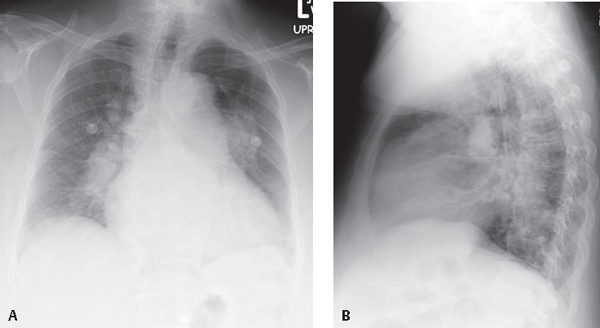
CASE 130 72-year-old man with progressive dyspnea, repeated syncopal episodes, and medically refractory chronic pulmonary thromboembolic disease PA (Fig. 130.1A) and lateral (Fig. 130.1B) chest radiographs demonstrate marked enlargement of the central pulmonary and interlobar arteries with sharply tapered or pruned peripheral vessels. The cardiac silhouette is enlarged. The enlarged right heart encroaches upon the retrosternal clear space on the lateral exam (Fig. 130.1B). Subsequent catheter pulmonary angiography (not illustrated) confirmed CPTE. Chronic Thromboembolic Disease Pulmonary Hypertension (CTEPH) • Idiopathic Pulmonary Artery Dilatation • Pulmonary Valve Stenosis • Pulmonary Artery Sarcoma (see Case 129) Fig. 130.1 Pulmonary artery hypertension (PAH) is defined by an elevated mPAP >25 mm Hg at rest (>30 mm Hg during exercise) and is classified by vascular changes affecting either the precapillary (arterial) or postcapillary (venous) pulmonary circulation. The latter occurs between the capillary bed and the left atrium. The vascular changes may be idiopathic, as in primary pulmonary hypertension (PPH) (i.e., precapillary level in the absence of an identifiable cause), but more commonly represent a secondary response to alterations in pulmonary blood flow. The postcapillary counterpart to PPH is pulmonary venoocclusive disease (PVOD), a rare idiopathic condition that diffusely affects the postcapillary pulmonary circulation but is characterized by normal pulmonary capillary wedge pressures (PCWP). Both precapillary and postcapillary pulmonary hypertension are regarded as secondary (SPH) when a cause can be established (Table 130.1). Precapillary hypertension creates a hemodynamic pattern of elevated right atrial pressure, increased mPAP, increased pulmonary vascular resistance, normal PCWP, and decreased cardiac output. Postcapillary hypertension is characterized by elevated right atrial pressure, increased resistance, and normal or elevated PCWP. Patients present with progressive dyspnea (60%), fatigue, angina, syncope, cor pulmonale, and Raynaud phenomenon. Women are affected three times as often as men. Onset of symptoms is typically in youth or middle age. Patients with portal hypertension (with or without liver disease), collagen vascular disease, HIV-AIDS, or a history of aminorex fumarate (an appetite suppressant) ingestion have an increased risk. Additionally, pregnant or postpartum patients and those using oral contraceptives may also be at increased risk. In addition to the hemodynamic derangements of PAH discussed above, PVOD is associated with normal or variably elevated PCWP. Normal left atrial and left ventricular pressures are characteristic and help exclude cardiac disease as the cause of venous hypertension. Patients present with progressive dyspnea, hemoptysis, and antecedent flulike symptoms. One-third of cases occur in children. There is a slight male predominance in adult patients. PVOD may be associated with pregnancy, bone marrow transplantation, or drug toxicity (e.g., carmustine, bleomycin, mitomycin). The clinical presentation and radiographic findings are suggestive of interstitial lung disease often leading to a delay in diagnosis. Table 130.1 Potential Causes of Pulmonary Artery Hypertension
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Young women
Young women
 Unilateral enlargement of main and left pulmonary artery
Unilateral enlargement of main and left pulmonary artery
 No pressure gradient
No pressure gradient
 Unilateral enlargement of main and left pulmonary artery
Unilateral enlargement of main and left pulmonary artery
 Left upper lobe vessels larger than counterpart right upper lobe vessels
Left upper lobe vessels larger than counterpart right upper lobe vessels
 Discussion
Discussion
Background
Etiology
Clinical Findings
Pulmonary Artery Hypertension
Pulmonary Venoocclusive Disease (PVOD)
Primary (Precapillary or Arterial) Pulmonary Hypertension | Primary (Postcapillary or Venous) Pulmonary Hypertension |
Idiopathic | Pulmonary venoocclusive disease (PVOD) |
Secondary (precapillary or arterial) pulmonary hypertension | Secondary (postcapillary or venous) pulmonary hypertension |
Congenital left-to-right cardiac shunt (e.g,, ASD, eisenmenger physiology) | Pulmonary capillary hemangiomatosis |
CPTE | Focal venous constriction (e.g., congenital venous stenosis, fibrosing mediastinitis) |
Tumor embolism (e.g., breast cancer, gastric cancer, renal cell, right atrial sarcoma, hepatoma) | Obstructive left atrial mass (e.g., left atrial neoplasia, myxoma, mitral stenosis, left ventricular failure) |
Infection (e.g., HIV-AIDS, schistosomiasis) | Compromised pulmonary venous drainage (e.g., anomalous pulmonary venous connections) |
IVDA (e.g., talc and other foreign body embolization) |