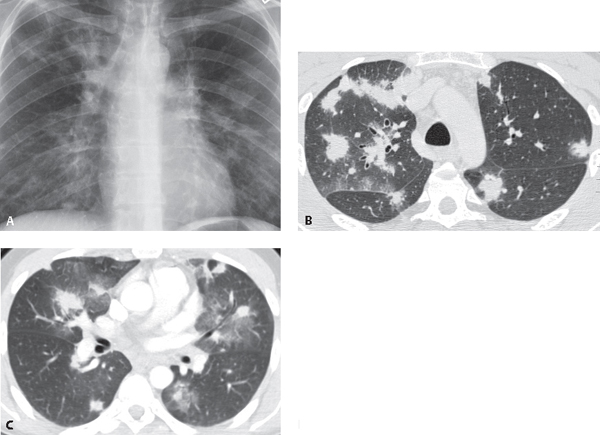
CASE 118 32-year-old man with AIDS, cough, and dyspnea Coned-down PA chest radiograph (Fig. 118.1A) demonstrates bilateral, symmetric, poorly defined nodular opacities measuring up to 3.0 cm in diameter with a predominantly perihilar distribution. The bronchovascular bundles appear thickened. Chest CT (lung window) (Figs. 118.1B, 118.1C) from another patient with a similar history reveals ill-defined and irregular or “flame-shaped” nodular opacities in a predominantly perihilar and peribronchovascular bundle distribution. Kaposi sarcoma • Lymphoma • Metastatic Disease Fig. 118.1 • Pneumocystis jiroveci Pneumonia • Mycobacterium tuberculosis Infection; Nontuberculous Mycobacterial Infection • Other Bacterial and Fungal Pulmonary Infections Kaposi sarcoma (KS) is a multicentric malignant neoplasm that originates from vascular and lymphatic endothelial cells. It occurs in 15–20% of HIV-infected male homosexuals, and in 1–3% of other HIV-infected individuals. The incidence of KS as an AIDS-defining illness has been decreasing over the last decade and is distinctly reduced in HIV-infected patients receiving antiretroviral therapy (ART). Cutaneous or visceral KS usually precedes lung involvement. There seems to be an association between infection with human herpesvirus 8 DNA and the development of KS. The HIV regulatory protein (transactivator target, TAT), important for viral replication, is also likely responsible for the proliferation of KS cells.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





