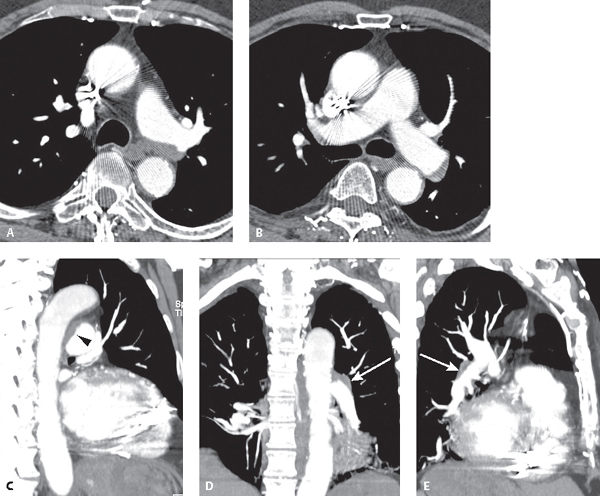
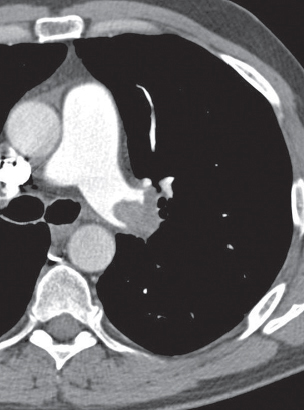
CASE 129 72-year-old man with past history of PTE and DVT presents with progressive dyspnea on exertion and fatigue Chest CTPA (mediastinal window) (Figs. 129.1A, 129.1B, 129.1C, 129.1D, 129.1E) demonstrates a peripheral, crescent-shaped intraluminal defect with obtuse angles along the left main lobar pulmonary artery’s posterior wall (Fig. 129.1A) and the lateral wall of the proximal descending left pulmonary artery (Fig. 129.1B). The obtuse margins of the intraluminal filling defect relative to the left pulmonary artery are readily appreciated on the MIP sagittal (Fig. 129.1C) (black arrowhead), coronal (Fig. 129.1D) (white arrow), and sagittal oblique (Fig. 129.1E) (white arrow) images. Compare the relative size of the main pulmonary artery (MPA) and ascending aorta. The MPA is not enlarged. Chronic Pulmonary Thromboembolic Disease Pulmonary Angiosarcoma PTE may be acute (≤2 weeks from initial event) or chronic (more long-standing, occurring weeks, months, or years after the acute event). Most acute emboli undergo fibrinolysis within 10–21 days and resolve spontaneously or under the course of medical therapy. Complete resolution may take several months in some patients. In a small percentage of patients, pulmonary emboli fail to resolve and become organized into fibrous tissue, resulting in chronic pulmonary thromboembolic disease (CPTE). CPTE obstructs blood flow through the lungs, increasing pulmonary artery pressures (PAP). In some cases, the PAP may approach or exceed systemic arterial pressures. Affected patients may complain of dyspnea on exertion or fatigue. Later on, patients may experience syncope and angina, and develop pulmonary artery hypertension (PAH), right heart enlargement, and eventual right heart failure (i.e., cor pulmonale). Pulmonary artery sarcoma (PAS) is a rare tumor frequently misdiagnosed as CPTE and is almost uniformly fatal, with reported survival times of a few months to a few years. Surgical resection is the single most effective modality for short-term palliation. The reported age at presentation ranges from 13 to 86 years, although most cases occur in middle age. PASs most often arise from the posterior wall of the MPA trunk. However, tumors may also arise from the right pulmonary artery (RPA), left pulmonary artery (LPA), pulmonary valve (PV), and right ventricular outflow tract (RVOT). Symptoms and signs such as weight loss, fever, anemia, and digital clubbing may suggest the correct diagnosis. Additional clinical findings include absence of risk factors for DVT, high sedimentation rate, nodular parenchymal opacities on CT (i.e., metastases), and failure to respond to anticoagulation. Unfortunately, none of these clinical features definitively excludes the possibility of CPTE. Fig. 129.1 (Images courtesy of Susan W. Bennett, MD, and Jeffery D. Settles II, MD, VCU Medical Center, Richmond, Virginia.) • Normal • Features of pulmonary artery hypertension (see Case 130) • Complete occlusion of a vessel that is smaller than adjacent patent vessels Fig. 129.2 Chest CTPA of a 45-year-old man with progressive dyspnea and CPTE. Large eccentric thrombus completely occludes the distal left pulmonary artery and demonstrates a convex margin with respect to contrast column (i.e., “pouch” defect). • Nonobstructive Filling Defects
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Clinical Findings
Imaging Findings
Chest Radiography
CTPA
Direct Signs of CPTE
 Vessel cut-off from CTPE has a convex margin with respect to contrast column (i.e., “pouch” defect) (Fig. 129.2)
Vessel cut-off from CTPE has a convex margin with respect to contrast column (i.e., “pouch” defect) (Fig. 129.2)
 Vessel cut-off from acute PTE is concave with respect to contrast column due to the trailing edge of thrombus
Vessel cut-off from acute PTE is concave with respect to contrast column due to the trailing edge of thrombus
 Decrease in vessel diameter distal to the complete obstruction from thrombus contraction
Decrease in vessel diameter distal to the complete obstruction from thrombus contraction
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine