Why Classify?
Fracture classification schemes have commonly been used in surgical practice. Most surgeons consider them necessary tools as a conceptual framework for diagnosis and treatment. Furthermore, these schemes are used as communication systems with regard to the relative severity of the injuries and the potential results of different treatment options. However, these schemes have been gradually introduced into the field without a proper discussion of their meanings and consequences. During the last decade the usefulness of these schemes has been a matter of intense debate. In a controversial editorial inthe Journal of Bone and Joint Surgery in 1993, Albert Burstein asked in conjunction with two other articles in the same issue: “Fracture classification systems: Dothey work and are they useful?”3 As a scientist outside the field of surgical practice, he observed:
“Fracture classification systems are, in effect, tools. The purpose of the tool is to help the surgeon to choose an appropriate method of treatment for each and every fracture occurring in a particular anatomical region. The classification tool should not only suggest a method of treatment; it should also provide the surgeon with a reasonably precise estimation of the outcome of that treatment. Generally, we think of an orthopedic tool as working if it produces the same desired results, time after time, in the hands of anyone who is likely to use it. Thus, each practitioner should produce the same classification every time the same patient data are reviewed (intraobserver reliability or repeatability), and different practitioners should agree on the classification of the data for a particular patient (interobserver reliability) . . . To use this tool before its workability has been proved is inappropriate… Any classification scheme, be it nominal, ordinal, or scalar, should be proved to be a workable tool before it is used in a discriminatory or predictive manner…Once the tool has been shown to be functional, the next step in the process is to prove that it is useful. This step requires clinical studies in which the classification has been used as the basis for the choice of treatment.”
The discussion of the value of such classification schemes began as a result of an evaluation of the Neer classification system for proximal humerus fractures, which proved to be a very unreliable scheme despite its widespread acceptance and use since 1970! If the orthopedic community has failed in the proper evaluation of something as relatively simple as fractures of the proximal humerus, what are clinicians to think of classification schemes for complex injuries of a compound structure such as the spine?
Classification of Thoracolumbar Spine Fractures
There has indeed been a great deal of controversy concerning the classification of fractures of the thoracolumbar spine. A plausible classification of these injuries was only possible after reliable imaging of the spine with proper radiographs became available on a large scale. After the first attempts at classification by Böhler in 1929, many authors recognized the difficulty of a comprehensive classification.2 The main difficulty lies in the fact that: (a) unlike the fractures of long bones, the pattern of spine fractures may be progressive, evolving into an increasing deformity even after apparent union of the fractured spine; and (b) fractures of the spine represent complex injuries of a structure composed of parts each with a different susceptibility to injury and different healing potentials. Böhler recognized five types of injury:
- Compression fracture with vertebral body injury.
- Flexion-distraction injuries with anterior injury due to compression fracture and posterior injury due to distraction.
- Extension fractures with injury to the anterior and posterior longitudinal ligaments and posterior arch injuries.
- Shear fractures.
- Torsion injuries.
The following efforts of Watson-Jones and Nicoll were more directed towards defining instability patterns so that the classification could be used as a predictive tool and a guide for treatment.29,18 Watson-Jones was the first who introduced the concept of “instability.” He recognized the importance of ligamentous injuries for the stability of the spinal column. Nicoll,18 on the basis of a study of 166 fractures and fracture-dislocations in 152 miners during the period 1939-1945, classified the fractures on an anatomical basis into four main types:
- Anterior wedge fracture. Lateral wedge fracture.
- Fracture-dislocation.
- Isolated fracture of the neural arch.
Recognizing the role of different structures in the generation of different patterns of fractures, he pointed out four different structures involved: the vertebral body, the disk, the intervertebral joints, and the interspinous ligament. He called the disk the fulcrum of the motion segment. He also referred to the importance of differentiating between stable and unstable varieties and the danger of increasing neurology or increasing deformity of unstable injuries.
Holdsworth tried to capture the problem of stability in the columnar spine.8 He tried to abstract the vertebral stability with an architectonic two-column concept (Fig. 4.1a). This concept has been influential ever since. His anterior column consisted of the vertebral bodies and the intervertebral disk. He called the posterior column the “posterior ligament complex” consisting of the facet joints, the intraspinous and supraspinous ligaments, and the ligamenta flava. In his theory the integrity of this posterior column is crucial for the stability of the spine. He called all injury patterns with an intact posterior column stable. He classified injuries into six groups:
- Anterior wedge compression.
- Dislocation.
- Fracture/dislocation by rotation.
- Extension injury.
- Burst fractures.
- Shear fractures.
He was the first to introduce the concept of the “burst fracture,” which he described as a result of compression force rupturing one of the endplates and forcing the disk into the body of the vertebra causing it to burst out. Although the concept of Holdsworth remained influential throughout the 1960s and 1970s, it was severely criticized from the outset. Kelly and Whitesides demonstrated that bony fragments retropulsed from the body in burst fractures, which gave them a high potential for instability.9 Roberts and Curtiss were the first to point to the late progression of deformities in the burst fractures, with possible neurological consequences.26 Roy-Camille and Demeulenaer emphasized in that context the role of their segment moyen, formed by the posterior part of the disk, annulus fibrosus, and the posterior longitudinal ligament, together with the pedicles and the facet joints.27 Louis tried to elaborate the spinal column concept with the introduction of a three-column architecture of the spine.14
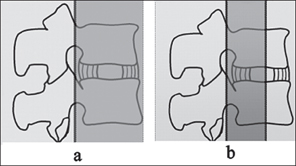
Fig. 4.1 a The two columns of Holdsworth. b The three columns of Denis.
The Three-Column CT Era
The introduction of computed tomography (CT) in the second half of the 1970s for spinal fractures provided new insight into the fine structural details of these injuries. The possibility of imaging the spine in transverse sections drew attention to the comminution of fractures and canal encroachment, which would not even have been suspected with traditional radiographs. These CT findings had a large impact on the thinking concerning a new classification system, based on the more accurate description of the extent and place of injury now possible. McAfee et al, in their extensive studies showed the indispensability of computed tomography for an exact description of the injuries.16 Efforts in this direction in the early 1980s culminated in the three-column concept of Denis, which has become the dominant classification system (Fig. 4.1b).4 Denis classified fractures into four types (Fig. 4.2):
- Compression fractures: Failure under compression of the anterior column. The middle column is intact.
- Burst fractures: Failure of anterior and middle columns under axial loads.
- Seat-belt injuries : Failure of both the posterior and middle columns under tension forces generated by flexion and distraction.
- Fracture dislocations: Failure of all columns under compression, tension, rotation or shear.
Denis also introduced the concept of different degrees of instability:
- Instability of the first degree is a mechanical instability with risk of progressive kyphosis.
- Instability of the second degree is a neurological instability.
- Instability of the third degree is both a mechanical and a neurological instability. Fracture/dislocations and unstable burst fractures are in this category.
Although this classification was a refinement of the understanding of the nature of these injuries, it was amenable to many simplifications and led to some confusion that still exists. As usual this scheme was also introduced without a proper analysis of reproducibility or predictive power. Although Denis emphasized that his columns are formed by osseous and nonosseous structures, no attempt has been made to further the diagnosis of nonosseous injuries. The three-column concept was reduced to what is visible with transverse CT images. It has been simplified and reduced to a simple rule of thumb, which states that any injury to two of the three columns, as seen on CT (bony injury), make the spine unstable. Further, an intact middle column has been seen as a guarantee of stability, although Denis mentioned some of these lesions as being first-degree unstable. Also the differentiation between first, second, and third degree instability has been lost, leading to a vague, poorly defined and alarming instability concept, which has remained dominant during the past two decades.
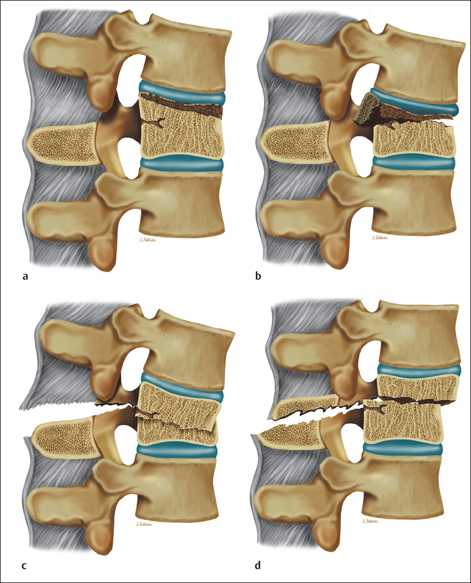
Fig. 4.2 Denis classification. a Compression; b Burst; c Seat-belt; d Fracture-dislocation.
Despite its widespread acceptance there has been criticism of the Denis classification and attempts have been made to modify it from the beginning. Ferguson and Allen called the columns a poor semantic choice because these tissues do not anatomically or biomechanically resemble a column.6 They argued: “the term, although appealing for its verbal ring, is anatomically and biomechanically incorrect.” They suggested a mechanistic classification instead, according to a presumed mechanism of injury deduced from the patterns of tissue failure. McAfee et al suggested a division of the burst fractures as stable and unstable.16 Finally, Farcy et al modified the Denis classification to include both bone and soft tissue injuries in each of the three columns of a motion segment.5 They developed a scheme of instability graded from 1 to 6, with injuries greater than or equal to grade 3 being unstable. But they also failed to develop diagnostic means to make the distinction between bone and soft tissue injuries.
The Load-Sharing Classification
Dissatisfaction with these vague concepts led to attempts to define some specific questions disturbing the practitioners. One of the most remarkable attempts was the load-sharing classification proposed by McCormak et al in 1994.17 This scheme is a specific elaboration of the Denis system with a specific problem in mind. The authors were disturbed by the high rate of failure of posterior fixation in their patients with some types of fractures, and searched for factors predictive of this failure. Their conclusion was that the degree of comminution of the vertebral body together with the apposition of fragments and the degree of deformity correction were factors predictive of the failure of posterior fixation. The authors developed a system of rating as follows:
- A: Comminution of the vertebral body: little (1), more (2), gross (3 points).
- b: Apposition of fragments: minimal (1), spread (2), wide (3 points).
- c: Deformity correction: little (1), more (2), most (3 points).
They observed that, in their series of 28 patients, all 10 cases with a screw fracture had a sum of 7 or more points, and no patient with a sum of 6 or less points had a screw fracture.
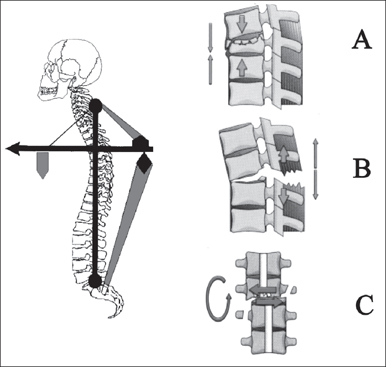
Fig. 4.3 Comprehensive classification (AO) is based on the crane model. Type A: caused predominantly by compression; Type B: transverse disruption; Type C: rotation or translation.
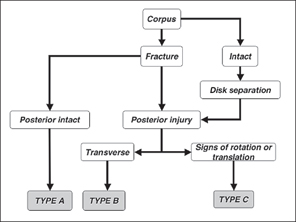
Fig. 4.4 Flow diagram for determining the type level of the AO classification.
The AO (Comprehensive) Classification
The classification scheme of the AO group is a culmination of efforts of many practitioners over a 10-year period.15 This scheme is primarily based upon the pathomorphological characteristics of the injuries and is based on the mechanical model of a crane. Three main categories with a common injury pattern, classified as types, are formed (Fig. 4.3):
Type A: Vertebral body compression.
Type B: Anterior and posterior element injury with distraction. Type C: Anterior and posterior element injury with rotation or translation.
The authors abandoned the three-column concept and went back to the two-column concept of Holdsworth, i. e., an anterior column consisting of the vertebral body and the disk, and a posterior complex. They also depended on the mechanistic classification of Ferguson and Allen for identification of common denominators of the types: type A injuries represent compression forces, type B tensile forces, and type C axial torque or shear (Fig. 4.4). A biomechanical study showed a good relation between this type categorization of the scheme and the resulting mechanical instability in a cadaveric fracture model.11 For further subclassification, the authors used the common AO 3-3-3 grid. Subclassification of the type B and C injuries essentially follows the subclassification of type A injuries (Fig. 4.5). Type A injuries: Injuries caused mainly by axial compression causing predominantly injury to the anterior elements (vertebral body and disk). There is no or insignificant injury to the tension band function of the posterior column. The subclasses of type A:
- A1: Impaction fractures. The deformation of the vertebral body is due to compression (plastic deformation) of the cancellous bone rather than fragmentation.
- A1.1: Endplate impaction with minor wedging up to 5°.
- A1.2: Wedge impaction with loss of anterior vertebral height resulting in an angulation of more than 5°.
- A1.3: Vertebral body collapse. Symmetrical loss of vertebral body such as observed in osteoporotic spines without significant extrusion of fragments.
- A2: Split fractures. The vertebral body is split in the coronal or sagittal plane with dislocation of fragments and filling of the defect with disk material.
- A2.1: Sagittal split fractures.
- A2.2: Coronal split fractures.
- A2.3: Pincer fracture, in which the central part of the body is crushed and filled with disk material.
- A3: Burst fractures

Stay updated, free articles. Join our Telegram channel
- A2: Split fractures. The vertebral body is split in the coronal or sagittal plane with dislocation of fragments and filling of the defect with disk material.

Full access? Get Clinical Tree