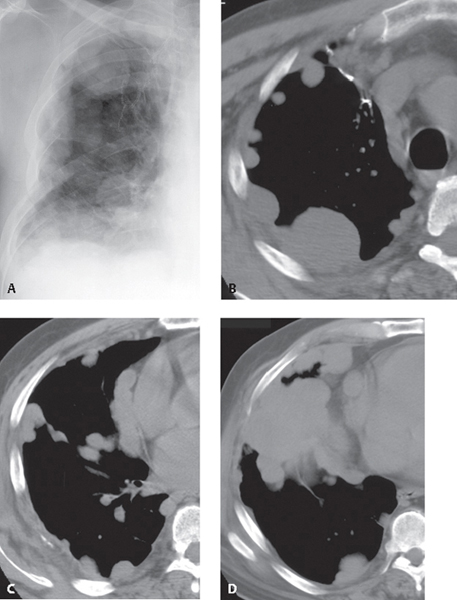
CASE 176 48-year-old woman with recently diagnosed lung cancer Coned-down PA chest radiograph (Fig. 176.1A) demonstrates circumferential nodular right pleural thickening with encasement and loss of volume of the right lung. Note the right upper lobe surgical chain sutures. Unenhanced chest CT (mediastinal window) (Figs. 176.1B, 176.1C, 176.1D) shows circumferential nodular pleural thickening that involves the major fissure (Fig. 176.1C) and is produced by multi-focal pleural masses of various sizes (Figs. 176.1B, 176.1C, 176.1D). Many pleural nodules/masses measure over 1 cm in thickness. Right upper lobe surgical chain sutures (Fig. 176.1B) are from prior wedge resection of a primary lung adenocarcinoma. Fig. 176.1 Pleural Metastases; Adenocarcinoma of the Lung • Pleural Metastases from Extrapulmonary Primary Malignancy • Diffuse Malignant Pleural Mesothelioma • Lymphoma • Invasive Thymoma Pleural metastases are the most common pleural malignancy and typically result from primary cancers of the lung, breast, pancreas, stomach, and ovary. However, pleural metastases can originate from primary neoplasms in almost any organ. Malignant pleural effusion is the most common manifestation of metastatic pleural disease and occurs in approximately 60% of patients with pleural metastases. The majority of malignant pleural effusions (75%) occur as a result of lung and breast cancers and lymphoma. Pleural metastases may also manifest as soft-tissue nodules or masses. Pleural metastases may develop from direct pleural invasion by an adjacent peripheral lung cancer. “Drop” metastases may produce circumferential pleural involvement and may develop in patients with invasive thymoma. Metastases may also disseminate to the pleura via hematogeneous and lymphatic routes.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree