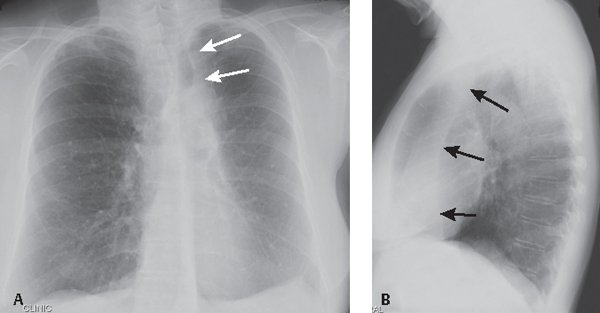
CASE 186 60-year-old woman status post antecedent left upper lobectomy for adenocarcinoma PA (Fig. 186.1A) and lateral (Fig. 186.1B) chest X-rays show decreased volume in the left thorax and leftward anterior mediastinal shift. The left diaphragm is elevated and a juxtaphrenic peak is present. The interface between lung and the shifted anterior mediastinum forms an upper triangle sign mimicking mediastinal widening (Fig. 186.1A) (white arrows). The anterior interface of the LLL with the mediastinum correlates with this finding on the lateral exam (Fig. 186.1B) (black arrows) and should not be confused with a displaced left oblique fissure. Note the absence of a LUL bronchial orifice on the lateral exam (Fig. 186.1B) Left Upper Lobectomy Left Upper Lobe Collapse (see Case 42) The various pulmonary resection techniques include wedge resection, excision of tumor confined to one specific area and a small margin of normal lung; segmentectomy, exaggerated wedge resection entailing excision of a larger volume of tissue but not the entire lobe; lobectomy, excision of entire lobe with or without accompanying lymphadenectomy, typically performed for early stage non–small cell lung cancer (see Section VI); sleeve lobectomy, an alternative to pneumonectomy in select cases of cancer involving a lobar orifice and airway reconstruction with end-to-end-anastomosis and wrapping of anastomosis with pleura or other vascularized tissue, for which the most common site is RUL (75%), followed by LUL (16%) and LLL (8%); and pneumonectomy, removal of the entire lung (see Case 187). This case will focus on lobectomy. Lobectomy can be considered the ultimate form of volume loss. That is, the anatomic and radiologic alterations in pulmonary and extrapulmonary structures closely resemble those of severe lobar collapse (see Section IV). Displacement of mediastinal structures into the post-lobectomy space may mimic lobar collapse. Postoperative pleural effusion or fibrothorax in the post-lobectomy space likewise may simulate lobar collapse on imaging. Reorientation of the left lung after lobectomy is characterized by a pleuromediastinal interface that also simulates lobar collapse. Right-sided lobectomies are characterized by reorientation of the remaining two lobes and apposition of the visceral interlobar pleural surfaces and formation of “neofissures.” Neofissures may be difficult to perceive on conventional radiography as they are often not parallel to the X-ray beam axis. Fig. 186.1 (Images courtesy of Anthony D. Casssano, MD, VCU Medical Center, Richmond, Virginia.) • Anastomotic dehiscence. May manifest as an airway complication after sleeve lobectomy (6%) and result in bronchopleural fistula. CT shows a defect in the bronchial wall or extraluminal air about the anastomosis, bronchial irregularity, or narrowing. • Bronchopleural fistula. Dreaded complication with high mortality (see Case 187). Usually develops at the bronchial stump after pneumonectomy or lobectomy. • Hemothorax (see Case 187) • Lobar torsion. Following RUL lobectomy, the RML relocates into the upper thorax. RML torsion may occur if it twists clockwise on its narrow vascular pedicle. The degree of torsion is usually 180°. Torsion of hilar vessels causes impaired circulation and predisposes to hemorrhagic infarction. Affected patients may have bronchorrhea, hemoptysis, shock, and sepsis. Mortality is high if the condition goes unrecognized and the affected lobe is not reduced or excised. Radiography shows rapidly developing consolidation with volume expansion of the affected lobe (Fig. 186.2A) and neofissure reorientation. CT findings include amorphous soft-tissue attenuation at the hilum, poor enhancement of torsed lobe with increased volume, ground glass opacity, septal thickening, neofissure reorientation, and tapered obliteration of the affected pulmonary artery and bronchus (Figs. 186.2B, 186.2C). • Non-obstructive atelectasis. Results from retained secretions, edema at the anastomosis, interruption of ciliary epithelium and lymphatic vessels, and partial denervation of the reimplanted lobe. This occurs in 5–10% of sleeve resections and more commonly follows those involving the lower lobe. Secondary infection may ensue. • Persistent air leak. Most patients undergoing lobectomy or segmentectomy develop some degree of air leak. This most often occurs in older patients and in those with underlying emphysema or incomplete/absent interlobar fissures and resolves within 24–48 hours. A persistent air leak continues beyond seven days. Imaging studies show persistent pneumothorax, pneumomediastinum, or subcutaneous air. • Pneumonia.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Post-Lobectomy Complications
Early Postoperative Lobectomy Complications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





