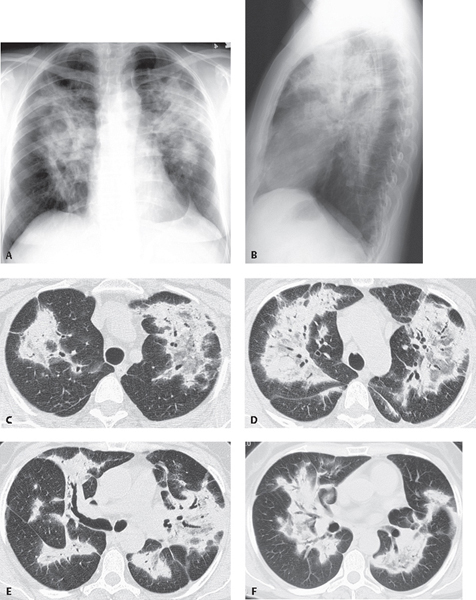
CASE 110 56-year-old woman treated for presumed community-acquired pneumonia for the last two months without improvement complains of dyspnea, persistent non-productive cough, and recent 8 pound weight loss. PA (Fig. 110.1A) and lateral (Fig. 110.1B) chest radiographs demonstrate bilateral perihilar and upper lobe non-segmental consolidations. HRCT (Figs. 110.1C, 110.1D, 110.1E, 110.1F) reveals patchy bilateral consolidations and ground glass opacities with a peribronchial distribution. Pleural tails extend out from the opacities to the chest wall. Bronchial wall thickening and dilatation can be seen. Cryptogenic Organizing Pneumonia (COP) • Acute Interstitial Pneumonia (AIP) • Non-Specific Interstitial Pneumonia (NSIP) • Chronic Eosinophilic Pneumonia • Sarcoidosis • Chronic Aspiration • Diffuse Alveolar Damage (DAD) • Desquamative Interstitial Pneumonia (DIP) Organizing pneumonia (OP) is histologically characterized by intraluminal plugs of granulation tissue within alveolar ducts and surrounding alveoli, with associated chronic inflammation in the surrounding lung. Because granulation tissue polyps are also present in the respiratory bronchioles, OP is also called bronchiolitis obliterans with organizing pneumonia (BOOP). Because the clinical, functional, radiologic, and HRCT features of this interstitial lung disease are primarily the result of an organizing pneumonia, the American Thoracic Society/European Respiratory Multidisciplinary Consensus Classification Committee has proposed cryptogenic organizing pneumonia (COP) as an alternative designation in idiopathic cases. The exact incidence and prevalence are unknown. The diagnosis is usually made on open lung biopsy. Most cases of OP are idiopathic (COP). Numerous conditions may be associated with an OP- or BOOP-like reaction, including but not limited to collagen vascular diseases, pulmonary infection (e.g., HIV, Pneumocystis pneumonia, Mycoplasma pneumonia), inflammatory bowel disease, hypersensitivity pneumonitis, drug toxicity, vasculitides (e.g., Wegener granulomatosis), intravenous drug abuse (e.g., cocaine), drug reactions, toxic fume inhalation, and lung and chest wall irradiation. Fig. 110.1
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine



