Introduction
Spondylolysis is an interruption of the pars interarticularis of the vertebral pedicles due to abnormal stress. This is usually a chronic recurrent form of stress, and acute episodes of trauma causing pars fractures are rare. Clinically, it manifests mainly during the second decade of life and it is in most cases located in the fifth lumbar segment. Spondylolysis is most commonly observed in males and has a male to female occurrence ratio of 2-3:1, as well as a higher probability of occurrence with inherited traits.1,2
Although some patients are asymptomatic, spondylolysis seems to be the most significant cause of lower back pain in athletes and in this group it is observed to occur more frequently than in the general population.3,4 Certain movement patterns associated with various types of sports (Table 9.1.1) may be causal in the development of spondylolysis in athletes as well as in other physically active individuals.5 Most notably younger, skeletally immature, athletes are at higher risk of spondylolysis during times of rapid skeletal growth.6 There is also a racial preponderance with a prevalence of 5-7% in Europeans, 9% in Bantus, 7-10% in Japanese, and up to 50% in Eskimos.7
| Applied force | Type of activity |
| Repetitive hyperextension maneuvers | Gymnastics, wrestling, diving, throwing sports, basketball, volleyball, pole vaulting, certain swimming styles (butterfly), high diving |
| Strong muscle forces | Body building, wrestling, hockey |
| Repeated monotonous exercises | Rowing |
| Rotational motion creating unilateral defects | Throwing sports, golf |
| High and various degrees of movement | Football, track and field athletics, dancing, Figure skating |
The development of spondylolysis is thought to derive from differential stress applied to the pars interarticularis of the vertebral arch. Therefore, spondylolysis is classified as a stress fracture of the vertebral arch and the numerous theories concerning its etiology may in principle relate to this concept.8,9 Brocher hypothesized in 1950 that spondylolysis develops from a congenital cleft.10 Such a defect, however, does not occur in this part of the vertebral arch, in which the perichondral ossification centers are located.11 So far spondylolysis has not been observed in neonates.7 Spondylolysis seems to develop in childhood around 6 years of age without clinical symptoms.1, 8 Niethard et al attributed the frontal orientation of the facet joints of the lower spine to a reduction of stability in this area and an increase in mobility, thus resulting in increased mechanical stress.12 In the early Medieval period, the prevalence of spondylolysis in an area of south-western Germany hasbeen shownto have been the same as its prevalence in the same area today.13
Low stress-resistance is mainly due to an elongation and thinning of the pars and is exaggerated by a prominent lordosis of the lumbar spine. Such lordosis especially develops between 6 and 8 years of age and is associated with a physiological flexion of the hip joints. Radiological evidence of a lumbosacral transitional vertebra (Fig. 9.1.1), a congenital cleft of the posterior arch of the S1 segment (spina bifida occulta), or of a zygapophyseal joint anomaly is strongly associated with spondylolysis of L5.9 Spina bifida occulta has been described to occur in between 13% and 58% of cases concomitant with spondylolysis.12 Spondylolysis also occurs in patients with Marfan’s syndrome and EhlersDanlos syndrome; inthe latter disease itmay besevere. Osteogenesis imperfecta and osteopetrosis are other forms of systemic diseases related to spondylolysis.
Repeated microfractures are mainly related to hyperextension movements, thus amplifying the lordotic state. Muscle strength and tension may influence the development of spondylolysis through shortening or tightness of the hamstring muscles of the thigh with increased tension on the posterior vertebral arches of the lower lumbar spine. Weakening of the spinal and the anterior abdominal wall muscles is a precursor in the development of spondylolysis, too, whereas strengthening parts of these muscles should have a preventive effect.
In the later course of spondylolysis, fibrous or bony callus formation at the pars defect site may develop. Bony outgrowths, facet joint arthrosis, or instability may lead to nerve root impingement with leg pain, numbness, or weakness.
With longer exposure to applied forces the isthmic form of spondylolisthesis may develop. It is a forward movement of the body of one of the lumbar vertebrae on the vertebra below it, whereas the posterior joints and the neural arches are aligned with the posterior elements of the inferior vertebral body. A fully dislocated vertebral body is named “spondyloptosis.”
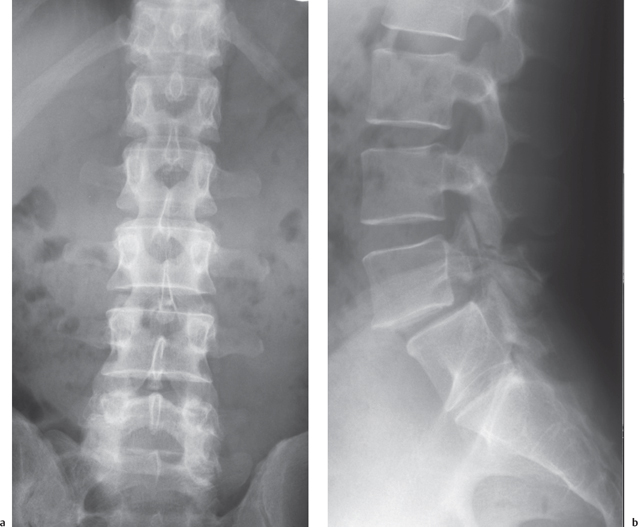
Fig. 9.1.1 Spondylolysis and spondylolisthesis with a concomitant transitional vertebra.
Spondylolisthesis occurs in the preadolescent and is found in up to 50% of athletes with persistent back pain. Symptoms may not occur until later in life. In a longitudinal study by Fredrickson et al three-quarters of all individuals with spondylolysis had an identifiable pars defect on plain films by age 6, and approximately 75% of these patients had evidence of a slip at that time.1 Further progression of the slip in adulthood is rare.14
Indications for Imaging
Imaging investigations should be performed if back pain more persistent than simple myalgia is observed. The typical pain associated with spondylolysis is dull and occasionally unilateral, sometimes radiating into the buttocks or even the groin.15 The pain increases during exercise with hyperextension and rotational movements. Hyperlordosis, stiffness of the hip joints, and pain or cramps in the hamstring muscles or in the erector spinae may be associated findings. Signs of neural impingement with L5 root compression or in some rare cases with cauda equina syndrome may indicate severe spondylolisthesis. A history of trauma is not observed, but subclinical backache for a longer period of time is typical. Today, the extreme form of slipped vertebra with heart-shaped buttocks, high iliac crests, and a relatively short torso is rarely observed.
Predisposing factors include history of a first-degree relative with a slipped vertebra, rare callus formation, and a young age of onset.16
The primary imaging investigation is done with conventional radiographs. More specialized investigation includes magnetic resonance imaging (MRI), computed tomography (CT), and scintigraphy. Following European referral criteria these modalities are classified with an evidence level of “C” on a scale A-C.17 Many cases of spondylolysis identified by some of the newer imaging techniques are not noted concurrently on conventional radiograms. MRI is performed to detect associated disk prolapse and to delineate the extent of neural impingement. CT is the modality of choice to confirm or rule out spondylolysis by displaying the morphology of the vertebral arch in great detail. Nuclear medicine studies should be applied if the results of other imaging modalities are negative, however, generally they are of lesser importance considering the modern multi-planar capabilities of CT and MRI.
Follow-up imaging studies may be indicated for the athlete if there is an urgent requirement for a return to competition. In general, nonoperative treatment of spondylolysis is reported to result in successful pain relief in approximately 80% of athletes, independent of radiographic evidence of healing of the defect.5 As it is difficult in children and preadolescents to predict the risk and the extent of vertebral slipping, radiological monitoring may be indicated in patients involved in sporting activities that are associated with a higher risk of spondylolysis, especially in throwing sports, gymnastics, and rowing (Table 9.1.1).4,7,18
Investigation Techniques
Radiography
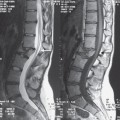
Conventional radiographs should be exposed in the lateral and antero-posterior direction and in many cases an interruption of the pars interarticularis can be detected on the lateral views. As there is an overlap of the right and left pars, oblique views with 45° angulation may be helpful. Amato et al found that lateral oblique views and a lumbosacral lateral spot view (Fig. 9.1.2a) are superior to anteroposterior and lateral views of the lumbar spine.19 Flexion and extension views of the lumbar spine are helpful to measure the extent of hypermobility or instability in the spondylolytic and in the neighboring segments (Figs. 9.1.2, 9.1.3). Correct display of the vertebral arches is, however, not always easy because of the nontomographical character of plain films and especially in patients with associated scoliosis where an interruption of the isthmus may be obscured (Fig. 9.1.4). Saifuddin et al analyzed 69 spondylolytic defects with CT and found a wide variation between individuals with only 32% of the lesions aligned within 15° of the 45° lateral oblique plane.20 Unfortunately, no internationally accepted labeling of the angulated views with respect to the left and right side exists; labels may refer to the side of the patient’s body as well as to the beam direction.
Fluoroscopy may be of help in selected cases to observe atypical movement patterns; however, considering radiation protection issues there is no justification in routine diagnosis.
Computed Tomography
CT with its multi-planar capabilities is the modality of choice to document spondylolysis (Fig. 9.1.5). Images reconstructed in a sagittally angulated plain parallel to the course of the pars interarticularis are the most useful for displaying not only an interruption of the pars but also its length and shape. Moreover, repair mechanisms and associated abnormalities of the facet joints or intervertebral foramina can be detected with CT. Furthermore, CT allows us to define the exact angles of spondylolysis as well as of the slipping of a vertebra. Investigations should be performed with a multi-row multidetector unit to obtain images with a high resolution in all planes. Where single-row machines are only available, the technique of reverse angle gantry tilt may be applied with images oriented perpendicular to the vertebral arch.
Magnetic Resonance Imaging
MRI is useful for detecting osseous clefts, bone marrow edema, or fat marrow conversion due to mechanical overload. It is of specific importance for assessing the spinal capacity and causes of neural impingement. With a standardized technique of investigation including sagittal T1W and T2W or STIR sequences a gap of the pars interarticularis is more easily detected than with axial slices (Fig. 9.1.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree