Axial DWI at the level of inferior olivary nuclei.
Axial GRE image at the level of pons and brachium pontis.
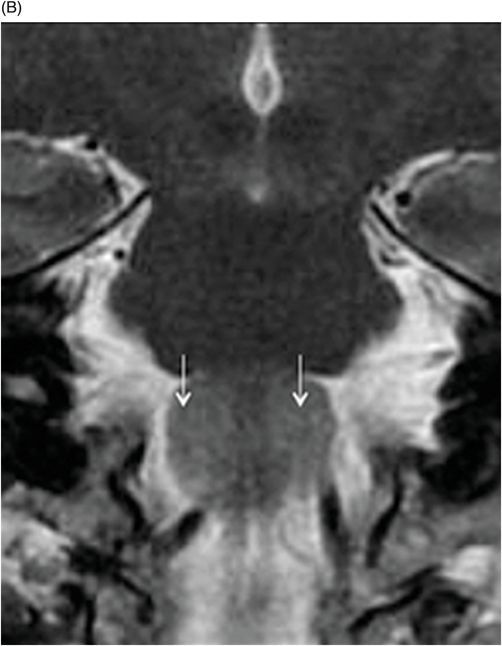
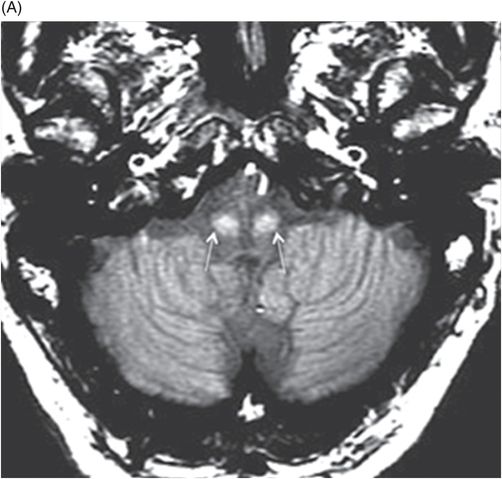
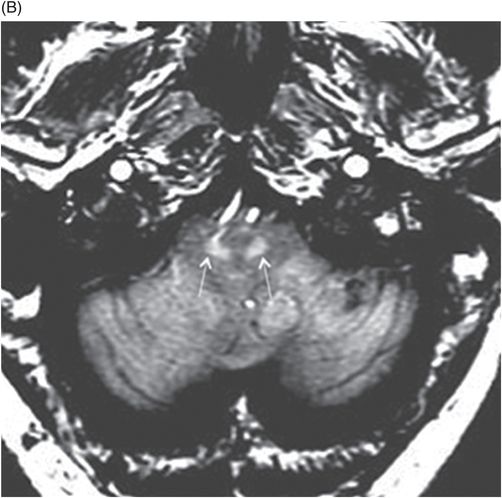
(A–B) Axial T1-MTC (magnetization transfer contrast) images at the level of inferior olivary nuclei.
Idiopathic Progressive Ataxia and Palatal Tremor
Primary Diagnosis
Idiopathic progressive ataxia and palatal tremor
Differential Diagnoses
Causes of bilateral hypertrophic olivary degeneration (brainstem stroke, tumor, hemorrhage, or demyelinating diseases)
Adult-onset Alexander disease with progressive ataxia and palatal tremor
Metronidazole toxicity
Imaging Findings
Fig. 15.1: (A) Axial T2WI and (B) Coronal images of the brainstem showed hyperintense signal changes in the bilateral inferior olivary nuclei (arrows). Fig. 15.2: Axial FLAIR image through the same level also demonstrated signal changes (arrows). Fig. 15.3: DWI showed no evidence of diffusion restriction. Fig. 15.4: GRE sequence of the proximal brainstem did not show any evidence of hemorrhage or mass lesion, similar to findings on T2WI (Fig. 15.1). Fig. 15.5: (A–B) Axial T1-MTC images show more pronounced signal changes (arrows).
Discussion
Insidious and progressive onset of ataxia and associated palatal tremors, with no identifiable structural lesion in the Guillain-Mollaret triangle to explain the presence of abnormal T2-FLAIR hyperintense signal changes in the inferior olivary nuclei that are more pronounced on T1-MTC images, as seen in this patient, are the key clinicoradiologic features suggestive of idiopathic progressive ataxia and palatal tremor (PAPT). Several etiologies such as stroke, hemorrhage, demyelination, and neoplasms resulting in bilateral hypertrophic olivary degeneration have been noted to cause symmetric T2-weighted and FLAIR signal abnormality changes that closely mimic PAPT; however, the lack of any predisposing factors excludes these pathologies from the diagnosis.
Neurology and neuroradiology literature describes a specific phenotype of adult-onset Alexander disease that can have imaging features similar to PAPT. Other imaging findings that are commonly associated with Alexander disease include signal changes in the basal ganglia and periventricular white matter. It has been suggested that involvement of the white matter along the hypothalamo-pituitary axis is responsible for the hypothermia, primary ovarian failure, and hypothyroidism often seen in these patients. Inferior olivary nuclei changes have also been described in toxic-metabolic conditions such as metronidazole toxicity. The acute presentation, involvement of dentate nuclei and splenium of corpus callosum with diffusion restriction and T2-FLAIR signal changes are the classical findings associated with metronidazole toxicity. However, there is complete resolution of imaging findings and symptomatic improvement after drug withdrawal, differentiating it from PAPT.
Palatal tremor is a rare neurodegenerative movement disorder of uncertain etiology. It is divided into essential palatal tremor (EPT), which comprises approximately 25% of cases, and symptomatic palatal tremor (SPT). Symptomatic palatal tremor is subdivided into sporadic and familial forms and is associated with rhythmic movements of the anterior soft palate and ear clicks that are attributable to levator palatini activity. Several etiologies such as stroke, hemorrhage, and tumors cause sporadic SPT. A small subgroup of the sporadic SPT form has no predisposing factors and is categorized as an idiopathic form. Symptomatic palatal tremor and idiopathic PAPT result from a lesion affecting the inferior olive, red nucleus, and contralateral dentate nucleus that together form the Guillain-Mollaret triangle. Common associations with this condition are progressive ataxia, cerebellar dysfunction, visual disturbance, and palatal tremor at 2 Hz.
Patients with familial PAPT present with corticospinal tract symptoms associated with significant brainstem and/or cervical cord atrophy. The familial form is also known as dark dentate disease due to abnormal iron accumulation/deposition. The familial variant does not have inferior olivary hypertrophy. The exact pathophysiology underlying palatal tremor in patients suffering familial PAPT syndromes also remains unclear.
In most cases, there are no identifiable imaging features on MRI. However, if present, the typical MRI features include hypertrophy and hyperintensity of the inferior olivary nuclei that are best depicted on T2-weighted and proton density sequences. In some cases, cerebellar atrophy may be noted. In addition to these findings, familial SPT is associated with brainstem and spinal cord atrophy. Recent case reports have emphasized the importance of T1-MTC pulse sequence. The bright signal on T1-MTC images is more evident as compared to T2-weighted and FLAIR sequences performed on 1.5 and 3 Tesla scanners. The signal changes are attributable to myelin loss or transsynaptic degeneration, similar to hypertrophic olivary degeneration. Few case reports with hypometabolism involving the dentate-rubro-olivary pathway have been described with dopaminergic dysfunction on FDG-PET imaging. The symptoms of PAPT are disabling with no effective treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree