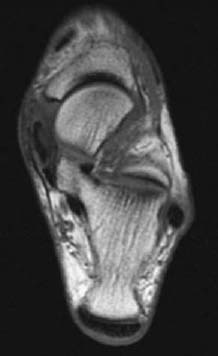
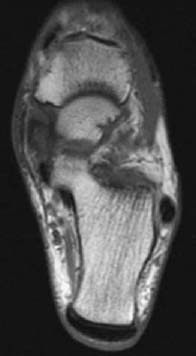
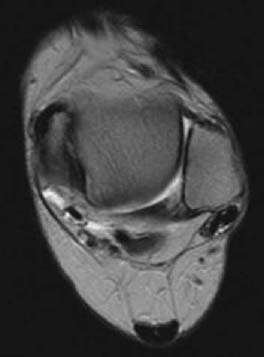
CASE 22 Anthony G. Ryan and Peter L. Munk and A middle-aged diabetic woman presented with pain and swelling on the medial aspect of her ankle and progressive flatfoot. Figure 22A Figure 22B Figure 22C An axial T1-weighted image (Fig. 22A) shows internal signal heterogeneity within the tibialis posterior tendon and intermediate signal intensity material surrounding the tendon within the tendon sheath. There is focal tendon discontinuity evident medially. Low signal intensity is visible within the overlying subcutaneous fat. An axial T1-weighted image (Fig. 22B) more caudad Fig. 22A shows the same findings with more extensive tendon disruption visible medially, the intermediate signal intensity within the tendon occupying ~80% of its cross-sectional diameter. An axial T2-weighted image (Fig. 22C) at a level more cephalad Figs. 22A, 22B shows the “empty sheath” sign, in which no tendon is visible within the tibialis posterior tendon sheath, seen anteromedial to the normal tendon of the flexor digitorum. Torn tibialis posterior tendon None. The tibialis posterior muscle takes its origin from the posterior surface of the intraosseous membrane, the posterior shaft of the tibia, and the upper shaft of the fibula. Its tendon inserts onto the navicular tuberosity with additional slips to the sustentaculum tali, the cuneiforms, the cuboid bone, and the bases of the second, third, and fourth metatarsals. The tibialis posterior tendon runs in a groove behind the medial malleolus deep to the flexor retinaculum and anterior to the tendon of the flexor digitorum longus. The tendon lies superficial to the deltoid ligament and deep to the calcaneonavicular ligament. Its main actions are plantar flexion, adduction, and inversion of the foot, while also serving as a plantar arch support. Posterior tibial tendinitis and rupture are common occurrences in association with rheumatoid arthritis. Women in their fifth or sixth decades, especially if diabetic, are most at risk. Other clinical associations include The most commonly torn of the flexor tendons, the tibialis posterior is the second-most commonly torn ankle tendon after the Achilles’ tendon. The loss of the tibialis posterior tendon itself leads to minimal loss of plantar flexion; however, its loss as an arch support leads to a cascade of hindfoot dysfunction. Acute complete tibial tendon rupture leads to an acute flatfoot. If a partial tear goes untreated, over time it is likely to result in a progressive flatfoot. Longitudinal arch collapse produces secondary heel valgus. Hindfoot valgus collapses the sinus tarsi, which, in turn, is a further source of chronic hindfoot pain. Conversely, if there are problems in the arch or plantar fascia, this can adversely affect the posterior tibial tendon, leading to tendinitis and/or rupture. The typical patient is a middle-aged diabetic woman presenting with medial hindfoot pain, swelling, and progressive loss of function secondary to acquired flatfoot, including difficulty standing on “tiptoes.” If an acute injury occurs, pain with an accompanying tender swelling on the medial aspect of the foot is the typical presentation, with reduced adduction that is painful against resistance. In assessing a patient’s ability to stand on his or her toes, the heel of a patient with an intact posterior tibial tendon will rotate inward; if the tendon is torn, the heel will not rotate inward and may in fact turn out. If a tear has been progressive or present for some time, hindfoot valgus, midfoot abduction at the midtarsal joints, and forefoot pronation may all be evident. Pain on the lateral aspect of the foot may become superimposed. Rarely, the tibialis posterior tendon may be involved in fractures of the medial malleolus. The staging is based on a combination of clinical and MRI findings: Stage 1 Medial pain and edema; normal MRI Stage 2 Increasing pain; “too many toes” sign (this is present when the examining physician sees “too many toes” when looking at the patient from behind; that is, the foot is pointing more laterally than normal); the deformity is reducible; partial tears evident on MRI
Posterior Tibialis Tendon Tear
Clinical Presentation
Radiologic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Etiology
Pathophysiology
Clinical Findings
Stages of Disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


