- Risk for radiation-induced stochastic effects
- Sources of data for long-term risk of exposure to ionizing radiation
- Linear and nonlinear models of risk
- Risks associated with activities in radiology compared with risks associated with other activities
- Organizations that evaluate radiobiological data and make recommendations regarding radiation protection
- Regulatory agencies and regulations
Introduction
The purpose of radiation protection regulations is to ensure the safe use of ionizing radiation. This involves balancing the benefits of radiation applications with the risks. Regulations are established by national or state governments and have the force of law with civil and or criminal penalties for violations. Regulations historically require long and complex procedures prior to becoming law. Recommendations are promulgated by extra-government organizations interested in radiation safety. They do not have the force of law but usually are the basis for government regulations. This chapter covers both regulations and recommendations regarding safe radiation use.
The benefits of radiation in medicine come from improved diagnostic information. The risk comes primarily from an increased risk of cancer. Regulators must weigh the benefits and risks of using ionizing radiation for workers, patients, and the public. Current regulations do not place limits on the amount of radiation delivered to a patient. This is because the benefit and risk to an individual are evaluated by the physician ordering the procedure. Regulations usually divide exposures to humans into exposures to the general public and exposures to those working with radiation. Radiation exposure limits to radiation workers are higher than the limits for the general public because they presumably are receiving an additional benefit (their job) in return for the slightly higher risk associated with the higher allowed radiation exposure.
Expressions of Risk
Risk is often expressed as the probability or likelihood that an event will occur. In this section, we will discuss the probability of long-term, stochastic, detrimental biological effects occurring in a person’s lifetime. These stochastic effects include genetic damage and carcinogenesis.
Committee reports such as Biological Effects of Ionizing Radiations (BEIR) VII and International Commission on Radiological Protection (ICRP) 103 state risk from radiation exposure as either absolute risk or relative risk. Absolute risk is expressed as the number of occurrences of a disease in a population. Relative risk is often expressed as a fraction or percentage. The relative risk is defined as the ratio of the rate of disease in an exposed population divided by the rate of disease in an unexposed population:
The ERR is excess relative risk and is equal to the relative risk minus one.
The EAR is the excess absolute risk and is equal to the rate of disease in exposed population minus the rate of disease in unexposed population.
Example of a numerical application of absolute risk and relative risk:
Consider a population with a natural absolute risk for incidence of a disease of 20,000 cases in every 100,000 individuals. After this population is exposed to ionizing radiation, there are 20,300 disease cases observed.
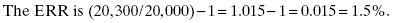
The EAR is (20, 300/100,000) − (20,000/100,000) = 300/100,000 or 300 in 100,000.
Organizations
There are four national and international organizations that evaluate epidemiological and radiobiological data and make recommendations regarding exposure to ionizing radiations. The recommendations are usually adopted by regulatory agencies and incorporated into national regulations. These organizations include the following:
These organizations have established recommendations based on data from human exposures to radiation, animal studies, and other laboratory data.
Sources of Data
A primary source of data used in committee reports such as BEIR VII and ICRP 103 is from the Life Span Study (LSS) in which the incidence of disease in the survivors of the nuclear weapon attacks on Hiroshima and Nagasaki has been tracked. The LSS data have been used to estimate quantitative risks of exposure to ionizing radiation.
The LSS data are unique for several reasons. The exposed population is large and includes approximately 100,000 individuals. People of all ages and both sexes were exposed to ionizing radiation during the attacks. The range of radiation exposures was large and included many who received relatively low doses (5–100 mSv) of radiation. The low doses are in the same range that can be expected from some diagnostic medical procedures. The LSS is also unique in that incidence and mortality data for cancer and other diseases have been tracked for nearly 70 years.
Dose–Response Models
Dose–response models are used to estimate the quantitative risk associated with an exposure to ionizing radiation. Obtaining a suitable model for risk associated with low doses has been controversial. For many survivors of the attacks on Nagasaki and Hiroshima, the exposure to radiation resulted in a high dose delivered at a high-dose rate. Occupational exposures and most radiological exposures involve low doses and low-dose rates. Yet the high dose, high-dose rate data from the LSS are still the primary source of data used for the estimation of risk factors due to low doses and low-dose rates.
To relate the high dose, high-dose rate data to low dose, low-dose rates, the dose and dose-rate effectiveness factor (DDREF) is used. Both the ICRP and BEIR Committee use a DDREF value of approximately 2. This used to account for the fact that the body repairs some radiation damage if the radiation exposure is spread over a longer time period. The assumption is that exposure to high doses and high-dose rates, such as found in nuclear weapon attacks, is approximately twice as likely to produce stochastic detrimental effects as low dose, low-dose rate exposures. In Fig. 15.1, the difference in the slope between the linear no-threshold (LNT) (high-dose rate) line and the LNT (low-dose rate) line in the figure is the DDREF.
Figure 15.1 Several possible methods of extrapolation from high-dose data to low-dose data. The linear no-threshold (low-dose rate) line is equivalent to the linear no-threshold (high-dose rate) line divided by the DDREF. Adapted from BEIR VII Phase II (2005). Modified from Brenner et al. (2003).
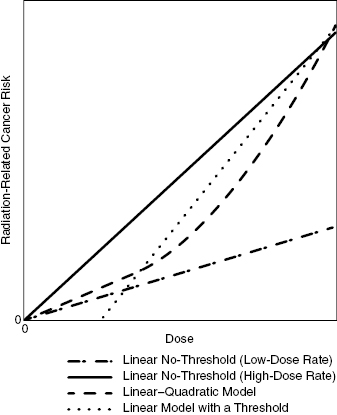
There are several dose-rate models that may be used to extrapolate from the high-dose data to the low-dose range where most occupational and radiological exposures are found. In the linear–quadratic model, the dose–response is nearly linear at low doses and then the slope increases at increasing doses. Some diseases, notably leukemia, are best modeled with this type of curve fit.
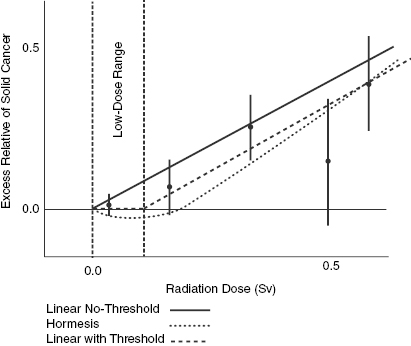
The linear models include the linear with-threshold and LNT models. In both linear models, the risk is assumed to increase linearly for all doses. In the linear with-threshold model, there is a nonzero, threshold level at which the ERR and EAR drops to zero. The ERR and EAR remain at zero for all doses less than the threshold. Evidence suggests that if a threshold truly exists, it is at low doses.
The model that is currently used by the BEIR Committee and the ICRP to model the risks for solid cancers is the LNT model. In this model, there is no threshold and the line crosses the origin. In the LNT model, it is assumed that any exposure to ionizing radiation carries a risk proportional to the dose. The LNT model is easy to use and is also the most conservative at relatively low doses (less than 500 mSv). In the latest reports, the ICRP and BEIR Committee still maintain that they do not have enough reason to depart from the LNT model. It should be noted that the ICRP and BEIR VII Committee state that the LNT dose–response model should only be used for radiation protection purposes. The model should not be used for epidemiological purposes or for estimation of risk to an individual.
There is some evidence that the LNT model does not provide good estimates of the dose–response in the low-dose range. Notice in Fig. 15.2 and Fig. 15.3 that the error bars in the low-dose range actually extend below 0.0 ERR. This could possibly indicate that low doses actually have zero risk or even less than zero risk. In other words, low doses of radiation could have a beneficial impact on health. The hypothesis that low doses of radiation actually reduce the risk of disease is known as hormesis. There is some evidence that exposure to low doses of radiation impart some degree of radioresistance to the organism being irradiated. The existence of hormesis in humans is inconclusive and has generally not been incorporated into radiation protection policy.
Figure 15.2 Excess relative risks of solid cancer for survivors of nuclear weapon bombings of Japan. The error bars represent approximate 95% confidence intervals. Adapted from BEIR VII Phase II (2005).
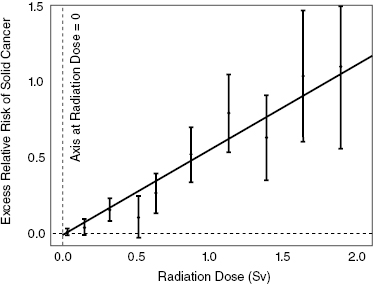
Figure 15.3 Close-up of low-dose region for excess relative risks of solid cancer for survivors of nuclear weapon bombings of Japan. The error bars represent approximate 95% confidence intervals. Adapted from BEIR VII Phase II (2005).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree