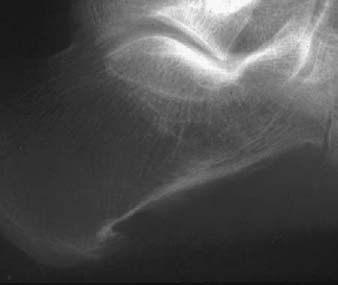
CASE 113 Anthony G. Ryan and Peter L. Munk A 25-year-old man presented with an acute exacerbation of a recurrently painful heel. Figure 113A A lateral radiograph of the heel (Fig. 113A) shows a calcaneal spur and a periosteal reaction along the inferior aspect of the calcaneus. Reactive arthritis (Reiter’s disease). The seronegative spondyloarthropathies consist of ankylosing spondylitis, psoriatic arthritis, reactive arthritis (Reiter’s syndrome), enteropathic spondylitis, and undifferentiated spondyloarthropathy, all of which share common clinical and radiographic features with characteristic involvement of the sacroiliac joints, the spine, and the peripheral joints. All of the above typically affect young adults. If a seronegative spondyloarthropathy presents in patients under the age of 16, it is referred to as “juvenile.” Previously known as Reiter’s syndrome, the condition is now more correctly called reactive arthritis and is clearly identified as one of the spondyloarthritis group of diseases. When the typical arthritis is accompanied by urethritis and conjunctivitis, the term Reiter’s syndrome still properly applies, with circinate balanitis (30%), buccal ulcerations, and a dermatitis (keratogenic blennorrhagia) as frequent additional findings. It appears that at least two factors are necessary for the development of reactive arthritis: an initiating infectious agent and a genetic predisposition. The infectious agent is most commonly a gram-negative bacterium with lipopolysaccharide as an integral component of its outer membrane, contracted via either a sexually transmitted urethritis or a dysentery. Chlamydia has recently been identified as a potential organism. The prevalence of the human leukocyte antigen (HLA) B27 in Reiter’s arthritis is quoted as between 63 and 93%. Conversely, the prevalence of spondyloarthropathies in a given population correlates directly with the prevalence of the HLA-B27 antigen. The presence of HLA-B27 strongly predisposes individuals to the development of reactive arthritis after an enteric or genitourinary infection. The disease is more severe in patients who are HLA-positive and tends to pursue a more aggressive and chronically relapsing course. HLA-B27 appears to modulate the interaction between reactive arthritis–triggering bacteria and immune cells by a mechanism unrelated to the antigen presentation function of HLA-B27. Molecular mimicry, the phenomenon of protein products from dissimilar genes sharing similar structures eliciting an immune response to both self and microbial proteins, has been proposed as a potential mechanism by which infections trigger autoimmune diseases. The molecules identified to demonstrate most consistent mimicry are chlamydial heat shock proteins 60, the deoxyribonucleic acid (DNA) primase of Chlamydia trachomatis, and chlamydial OmcB proteins, thus potentially implicating this organism in the initiation and maintenance of reactive arthritis. In addition, elevated levels of tumor necrosis factor-α (TNF-α) have been identified in the synovium of patients with reactive and undifferentiated arthritis, implicating TNF-α in the pathogenesis of these disorders. Patients (the vast majority male, in their third and fourth decades) typically present with a triad of symptoms, namely, painful joints, painful eyes, and painful urination, reflecting underlying arthritis, conjunctivitis, and urethritis. There is a frequent history of a recent infection, either sexually transmitted or a diarrheal illness (Shigella, Salmonella, Yersinia, or enteric Campylobacter). The arthritis is typically mono- or pauciarticular, asymmetric, and involves lower extremity peripheral joints predominantly. Enthesitis is the term given to inflammation at the site of ligamentous attachment to bone and is a frequent attendant of reactive arthritis. Reflecting this, heel pain is present in 26 to 50% of cases and may affect the region of the Achilles’ insertion or the plantar surface of the calcaneus, which may be visibly or palpably swollen on examination. Dactylitis and tenosynovitis are frequently present early on in as many as 17% of patients. Less commonly, patients may present with inflammatory spinal pain, sacroiliitis, chest wall pain, lesions of the lung apices, and aortic incompetence together with conduction disturbances. All of these may also occur in isolation. When the arthritis is isolated and oligoarticular, particularly in the presence of a urethritis, it must be differentiated from gonococcal arthritis by aspiration. In reactive arthritis, joint aspiration reveals a turbid yellow fluid.
Reactive Arthritis (Reiter’s Disease)
Clinical Presentation
Radiologic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Etiology
Pathophysiology
Clinical Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


