and 9 years. It consists of a ring of ossification at the edge of the cartilaginous plate. It fuses with the vertebral body at some time, usually between the ages of 14 and 18 years (Fig. 9.2.2). Before fusion, the ossification is separated from the rest of the vertebral body by a thin layer of hyaline cartilage and this area represents a relative region of weakness. Herniation of the nucleus pulposus can occur through this region, permanently separating the ring from the vertebral body forming a limbus vertebra (Fig. 9.2.3).

Fig. 9.2.3 Sagittal T2W MRI through the lumbar spine. L3/L4 limbus vertebrae. The intervertebral disk has prolapsed between the ring apophysis and vertebral body at the superior endplate of L4, permanently separating the apophysis from the body.
Scheuermann’s Disease
In 1921 Scheuermann described a condition characterized by vertebral body wedging resulting in a kyphosis of the lower thoracic spine.2 Hereditary factors have long been thought to be important in the pathogenesis of the disease.3,4 In 1977 Alexander proposed a theory that there were two types of Scheuermann’s disease.5 The classical form, as described by Scheuermann, occurs around the T7 to T10 levels, while the traumatic form occurs lower down at the thoracolumbar junction. This type, found in young athletes undergoing a variety of sports, has been termed “atypical Scheuermann’s.”6,7 It should be of no surprise that mechanical factors have their greatest affect on the spine at this level, since this is the region of greatest mobility in the thoracic and lumbar spine. The thoracolumbar junction includes the T11 and T12 vertebrae, as the floating ribs at these levels provide no structural support, unlike the bony ring of spine, ribs, and sternum higher up the thoracic spine. The mechanical forces induced by chronic sporting activities particularly affect the anterior portion of the vertebral body, and this is an important distinction to make from the classical Schmorl’s nodes.
Schmorl described a herniation of the intervertebral disk through the endplate in 1927.8 Schmorl’s nodes are very common and occur in 19%of asymptomatic individuals,9 and occur equally frequently in athletic and nonathletic individuals.10,11 An acute herniation of the disk into the vertebral body is usually not visible on a plain radiograph until bone repair forms a sclerotic edge around the herniation. Unlike chronic Schmorl’s nodes, the acute Schmorl’s node is a painful condition and is best demonstrated by magnetic resonance imaging, which shows bone edema within the vertebral body (Fig. 9.2.4).12 Little is known of the natural history of the acute Schmorl’s node in terms of the MRI appearances, but since it represents an acute fracture, reactive bone edema can be expected for at least 6 months. After this the edema subsides, but the Schmorl’s node remains as a chronic lifelong feature. Whilst Schmorl’s nodes are undoubtedly a feature of the endplate abnormalities of Scheuermann’s disease, the demonstration of Schmorl’s nodes in themselves does not constitute a diagnosis of Scheuermann’s disease, since this requires anterior endplate abnormalities with wedging. In the athlete with back pain, Schmorl’s nodes can largely be discounted as being of any significance, except in the acute stages when they are responsible for an acute onset of back pain.
Atypical Scheuermann’s disease, with anterior endplate lesions occurring at the thoracolumbar junction has been demonstrated in relation to athletic activity.11,13–15 The most commonly investigated groups have been gymnasts and elite skiers. The competitive nature of sports is leading more children into strenuous activity at an earlier age in order to gain an advantage over rival competitors, but this subjects the spine to mechanical forces during a vulnerable period of growth. Most studies have concentrated on the plain radiographic appearances in young athletes. It is generally accepted that there is a poor correlation between plain radiographic findings and patient’s symptoms, with many plain radiographic abnormalities being found in asymptomatic individuals.16,17 The demonstration of endplate abnormalities in the thoracolumbar region on plain radiographs therefore does not necessarily explain a patient’s symptoms.
Whilst most studies have simply documented the incidence of endplate abnormalities in athletes, a study by Ogon et al correlated these abnormalities with lower back pain.18
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree