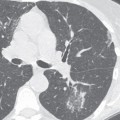
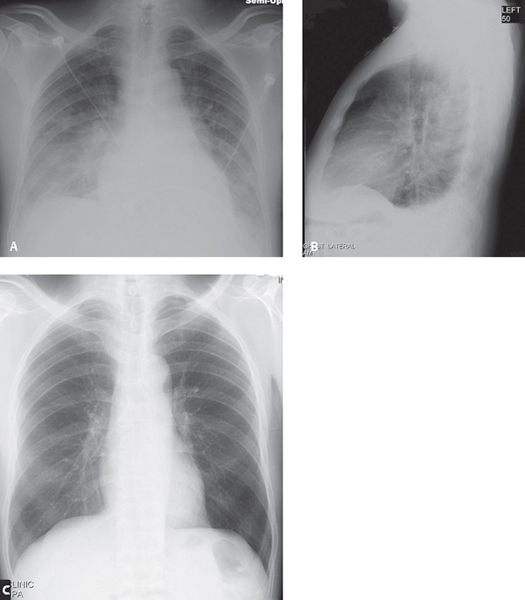
CASE 131 53-year-old man presenting to the Emergency Department with an acute onset of chest pain, hypoxia and shortness of breath AP (Fig. 131.1A) and lateral (Fig. 131.1B) chest radiograph demonstrates an enlarged cardiomediastinal silhouette; widened vascular pedicle; peripheral vascular engorgement; bilateral parahilar ground glass opacities, right greater than left; and bilateral pleural effusions, again right greater than left. Abnormal thickening of the posterior wall of the bronchus intermedius is seen on the lateral exam (Fig. 131.1B). Baseline PA (Fig. 131.1C) chest radiograph from five months earlier for comparison is grossly normal. Fig. 131.1 Increased Hydrostatic Pressure Pulmonary Edema; Acute Myocardial Infarction • Increased Hydrostatic Pressure Pulmonary Edema of Other Etiologies • Mixed Edema: Simultaneous Increased Hydrostatic Pressure and Permeability Changes Pulmonary edema results from the abnormal accumulation of fluid in the extravascular compartments of the lung. The relative amounts of intravascular and extravascular fluid are determined by the permeability of capillary membranes and the oncotic pressure. Pathophysiologic alterations in either will result in accumulation of fluid in the lung and edema. Pulmonary edema is divided into four main categories: (1) increased hydrostatic pressure edema, (2) permeability edema with diffuse alveolar damage (DAD), (3) permeability edema without DAD, and (4) mixed edema from simultaneous increased hydrostatic pressure and permeability changes (e.g., neurogenic pulmonary edema, reperfusion pulmonary edema, pulmonary edema following lung transplantation, re-expansion pulmonary edema, post-pneumonectomy edema, post–lung volume reduction edema). The variable clinical manifestations and radiologic patterns of pulmonary edema are summarized in Table 131.1. There are two pathophysiologic and radiologic phases of increased pressure hydrostatic pulmonary edema. These are interstitial edema and alveolar flooding. These phases are similar for left-sided heart failure and volume overload, the most common causes of increased pressure hydrostatic edema in both ICU and emergency department patients. The intensity and duration of these phases is related to the degree of increased pressure, which is determined by the ratio of hydrostatic to oncotic pressures. Interstitial edema occurs with an increase of 15–25 mm Hg in mean transmural arterial pressure. Alveolar flooding occurs with increases in transmural pressures >25 mm Hg. Pulmonary artery catheters are often used to assess and monitor hydrostatic pressure in critically ill patients. Pulmonary capillary wedge pressure (PCWP) reflects left atrial pressure and correlates well with the radiologic manifestations of heart failure and pulmonary venous hypertension. The PCWP can often be predicted on the basis of the radiologic findings by the application of the “rule of 6’s” as depicted in Table 131.2. However, in acute heart failure, a “lag time” is often seen between increased PCWP and radiologic manifestations of edema. Similarly, radiographic features of edema may lag behind clinically resolving pulmonary edema and reductions in PCWP. In approximately 10% of cases, the radiograph will demonstrate a central pattern of edema. This bat wing pattern generally occurs with the rapid onset of severe heart failure (e.g., acute mitral insufficiency associated with papillary muscle rupture, massive infarction, septic endocarditis with valve leaflet destruction) or renal failure (Fig. 131.2A, 131.2B). • Increased cardiothoracic ratio (Fig. 131.1A) • Increased vascular pedicle width (Fig. 131.1A) Table 131.1 Radiologic Patterns of Pulmonary edema Based on Clinical Scenario
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
Imaging Findings
Radiography
 >70 mm supine chest radiography
>70 mm supine chest radiography
 Measuring vascular pedicle: Draw vertical line paralleling left subclavian artery origin off transverse aorta; draw horizontal line extending from this line to lateral border of superior vena cava as it crosses right main bronchus
Measuring vascular pedicle: Draw vertical line paralleling left subclavian artery origin off transverse aorta; draw horizontal line extending from this line to lateral border of superior vena cava as it crosses right main bronchus
Clinical Scenario | Typical Radiologic Pattern |
Negative pressure (post-obstruction) | Septal lines Peribronchial cuffing Central alveolar edema (severe cases) Normal cardiac size |
Chronic pulmonary thromboemboli | Sharply demarcated areas of increased ground glass attenuation associated with dilated pulmonary arteries |
Pulmonary venoocclusive disease | Large pulmonary arteries Diffuse interstitial edema Numerous Kerley lines Peribronchial cuffing Dilated right ventricle |
Stage I near drowning | Kerley lines Peribronchial cuffing Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|