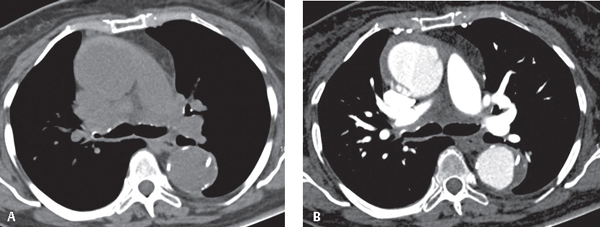
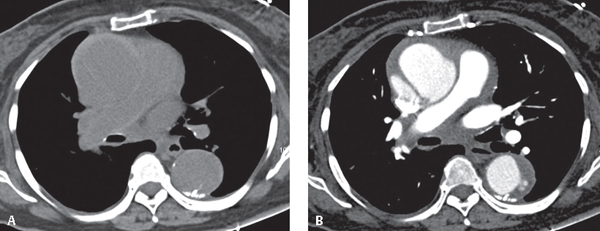
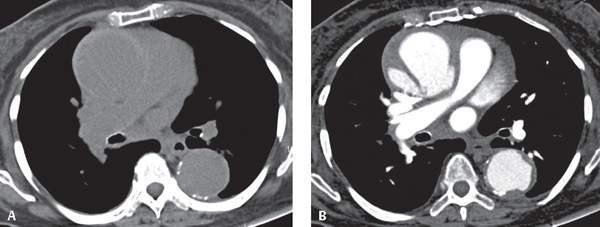
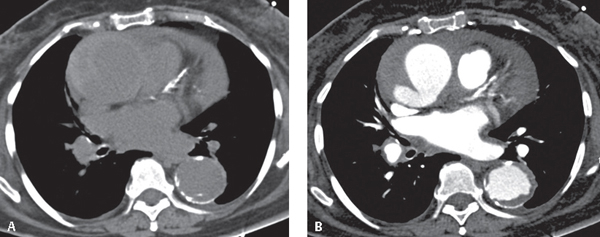
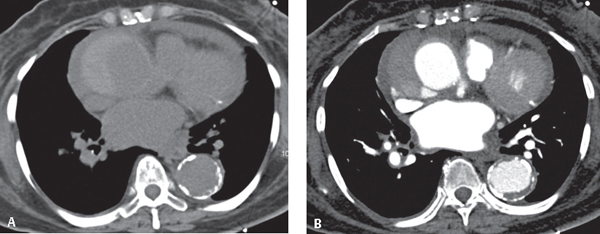
CASE 137 75-year-old woman presented to the Emergency Department with chest pain over the previous several hours with an abrupt increase in severity and intensity just prior to CT imaging Unenhanced chest CT images (Figs. 137.1A, 137.2A, 137.3A, 137.4A, 137.5A) demonstrate aneurysmal dilatation of the ascending aorta (5.6 cm) relative to the descending aorta with an associated eccentric high-attenuation intramural fluid collection. An intimomedial flap is suggested in the ascending aorta (Figs. 137.2, 137.3). Displaced intimal calcifications are seen in the descending aorta at 2:00 (Fig. 137.1) and 6:00 (Fig. 137.4). Note the high-attenuation pericardial effusion (i.e., hemopericardium) (Figs. 137.4, 137.5) and the extensive coronary artery calcifications. Contrast-enhanced CT images at approximately the same anatomic levels (Figs. 137.1B, 137.2B, 137.3B, 137.4B, 137.5B) depict a smooth, non-enhancing, eccentric region of aortic wall thickening involving the ascending aorta and confirm the presence of a spiraling intimomedial flap. Extensive mural thrombus is present in the descending aorta. Stanford Type A Intramural Hematoma Complicated by Overt Dissection • Acute presentation in symptomatic patient • Incidental finding in asymptomatic patient Fig. 137.1 Fig. 137.2 Fig. 137.3 Fig. 137.4 Fig. 137.5 Aortic intramural hematoma (IMH) is often described as an atypical or “flapless” aortic dissection and is thought to represent either an early-stage limited dissection or thrombosis of the false lumen in dissection. The distinguishing feature is the absence of the intimal disruption that characterizes classic aortic dissection. The Stanford system for classification of typical aortic dissection (AD) is applicable to the classification of IMH. That is, Stanford type A IMH involves the ascending aorta, with or without involvement of the descending aorta, and Stanford type B IMH involves the descending thoracic aorta, distal to the left subclavian artery origin. However, IMH exhibits a more variable natural history than classic AD, and may be characterized by periods of stabilization, regression, resolution, or progression to overt dissection. Type A IMH is more likely to progress to overt dissection than type B IMH. This is likely what occurred in this particular case. IMH results from rupture of the vasa vasorum and hemorrhage into the tunica media with resultant weakening of the aortic wall.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 None
None
 Aortitis: normal interspersed segments between involved sites
Aortitis: normal interspersed segments between involved sites
 Periaortic Lymphoma: thickened aortic wall with irregular external border
Periaortic Lymphoma: thickened aortic wall with irregular external border
 Atheroma: irregular intraluminal surface
Atheroma: irregular intraluminal surface
 Discussion
Discussion
Background
Etiology
Clinical Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


137 Intramural Hematoma Thoracic Aorta