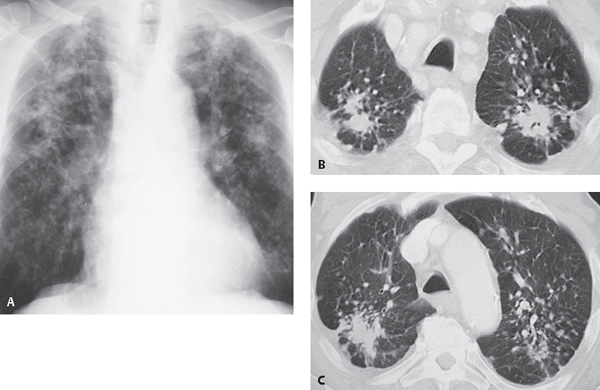
CASE 124 80-year-old man with increasing dyspnea Coned-down PA chest radiograph (Fig. 124.1A) demonstrates small bilateral well-defined nodules (1–6 mm) and coalescent nodular opacities (>1 cm) that predominantly involve the upper and mid lung zones. There is bilateral upper lobe parenchymal distortion. Chest CT (lung window) (Figs. 124.1B, 124.1C) shows bilateral upper lobe spiculated masses, small well-defined nodules, and larger irregular opacities in the dorsal aspect of both upper lobes. Silicosis; complicated • Coal Worker’s Pneumoconiosis • Sarcoidosis • Tuberculosis Fig. 124.1 The term pneumoconiosis refers to the accumulation of dust in the lungs and the tissue reaction to its presence. The most frequently encountered inorganic dusts are silica, asbestos, coal, iron, and beryllium, and accumulation occurs most commonly through inhalation during occupational exposure. Silicosis is a chronic occupational lung disease characterized by pulmonary nodules that may coalesce to form lung masses and may progress to pulmonary fibrosis in patients with a history of inhalation of crystalline free silica. Criteria for the diagnosis of silicosis are (1) appropriate exposure history, (2) radiologic findings consistent with silicosis, and (3) absence of other diseases to explain the radiologic findings. Simple silicosis refers to cases in which small silicotic nodules (<10 mm) are present and larger, conglomerate opacities are not demonstrated. It occurs in 10–20% of exposed workers. Complicated silicosis refers to progression of disease with larger nodules which coalesce to form conglomerate masses (>1 cm) in a process called progressive massive fibrosis (PMF). Complicated silicosis occurs in 1–2% of exposed workers. The most important factors in the development of silicosis are the intensity and duration of exposure to silica. The most abundant source of crystalline silica is quartz, and exposure is most common in rock mining, quarrying, stone cutting, sandblasting, and ceramics. Pathogenetic factors include the size, shape, and concentration of dust particles, duration of exposure, and individual patient susceptibility. Relatively low levels of exposure result in classic chronic silicosis. Silica particles are ingested by alveolar macrophages; when the macrophages eventually break down, enzymes and other products are released and the silica particles become available for re-ingestion by other macrophages. This repeating cycle explains the progression of silicosis, despite cessation of exposure to silica dust. A rare, generalized form of alveolar proteinosis (silicoproteinosis; syn. acute silicosis) may occur in individuals who experience a massive exposure to silica dust in enclosed spaces (e.g., sandblasters). In those individuals, the normal clearing mechanisms are overwhelmed, and silica particles are taken up by type II pneumocytes. Silicoproteinosis is a rapidly progressive condition that may result in death from respiratory failure within 1–2 years.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





