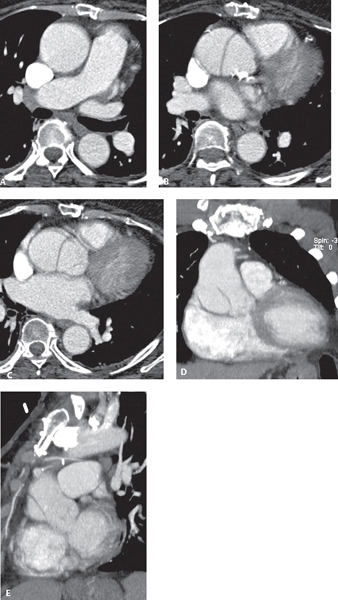
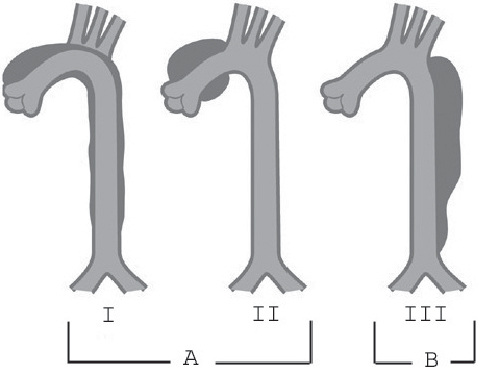
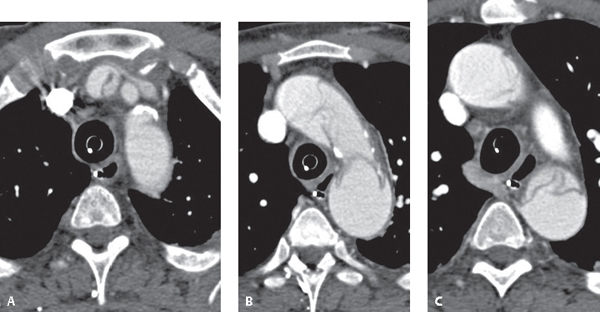
CASE 136 66-year-old woman with poorly controlled hypertension presented to the Emergency Department with sudden, sharp, tearing intractable chest pain MDCTA axial (Figs. 136.1A, 136.1B, 136.1C), coronal MIP (Fig. 136.1D), and sagittal MIP (Fig. 136.1E) images demonstrate an intimomedial flap limited to a significantly dilated ascending aorta and aortic root. Note the atheromatous changes in the thoracic aorta, its branch vessels, and the left main origin as well as left anterior descending coronary artery. Acute Dissection of the Thoracic Aorta (Type A) • Other Causes of Acute Coronary Syndrome Aortic dissection (AD) is the most common acute emergency condition of the aorta and is often fatal. The reported incidence is 2,000 new cases per year (USA). AD occurs two to three times more often than a ruptured abdominal aortic aneurysm, and it is two to three times more common in men. One-half of aortic dissections in women under 40 years of age occur during pregnancy. Patient outcome and survival are determined by the type and extent of AD and the presence of associated complications. There are two systems of classification (Fig. 136.2). The DeBakey system is based on the extent of the dissection, and the Stanford system classifies dissections by their proximal extent. DeBakey type I dissections (29–34%) involve the ascending aorta and extend around the arch and continue distally (Figs. 136.2, 136.3A, 136.3B, 136.3C). DeBakey type II dissections (12–21%) involve the ascending aorta only (Figs. 136.1A,136.1B, 136.1C, 136.1D, 136.1E, 136.2). DeBakey type III dissections (>50%) begin beyond the thoracic aorta branch vessels and continue down the descending aorta (IIIA), often below the diaphragm into the abdominal aorta (IIIB), and sometimes as far distally as the femoral arteries (Figs. 136.2, Fig. 136.4A, 136.4B, 136.4C, 136.4D, 136.4E, 136.4F). Stanford type A dissections (70%) involve the ascending aorta, regardless of where the entry tear begins and how far distally the dissection extends, and are equivalent to DeBakey type I and type II ADs (Figs. 136.1A, 136.1B, 136.1C, 136.1D, 136.1E, 136.2). Stanford type B dissections (20–30%) begin after the arch vessels and are equivalent to DeBakey type III (Figs. 136.2, Fig. 136.4A, 136.4B, 136.4C, 136.4D, 136.4E, 136.4F). An AD <2 weeks old is considered acute, whereas one >2 weeks old is considered chronic. Fig. 136.1 Fig. 136.2 Artist’s illustration depicting the three major types of aortic dissection Stanford type A is equivalent to DeBakey type I and/or II. Stanford B is equivalent to DeBakey type III. Fig. 136.3 MDCTA axial images show a type I (type A) AD of ascending and descending thoracic aorta (B,C) with extension into the brachiocephalic artery (A). Note the displaced intimal calcifications in the ascending aorta. Spontaneous separation of the aortic intima and adventitia allows circulating blood to gain access to and split the media of the aortic wall, creating a false lumen. This false lumen typically has pressures greater than or equal to that of the true lumen. The pressure difference, loss in transmural pressure across the intimomedial flap, and reduced elastic recoil in its thin outer wall due to elastin deficiency, result in expansion of the false lumen and compression-obstruction of the true lumen. These same factors predispose the false lumen to rupture.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


136 Acute Dissection Thoracic Aorta