2 Special Radiographic Procedures
Digitally acquired projection radiographs can be postprocessed and transmitted electronically by a picture archiving and communication system (PACS) and filed. For diagnosis of skeletal abnormalities, digital luminescence radiography with phosphorus storage screens, as well as digital image-intensifier cinefluorography, is employed. Direct radiography with flat-panel detectors, which at present is not widely used, is a very promising method. Magnification techniques for high-definition images can demonstrate early stages of inflammatory and metabolic diseases.
Magnifying radiography with mammography films and the direct radiographic magnification (DIMA)technique are available for this purpose. Inflammatory changes of soft tissue can be visualized with low-kilovoltage radiography with a tube current of 28–30kV. All these methods are reserved for special indications. Conventional tomography with multidimensional blurring figures is no longer used. Pathologic movements in dynamic carpal instabilities can be documented at high temporal resolution with cineradiography.
Digital Radiographic Procedures
Aside from the sectional imaging techniques of ultrasonography, computed tomography (CT), and magnetic resonance (MR) imaging, digital imaging systems are also employed with increasing frequency in projection radiography.
The typical characteristic of all digital techniques is the separation of the process of acquisition of the signal from the object under examination and the display of the signal as a luminance distribution in a computer system. The following quality parameters in combination provide good perception of image details.
The resolution and thereby the image definition are limited by the image matrix and the pixel size. In comparison to film–screen systems, digital imaging techniques are characterized by reduced spatial resolution. The spatial resolution of digital systems depends on the size of the matrix and the image format employed. To ensure good diagnostic detail recognition of bony structures, 2K systems (image matrix 2048×2048) are recommended for projection radiography of the hand. A matrix of 2048×2048 in a cassette format of 18×24cm results in a resolution of 5 line pairs (Lp)/mm, and in a cassette format of 24×30cm gives resolution of 3.3 Lp/mm. In comparison, conventional film–screen systems deliver a spatial resolution between 5 and 8 Lp/mm.
This is contrasted with the advantages of improved contrast resolution of digital imaging systems. Digital images are generally stored with an image depth of 10 or 12 bytes/pixel. Digitally acquired images offer the possibility of subsequent postprocessing of the brightness and contrast. Overlapping of the image signal by interference signals (noise) is primarily caused by quantum mottle. A direct relationship exists between the noise and the applied dose.
Further advantages, apart from postprocessing, are the possibilities of telecommunication, making a diagnosis on the monitor, and filing without film on RAID-array storages, laser disks, and tape recorder in a picture archiving and communication system (PACS). Alternatively, a hard copy can be made.
The three different imaging systems in digital projection radiography are explained below.
Digital Luminescence Radiography (DLR)
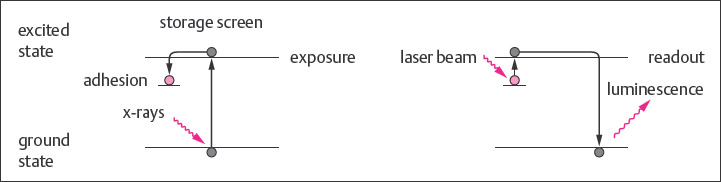
The Principle
In digital luminescence radiography, the film–screen system is replaced as a data-storage medium by a storage screen, which, for example, consists of a layer of phosphorus compound. Special cassettes with formats identical to those of conventional systems are required. The cassettes equipped with phosphorus storage screens can be exposed in conventional radiographic examination units, making the procedure economic. The radiographic absorption profile is saved as a temporary image by the activation of electrons to a higher energy level on the phosphorus screen. The read-out process involves scanning with a beam of a helium laser ( Fig. 2.1 ). The energy absorbed within the phosphorus crystals during x-ray exposure is released locally as luminescence according to the information in the virtual image. The distribution of the emitted light is stored as an electrical signal via photomultipliers. The digitally stored DLR images can be postprocessed on a computer work-station.
Technical Procedure
Storage screens have high sensitivity for x-rays and, in principle, enable radiation exposure to be reduced. Since the signal-to-noise ratio decreases with lower doses, reduction of the dose in diagnostic imaging of the hand is only possible to a limited degree. Dose reductions of about 15% can be achieved in follow-up radiography in traumatology and in pediatric radiography. Radiation quality and doses applied in digital luminescence radiography are generally comparable to those of the conventional film–screen technique.
Images that have been over- or underexposed in the acquisition process can usually be corrected during postprocessing, since the characteristic gradation curve is linear over a large range in storage-screen systems. The linearity over a large range results of faulty exposure can thus be compensated.
Difficulties in interpretation in skeletal imaging can be caused by overshoot artifacts in the immediate vicinity of materials used for osteosynthesis. Extinction phenomena, which in the worst case can mimic loosening of material or infection, may arise with metallic implants with low image resolution.
Indications
Given its many advantages, digital luminescence radiography with storage screens is currently the favored imaging procedure in projection radiography of the musculoskeletal system. K2 systems with an image matrix of 2048×2048 are used for diagnosis of the hand.
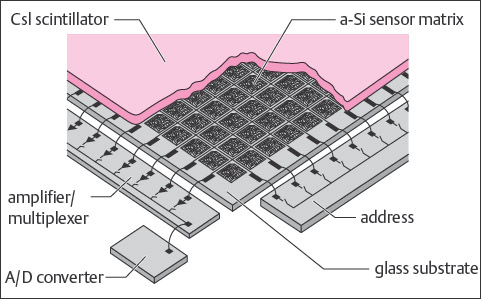
Direct Radiography with Flat Detectors
The Principle
In addition to the phosphorus storage-screen technique, projection radiography with electronic flat detectors (semiconductors and flat-panel detectors) provides a further digital procedure for projection radiography. These systems employ either amorphous silicon or selenium as the detector. In silicon or selenium detectors, information about the absorbed x-ray profile is recorded directly, electronically enhanced, and transferred to an analog-to-digital (A/D) converter ( Fig. 2.2 ). Since an intermediate step of optical, electronic, or mechanical scanning is unnecessary, this technology is referred to as direct radiography. Direct radiography has superior quantum efficiency to other imaging systems, resulting in lower image noise at the same radiation dose. This improved quantum efficacy can potentially be used to reduce the radiation dose.
In a further application, real-time images that enable digital fluoroscopy to be performed can be generated with the selenium and silicon detectors because of their active matrix.
Technical Procedure
Positioning methods and x-ray exposures in direct radiography with flat detectors are the same as for conventional projection radiography. The exposure values are equivalent to the common kV and mAs values over wide ranges. After exposure on the flat-panel detector system, the digital image information is immediately available for postprocessing and channeling into a PACS environment. In routine use, the processing is rapid because of the absence of cassettes is an advantage. Static integration of the system into the Bucky table or the use of a wall-mounted cassette holder introduces limitations, however, since both prevent mobile use with the use of individually placed cassettes.
Indications
The advantages of improved image quality, exposure without cassettes, and digital image acquisition and archiving make flat-panel direct radiography the imaging technique of the future. The flat-panel technique is not widely employed at present because the complex production techniques for the crystals result in high investment cost.
Image-intensifying Radiography
The Principle
In digital image-intensifying radiography, image recording is performed with a CCD (charge-coupled device) camera, which is integrated into the image-intensifying unit of a fluoroscopy unit as a recording system. The prototype of digital image-intensifying radiography is digital subtraction angiography (DSA). The resultant image is immediately available on the monitor screen. The digital image acquisition makes postprocessing possible (e.g., mask subtraction, pixel shift, edge enhancement, adjustment of contrast and brightness).
Technical Procedure
Fluoroscopy of the hand is achieved with spot films or angiography series. For high-contrast musculoskeletal imaging (plain osseous and arthrographic series), a matrix size of 1024×1024 with a spatial resolution of 1.8–2.0 Lp/mm is generally sufficient. For minute bony lesions, an image matrix of 2048×2048 is desirable. Digital image-intensifying radiography makes it possible to reduce radiation dose, but this desirable effect in radiation hygiene is achieved at the cost of a reduced signal-to-noise ratio and decreased detail recognition.
Indications
Besides digital subtraction angiography, digital image intensifying radiography is used for fluoroscopic analysis and documentation. Despite reduced spatial resolution, arteriography of the hand (Chapters 5 and 48), movement analysis of the wrist, and three-compartment arthrography Fig. 3.2 can be comfortably performed and documented.
Radiography with Mammography Films
The Principle
Survey views of the entire hand are performed with a film–screen combination providing a sensitivity value of 200 in traumatology. To achieve greater detail resolution, a less-enhancing mammography film–screen combination with a sensitivity value of 25 can be used. At a tube focus size of 0.6 mm, the spatial resolution is 6–8 Lp/mm.
Technical Procedure
The mammography films, contained in special cassettes, are exposed on the Bucky table with a suspended above-table unit (FFD 105cm) without the use of a scattered-radiation grid. Typical exposure values are 55 kV and 6.4mAs.
|
Indications
Because of their higher radiation dose requirements than those for standard films (up to eightfold greater), mammography film–screen combinations should be employed only when strictly indicated for the diagnostic purposes listed in Table 2.1 .
Techniques in Magnification Radiography
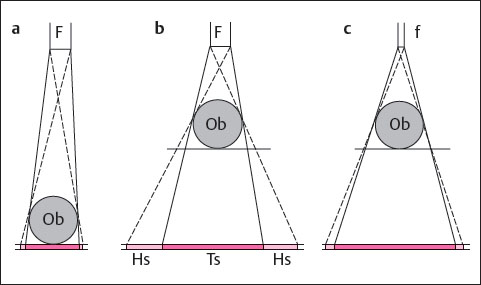
Increasing the distance between object and film enlarges the image at a constant film–focus distance. Decreasing the size of the tube focus can compensate for the resulting lack of sharp detail ( Fig. 2.3 ). Because of the limited x-ray performance at a small focus, only thin objects can be examined with the magnification technique. The clinical objectives for imaging of the hand listed in Table 2.2 can generally be examined with the magnification technique.
The magnification technique makes it possible to recognize even the smallest structural irregularities in the cortical and trabecular bone and demineralization at the subchondral bone plate, as well as inflammatory swelling of the soft tissues. Ultrafine-focus magnification imaging of soft tissues and osseous structures can be carried out with the Groedel or direct radiographic magnification (DIMA) technique.
|
Magnification Radiography with Mammography Equipment
The Principle
The X-ray focus of mammography equipment has a size of 0.1–0.4mm. The object should be enlarged by at least a factor of 1.5 in the image plane. If the enlargements are made at a focus–film distance of 0.65m and an object–focus distance of 0.34m, the result is an enlargement factor of 2. Skeletal radiographs for investigation of the fine structure of the trabecular bone are performed with an aluminum filter. The conventional molybdenum filter is used to investigate abnormalities of the soft tissues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree