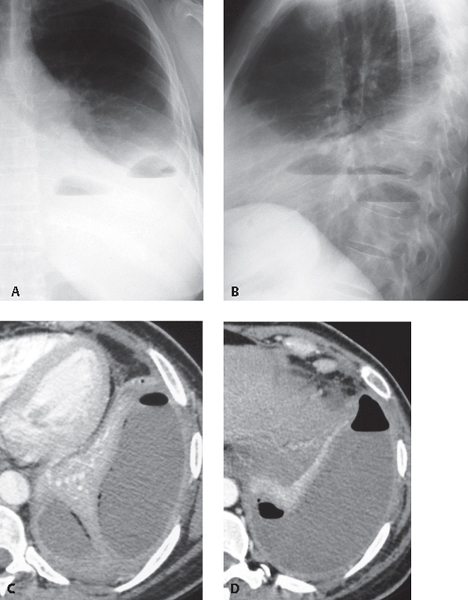
CASE 172 40-year-old woman with cough and fever Coned-down PA (Fig. 172.1A) and lateral (Fig. 172.1B) chest radiographs demonstrate a large left pleural effusion with two air-fluid levels. Note the difference in length of the superior air-fluid level on the two orthogonal radiographs (Figs. 172.1A, 172.1B). Contrast-enhanced chest CT (mediastinal window) (Figs. 172.1C, 172.1D) shows a loculated left pleural effusion with two air-fluid levels (Fig. 172.1D) and smooth, mildly thickened enhancing visceral and parietal pleural surfaces (split pleura sign) that surround the fluid (Fig. 172.1D). Note the mass effect on the adjacent atelectatic left lower lobe (Fig. 172.1C). Fig. 172.1 Empyema; Bronchopleural Fistula • Loculated Pleural Effusion—Post Instrumentation • Malignant Pleural Effusion with Bronchopleural Fistula Pleural effusions caused by infection are generally exudative and are classified into three groups, based on pleural fluid analysis. Simple parapneumonic effusions are culture and Gram stain negative. Complicated parapneumonic effusions are culture and Gram stain negative but have high LDH levels, low pH (<7.2), or low glucose levels (<40 mg/dL). Empyema is characteristically purulent on gross inspection, has high neutrophil counts and low pH, and may be culture or Gram stain positive. Differentiation between parapneumonic pleural effusions and empyemas is based on pleural fluid analysis rather than on imaging features. Empyema may be associated with bronchopleural fistula when a communication is established between the infected pleural fluid and adjacent airways. Bronchopleural fistula is the most frequent cause of abnormal air collections and air-fluid levels within empyemas. Pleural infection may result in progressive pleural thickening, with formation of an inelastic fibrous membrane that may encase the lung and restrict function (pleural peel). Empyema is most commonly due to pleural extension of infection from adjacent pneumonia, typically caused by Gram-negative bacteria, anaerobic bacteria, Staphylococcus aureus, Streptococcus pneumoniae, or Myco-bacterium tuberculosis. Other causes include lung abscess, septic emboli, and subphrenic infection. Affected patients present with fever, chills, cough, and pleuritic chest pain. Physical examination may reveal chest wall erythema and edema. Absence of fever or leukocytosis does not exclude the possibility of empyema. Detection of grossly purulent pleural fluid by thoracentesis is diagnostic. • Findings of uncomplicated pleural effusion (see Case 171) • Ovoid, lenticular, or rounded pleural mass; loculated pleural effusion • Lesion margins often better defined in one of two orthogonal radiographs, discrepant margin visualization (incomplete border sign) • Bronchopleural fistula
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
Imaging Findings
Chest Radiography
 Air-fluid level(s) within a pleural mass (loculated empyema) or pleural effusion (Figs. 172.1A, 172.1B)
Air-fluid level(s) within a pleural mass (loculated empyema) or pleural effusion (Figs. 172.1A, 172.1B)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree