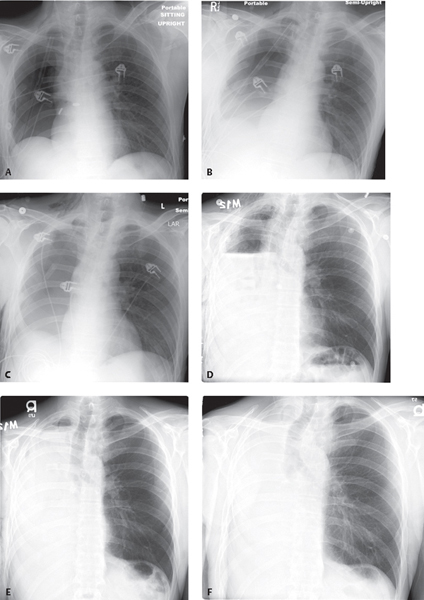
CASE 187 57-year-old man status post right pneumonectomy for adenocarcinoma First postoperative chest exam (Fig. 187.1A) following right pneumonectomy shows an air-containing pleural space, slight ipsilateral mediastinal shift and diaphragmatic elevation, and mild vascular congestion of the contralateral lung. The right sixth posterior rib has been partially resected and the chest tube is in place. Minimal subcutaneous air is present. Frontal chest exams on postoperative day 1 (Fig. 187.1B), day 3 (Fig. 187.1C), and day 5 (Fig. 187.1D) demonstrate gradual but progressive filling of pneumonectomy space with fluid and decreasing volume of air. Note the progressive ipsilateral mediastinal shift, diaphragmatic elevation, and overinflation of the left lung. By post-op day 15 (Fig. 187.1E) 90% of the pneumonectomy space is fluid-filled. Three months later (Fig. 187.1F) the space is completely obliterated. The mediastinum remains displaced appropriately toward the ipsilateral thorax. Post-Pneumonectomy; Normal Postoperative Sequence None Pneumonectomy is the treatment of choice for lung cancer, advanced medically refractory infection, and complicated bronchiectasis. Radiologists must be cognizant of the normal postoperative appearance of the post-pneumonectomy chest to avoid misinterpreting expected findings with true complications. Pulmonary resection techniques include intrapleural pneumonectomy, resection of the involved lung and surrounding visceral pleura (most common); extrapleural pneumonectomy, en bloc resection of the ipsilateral lung, parietal and mediastinal pleura, pericardium, and diaphragm; intrapericardial pneumonectomy, which entails opening the pericardium and dividing vessels involved by tumor within the pericardial sac; and sleeve pneumonectomy, resection of tumor involving the tracheobronchial angle, carina, or lower trachea and the ipsilateral lung with anastomosis of proximal contralateral mainstem bronchus to the lower trachea. The initial postoperative chest radiograph should demonstrate an air-containing ipsilateral pleural space, slight ipsilateral mediastinal shift and diaphragmatic elevation, and mild vascular congestion of the contra-lateral lung (Fig. 187.1A). Thereafter, the normal pneumonectomy space begins to fill with serosanguineous fluid at a rate of about two ribs per day (Fig. 187.1B, 187.1C, 187.1D), although the left thorax tends to fill more rapidly than the right. By the end of the second postoperative week, 80–90% of the pneumonectomy space should be obliterated (Fig. 187.1E), and complete obliteration is typically seen by 2–4 months (Fig. 187.1F). The post-pneumonectomy space is usually obliterated by a combination of fluid, ipsilateral diaphragmatic elevation and mediastinal shift, and overexpansion of the contralateral lung. Ipsilateral mediastinal shift is the most reliable radiologic sign of a normal postoperative course. Fig. 187.1 Complications occur in 20–60% of patients following pneumonectomy. Complications may occur early in the postoperative course or at a later time. • Hemothorax. Most commonly results from inadequate hemostasis of a bronchial artery or systemic vessels in the chest wall. Other causes include ligature slippage from a pulmonary vessel and iatrogenic vascular injury. Mortality rate is <0.1%. On radiography, hemothorax presents as a rapidly enlarging pleural effusion. CT features include heterogeneous or high-attenuation pleural effusion or a fluid-hematocrit level. • Chylothorax. Injury to the thoracic duct or one of its branches results in the accumulation of chyle in the pleural space. Potential sites of injury include inferior right paravertebral region during extrapleural pneumonectomy; pericarinal and subaortic region during radical lymphadenectomy; and pulmonary ligaments during intrapleural pneumonectomy. • Pulmonary edema.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Normal Post-Pneumonectomy Radiography Changes
Post-Pneumonectomy Complications
Early Postoperative Complications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine



