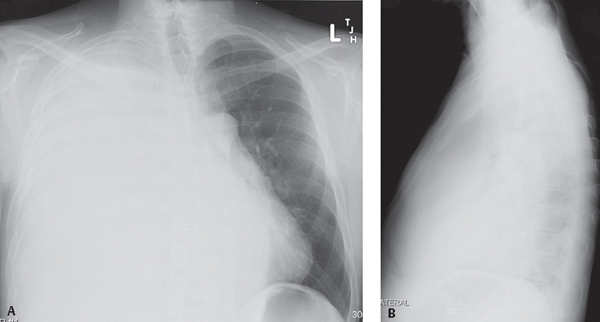
CASE 171 40-year-old man with liver failure, ascites, and absent right-sided breath sounds PA (Fig. 171.1A) and lateral (Fig. 171.1B) chest radiographs show complete “white-out” of the right hemithorax. No air bronchograms are seen and only the left diaphragm is perceptible on the lateral exam. Note the contralateral displacement of the tracheal air column and mediastinum “away” from the white-out on the PA exam (Fig. 171.1A). Massive Unilateral Pleural Effusion; Hepatic Hydrothorax • Unilateral Opaque Thorax (“White-out”) is quite broad (Table 171.1) • Differential can be narrowed based on location of trachea (Table 171.2) • Other Causes of Unilateral Pleural Effusion (Table 171.3) Fig. 171.1 Table 171.1 Unilateral Opaque Thorax (‘White-out”)
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
Pleural Disease | Pulmonary Disease | Chest Wall Deformity |
Pleural effusion | Total lung collapse | Significant scoliosis |
Pleural thickening | Pneumonia | Severe congenital or acquired chest wall deformity |
Fibrothorax | Pneumonectomy | Large chest wall hematoma |
Diffuse malignant mesothelioma | Pulmonary agenesis | Large chest wall tumor |
Metastatic pleural cancer |
| Diaphragmatic hernia |
Table 171.2 Unilateral Opaque Thorax (“White-out”) Based on Trachea Location
Pulled “Toward” White-Out | Pushed “Away” from White-out | Central Position |
Total lung collapse | Pleural effusion | Pleural thickening |
Pneumonectomy | Diaphragmatic hernia | Fibrothorax |
Pulmonary agenesis | Severe congenital or acquired chest wall deformity | Diffuse malignant mesothelioma |
|
| Metastatic pleural cancer |
|
| Large chest wall hematoma |
|
| Large chest wall tumor |
Table 171.3 Unilateral Pleural Effusion Differential Diagnosis
Heart failure |
Parapneumonic-empyema |
Neoplasia |
Pulmonary thromboembolism |
Autoimmune-collagen vascular disorders |
Trauma |
Chylothorax |
Subdiaphragmatic diseases and disorders |
 Discussion
Discussion
Background
Pleural effusion is an abnormal accumulation of fluid in the pleural space and a common manifestation of local and systemic diseases that involve the thorax, affecting an estimated 1.3 million persons each year. The normal pleural cavity contains a small volume of fluid (5–15 mL) that provides a frictionless surface between the visceral and parietal pleura as lung volume changes during respiration. However, between 1 and 2.5 L of pleural fluid is produced each day. Pleural fluid normally forms and flows from capillaries in the parietal pleura into the pleural space and is absorbed through parietal pleural lymphatics. The parietal pleura vasculature drains to the right side of the heart, whereas the visceral pleura vasculature drains to its left side. The formation and absorption of pleural fluid is governed by Starling’s equation. That is, the net filtration and resorption of water and its solutes (i.e., pleural fluid) across a semi-permeable membrane (i.e., pleura) are determined by balances between hydrostatic and osmotic pressures. Anything that upsets this balance results in accumulation of pleural fluid: (1) increased hydrostatic pressure (e.g., heart failure, constrictive pericarditis); (2) decreased osmotic pressure (e.g., cirrhosis, hypoalbuminemia); (3) decreased pleural space pressure (e.g., atelectasis); (4) increased microvasculature permeability (e.g., neoplasia, inflammatory conditions); (5) impaired lymphatic drainage (e.g., neoplasia, fibrosis, radiation therapy); and (6) increased transportation of fluid from the peritoneal space into the pleural space (e.g., ascites, nephrotic syndrome).
Etiology
Thoracentesis is usually performed to evaluate pleural effusions of unknown etiology. Fluid is examined grossly and submitted for biochemical analysis, red and white blood cell counts, Gram and acid-fast stains, and cytology. More invasive procedures, including closed, open, or thoracoscopic biopsy, are sometimes necessary to establish a diagnosis. Most effusions are categorized as transudates or exudates using criteria established by Light. Such categorization is useful in narrowing the differential diagnosis (Tables 171.4, 171.5) and dictating patient management. Exudates exhibit one or more of the following characteristics: (1) pleural fluid protein/serum protein ratio >0.5; pleural fluid lactic acid dehydrogenase (LDH)/serum LDH ratio >0.6; and (3) pleural fluid LDH ratio greater than two-thirds the normal serum LDH. Transudates are characteristically clear, straw-colored, have a low protein concentration, and have few cells. Most transudates result from systemic factors that alter pleural fluid formation or absorption (Table 171.4). Exudative
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree