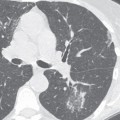
CASE 100 40-year-old man involved in an all-terrain vehicle (ATV) incident with a clinical concern of possible hemomediastinum and acute aortic injury Contrast-enhanced axial (Fig. 100.1A) and sagittal oblique (Fig. 100.1B) chest CTA (mediastinal window) demonstrates the typical location and appearance of an acute post-traumatic aortic pseudoaneurysm. The pseudoaneurysm projects from the anteromedial aorta at the LMSB and distal to the left subclavian artery. Note the peribranch vessel and para-aortic hemomediastinum. Acute Post-Traumatic Aortic Injury (ATAI) with Pseudoaneurysm None ATAI from blunt trauma is a substantial cause of morbidity and mortality, occurring in approximately 0.5–2% of all non-lethal motor vehicle collisions (MVCs) and 10–20% of all high-speed deceleration fatalities. MDCT has emerged as the definitive screening modality for both diagnosis and exclusion of ATAI and great vessel injury without the need for conventional aortography or transesophageal echosonography. The latter are now typically only used in the infrequent setting of equivocal MDCT findings. In fact, the increased use of MDCT has led to the recognition of numerous vascular variants that may mimic acute injuries (see Case 101) as well as the diagnosis of more subtle vascular injuries, which heretofore likely went undiagnosed, often with little or no surrounding peribranch vessel or para-aortic hematoma. The increasing use of non-surgical therapies (e.g., blood pressure augmentation, endovascular stents) for both temporary and definitive management necessitates accurate localization and characterization of these otherwise lethal injuries. Thus, it is imperative that the radiologist specifically describe the: Fig. 100.1 • Nature of ATAI (e.g., pseudoaneurysm, intimal flap, dissection, luminal thrombosis, coarctation) • Diameter of the aorta or affected branch vessel immediately proximal and distal to the injury • Length of the injury along its vascular axis • Relationship between the injury and the nearest arterial branch vessel • Congenital vascular variations in anatomy (e.g., aberrant right subclavian artery, left vertebral artery originating off the aortic arch, right-sided aortic arch with aberrant left subclavian artery, vascular slings, etc.) and their relationship to the injury ATAI may occur anywhere along the thoracic aorta: • Aortic isthmus—within 2 cm of left subclavian artery origin: most common site • Aortic root and ascending aorta—5–14% of autopsies with aortic injuries; rarely seen at MDCT presumably because of its lethal nature • Aortic arch and branch vessel— less common. Isolated branch vessel injuries are more common than aortic arch injuries (<4% of blunt chest trauma victims), but may occur in combination with ATAI in 0–45% of patients. Brachiocephalic and common carotid arteries are the most commonly involved vessels (66–90%). • Mid and distal descending thoracic aorta— 1–12% of autopsies with aortic injuries. These injuries can be associated with diaphragm injury (10% cases) and adjacent thoracic spine compression fractures. • Minimal aortic injuries— only affect the intima and are estimated to occur in 10% of patients with ATAI; encountered with increasing frequency. Nearly half of cases show no abnormality at conventional angiography. The exact mechanism of injury is not precisely known. Proposed mechanisms include shearing forces, rapid deceleration, hydrostatic forces, and the osseous pinch. Most ATAI (75–80%) results from violent deceleration, most commonly a high-speed MVC, especially head-on (50%) and lateral side-impact collisions (73%). Interestingly, various occupant restraint devices (excluding side airbags) are largely ineffective in curtailing ATAI in lateral side-impact collisions. Other potential causes include falls from height, pedestrian-automobile collisions, and crush injuries. Direct injury of the aorta may also occur due to penetration from rib and thoracic spine fractures. The nature and extent of ATAI vary widely, ranging from intimal hemorrhage to complete transection. Most injuries result from transverse tears and can be segmental (55%) or circumferential (45%). Tears may also be partial (65%) or transmural (35%). Spiral and irregular tears are rare. Partial lacerations involve the inner two walls of the aorta, resulting in a contained rupture. The adventitia may be injured in up to 40% of cases. These latter injuries are almost universally fatal because of rapid exsanguination. Clinical signs and symptoms are nonspecific and insensitive for the diagnosis and exclusion of ATAI. Most patients have no clinical signs of aortic injury until they suddenly become hemodynamically unstable. Symptoms induced by stretching of the mediastinal connective tissues by hemomediastinum include interscapular pain, dyspnea, and hoarseness. Clinical signs of ATAI are absent in one-third of patients but when present include “pseudocoarctation syndrome” (i.e., upper extremity hypertension and lower extremity hypotension with diminished femoral pulses), external chest wall injuries, paraplegia, systolic murmur, and initial chest tube output >750 mL of blood. There are, however, seven criteria that are useful predictors in the risk assessment of potential ATAI. The more criteria that are met, the greater the probability of ATAI (e.g., trauma patients with ≥4 criteria: 30% chance of an ATAI). These criteria include: • Age >50 years • Unrestrained vehicle occupant • Systolic blood pressure <90 mm Hg • Thoracic injury (e.g., rib fracture, pneumothorax, lung contusion, or laceration) • Abdomino-pelvic injury requiring emergent laparotomy or with fractures of the lumbar spine and pelvis • Long bone fractures (e.g., humerus, radius, ulna, femur, tibia, or fibula) • Major head injury (e.g., skull fracture, intracranial hematoma, unconsciousness at time of evaluation, or intraparenchymal hemorrhage) Exclusion of life-threatening injuries requiring immediate treatment (e.g., tension pneumothorax, large hemothorax, malpositioned life support devices) Indirect evidence of hemomediastinum and potential ATAI • Abnormal aortic contour or poor definition of transverse aorta (Fig. 100.2) • Superior mediastinal widening at transverse aorta level >8 cm (Fig. 100.2) • Superior mediastinum ≥25% of the width of the thorax (Fig. 100.2) • Opacification of aorticopulmonary window (Fig. 100.2) • Rightward deviation of trachea and/or endotracheal tube (Fig. 100.2) • Nasogastric tube deviation to the right of the T4 spinous process • Thickened or poorly defined left paraspinal line • Poor definition of descending thoracic aorta interface • Widened right paratracheal stripe (>5 mm) (Fig. 100.2) • Downward displacement of left mainstem bronchus >40° from the horizontal • Left hemothorax and/or left apical cap • Fractures of first and second ribs (Fig. 100.2) • May be normal or deceptively underwhelming in up to 7% of proven ATAI cases • Concomitant thoracic injuries not uncommon (e.g., pulmonary contusion, pneumothorax, hemothorax, diaphragmatic injury) CT imaging features of aortic and great vessel injury are categorized as direct or indirect. The most specific direct signs are intimal flap and luminal thrombus or debris (100%) whereas irregular aortic contour or pseudoaneurysm is the most sensitive (100%). Fig. 100.2 AP trauma bay chest X-ray of a 40-year-old unrestrained driver involved in a high-speed MVC shows indirect evidence of hemomediastinum and potential ATAI, subsequently proven on MDCT. There is poor delineation of the aortic arch and opacification of the aorticopulmonary window. The superior mediastinum is widened with rightward tracheal displacement. The right paratracheal stripe is thickened. Note the displaced right clavicle fracture, fractures of bilateral first and second ribs, and additional left-sided ribs. • Pseudoaneurysm
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background

Etiology
Clinical Findings
Imaging Findings
Chest Radiography
Primary Role
Secondary Role
MDCT

Direct Signs
 Well-defined rounded bulge with irregular margins arising from anterior or anteromedial aspect of proximal descending thoracic aorta at LMSB and proximal LPA level (Figs. 100.1A, 100.1B, 100.3, 100.4, 100.5)
Well-defined rounded bulge with irregular margins arising from anterior or anteromedial aspect of proximal descending thoracic aorta at LMSB and proximal LPA level (Figs. 100.1A, 100.1B, 100.3, 100.4, 100.5)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree